-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Orbital Cellulitis as a Complication of Acute Rhinosinusitis – our Experience with Treatment in Adult Patients
Orbitocelulitida jako komplikace akutní rhinosinusitidy – naše zkušenosti s léčbou u dospělých pacientů
Cíl:
Studie má ukázat na závažnost orbitocelulitidy, která přestože je popisována Chandlerem jako počáteční stadium orbitální komplikace rhinosinusitidy může probíhat dramaticky a končit i letálně, a to zejména při současném výskytu nitrolební komplikace.Materiál a metody:
V retrospektivní studii je prezentován soubor 18 pacientů operovaných v letech 1999 – 2014. Soubor pacientů tvořilo pět žen, 13 mužů, ve věku v rozmezí od 21 do 75 let, průměrný věk 50 let. Orbitocelulitida se vyskytla vpravo u osmi pacientů, vlevo u osmi pacientů, a u dvou pacientů oboustranně.Výsledky:
Celkem bylo provedeno u 18 pacientů 24 operací. Tyto operace byly provedeny zevním přístupem 12krát (50 %), endoskopické přístup byl použit jednou (4 %). Kombinovaným přístupem jsme postupovali 11krát (46 %). CT navigační systém byl použit ve dvou případech (8 %). Komplikace, které se objevily jako důsledek orbitocelulitidy po operaci: jeden pacient (6 %) s dekompenzovaným diabetes mellitus a současné intrakraniální komplikací zemřel, trvalá diplopie byla pozorována u dvou pacientů (11 %).Závěr:
Orbitocelulitida je závažný stav, často vzniklý jako komplikace akutní rhinosinusitidy. Neléčená orbitocelulitida je spojena s vysokým rizikem komplikací a je potenciálně letální. V léčbě orbitocelulitidy je indikována chirurgická léčba a intravenózní terapie antibiotiky.Klíčová slova:
orbitocelulitida – onemocnění orbity – rhinosinusitida – chirurgická léčba
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors: R. Holý 1; D. Kovář 1
; P. Fundová 1; T. Belšan 2; T. Filipovský 1; J. Astl 1,3
Authors place of work: Department of Otorhinolaryngology and Maxillofacial Surgery, rd Faculty of Medicine of Charles University and Military University Hospital Prague 1; Department of Radiology, Military University Hospital Prague 2; Department of Otorhinolaryngology and Head and Neck Surgery, 1st Faculty of Medicine of Charles University and Motol University Hospital Prague 3
Published in the journal: Cesk Slov Neurol N 2016; 79/112(6): 698-702
Category: Krátké sdělení
Summary
Aim:
The study seeks to demonstrate seriousness of orbital cellulitis that, although described by Chandler as an initial stage of orbital complications of rhinosinusitis, can have serious outcome that can be fatal, particularly when it is associated with intracranial complications.Material and methods:
This retrospective study presents a cohort of patients who underwent surgery between 1999 and 2014. We analysed a group comprising 18 adult patients, five women and 13 men, all aged between 21 and 75 years (median age 50 years). Orbital cellulitis was right-sided in eight patients, left-sided in eight patients and bilateral in two.Results:
In total, 24 surgeries were performed. External approach was used in 12 cases (50%), endscopic approach in one case (4%) and combined approach in 11 cases (46%). Computer-assisted surgery was used in two cases (8%). Complications following surgery: one patient (6%) with decompensated diabetes mellitus and concurrent intracranial complications died and diplopia was permanent in two patients (11%).Conclusion:
Orbital cellulitis is a severe condition often occuring as a complication of acute rhinosinusitis. Untreated orbital cellulitis is associated with high risk complications and can be potentially fatal. Surgical and antibiotic treatment is preferred to manage orbital cellulitis.Key words:
orbital cellulitis – orbital diseases – rhinosinusitis – surgical proceduresIntroduction
Orbital cellulitis is considered to be potentially serious complication of rhinosinusitis. It is a severe, potentially life-threatening condition. Infection can spread from the sinuses to orbit per continuitatem via blood vessels, lymphatic vessels, along nerves or through anatomical defects (post-traumatic, post-operative and congenital) and also through haematogenous metastatic dissemination [1 – 4].
According to Chandler’s classification, gradual development of an infection into orbital complication occurs in several stages: I. periorbital cellulitis (preseptal swelling), II. orbital cellulitis, III. subperiosteal abscess, IV. phlegmon and orbital abscess, V. thrombosis and thrombosis sinus cavernosus. In addition, intracranial complications and cavernous sinus thrombosis can occasionally occur [1 – 7]. Orbital cellulitis is an acute infection of the tissue immediately surrounding the eye, including the eyelids, eyebrow, and the cheek. The disease is more common in children up to the age of 7. It is a diffuse inflammation process originating mostly from sinusitis, especially ethmoid sinusitis [1 – 7].
Orbital cellulitis is a dangerous infection with potentially serious complications. Orbital cellulitis with concurrent intracranial complications and blindness is the most severe complication. Chandler did not consider another potential complication, sepsis that is particularly dangerous in immunocompromised patients [1 – 4,6 – 10].
The following etiologic agents are described in literature: Haemophillus influenzae, Streptococcus pneumoniae, Staphylococcus aureus, Pneumococcus, anaerobi (Fusobacterium) and fungi in immunocompromised patients and in patients with severe diabetes mellitus (DM) [1,4,6,8 – 12].
Clinical signs of orbital cellulitis are:
- Main: eyelid swelling, erythema and chemosis, impaired visual acuity, impairment of colour perception, impairment of extraocular muscles, diplopia, tenderness, protrusion or eyeball deviation.
- Supplementary: rhinosinusitis, headache, fever, alteration of general condition.
Diagnostic criteria:
- Computed tomography (CT) and magnetic resonance (MRI) finding of diffuse orbital swelling commonly associated with sinusitis [1,3,4,7 – 14].
- Ocular signs.
- Febrile state, general health status deterioration.
- Blood tests with elevated markers of inflammation (leukocytes, CRP, procalcitonin).
Diagnostic process should be performed urgently under hospitalisation and should include clinical and laboratory examinations, nasal endoscopy, ophthalmological examination and, in particular, CT scan. If there is a suspicion of intracranial infection spreading, brain MRI is performed [1,2,4,7,14 – 18].
Early diagnosis is crucial for successful treatment. To achieve this, we use a scoring system described in Tab. 1. If the score reaches 5 points or above in adults, surgical treatment should promptly be performed. Conservative treatment is preferred in children under the age of 7 since the sinuses are not yet fully developed [1 – 4,6,19].
Tab. 1. Scoring system for treatment of orbital cellulitis decision. 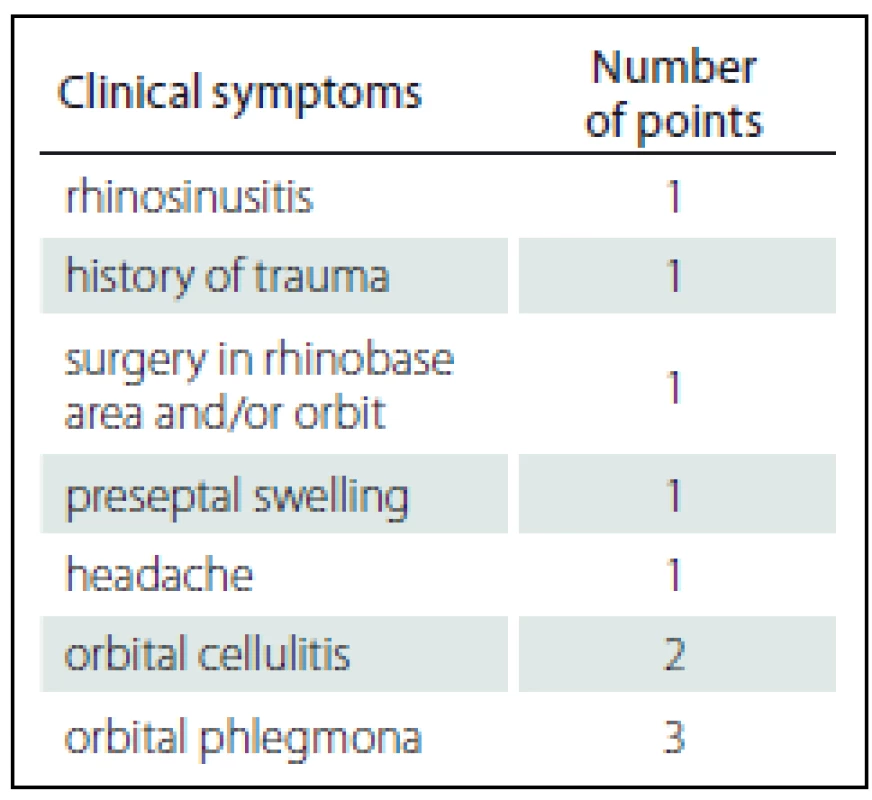
Surgical drainage of the predisposingrhinosinusitis, orbital decompression by longitudinal incisions of periorbita and concurrent parenteral broad-spectrum antibiotics are considered to be the essential treatment of orbital cellulitis in adults.
At present, surgical drainage is preferably performed via a combined or external or endoscopic approach, with or without CT navigation [20]. The Jansen Ritter procedure and Killian procedure are utilised for external approach. During the last 20 years, our department more frequently employed the endoscopic approach. Open approaches are demanding with respect to surgical skills and erudition of the surgeon [2,4,6,7,13 – 17].
Material and methods
A cohort of adult patients with orbital cellulitis (as a complication of acute rhinosinusitis) surgically treated between 1999 – 2014 was evaluated in this retrospective study. Allpatients underwent a surgery at the Department of ENT and Maxilofacial Surgery of the 3rd Medical Faculty, Charles University and the Military University Hospital in Prague.In total, 18 patients were treated. Ages, genders, treatment modalities, surgical procedures, postsurgical mortality and treatment outcomes were reviewed. Ophthalmological records of all patients were alsoevaluated.
Results
Data of the 18 treated patients were analysed and are shown in Tab. 2. During the 15-year period between 1999 and 2014, a total of 2,458 patients underwent surgery associated with a paranasal sinuses disorder at our department. Endoscopic treatment (FESS) was utilised in 2,239 patients (91%) and external approach was preferred in 219 patients (9%). On average, 164 patients were operated on per year; 149 with endoscopic approach (FESS) and 15 using external approach. The 18 patients undergoing surgery due to orbital cellulitis represent 0.7% of all patients in whom paranasal sinuses were surgically managed.
Tab. 2. Patients with orbital cellulitis – data analysis (n = 18). 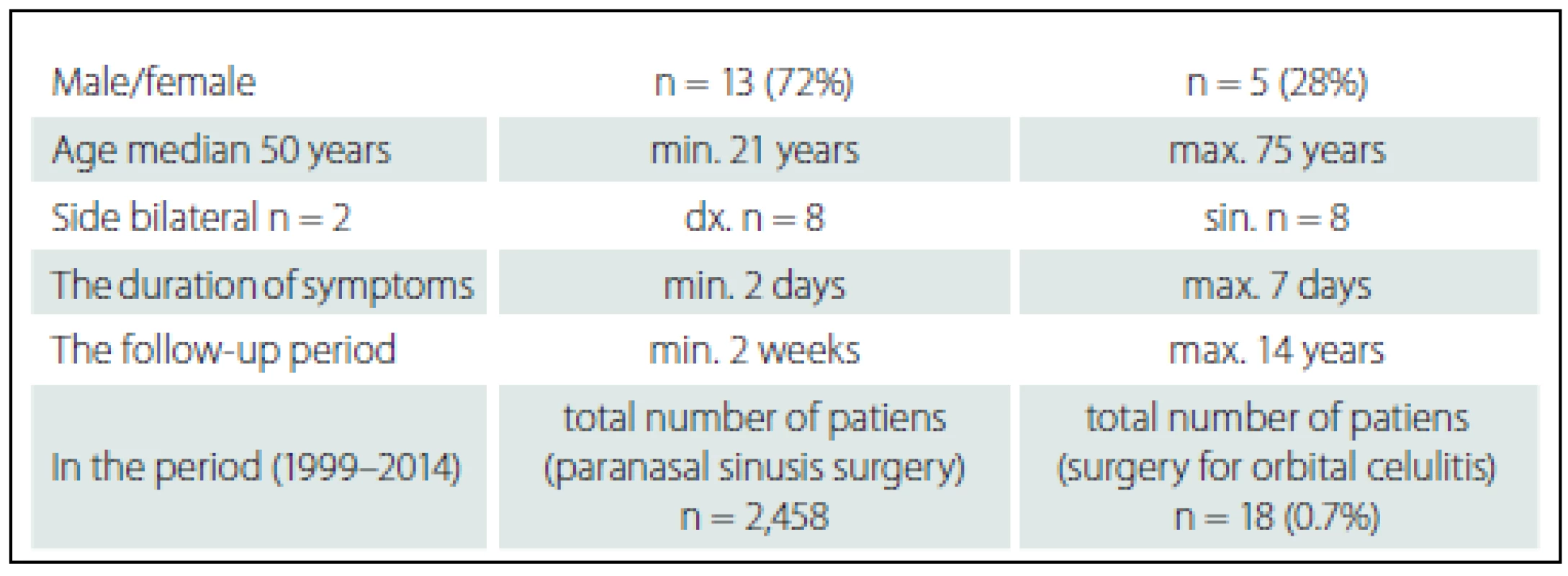
We used a scoring system to make a decision about the treatment of orbital cellulitis. (Tab. 1). All patients received surgical treatment because their symptoms reached the score of 5 points or above.
One patient (6%) with decompensated DM and concurrent intracranial complications (cerebritis) died. Two patients (11%) were addicted to drugs.
In total, 24 operations were performed. All patients were operated on within 24 hours of hospital admission. Four patients underwent repeated surgery (two operations). CT navigation was used in two cases (8%). We performed 11 operations (46%) with combined approach, both endoscopically and externally (Jansen Ritter procedure). External approach was used in 12 cases (50%) with the Jansen Ritter procedure in 11 patients and the Killian procedure in one; endoscopic approach was used once only (4%) (Tab. 3).
Tab. 3. Surgical treatment of orbital cellulitis (n = 24 surgeries). 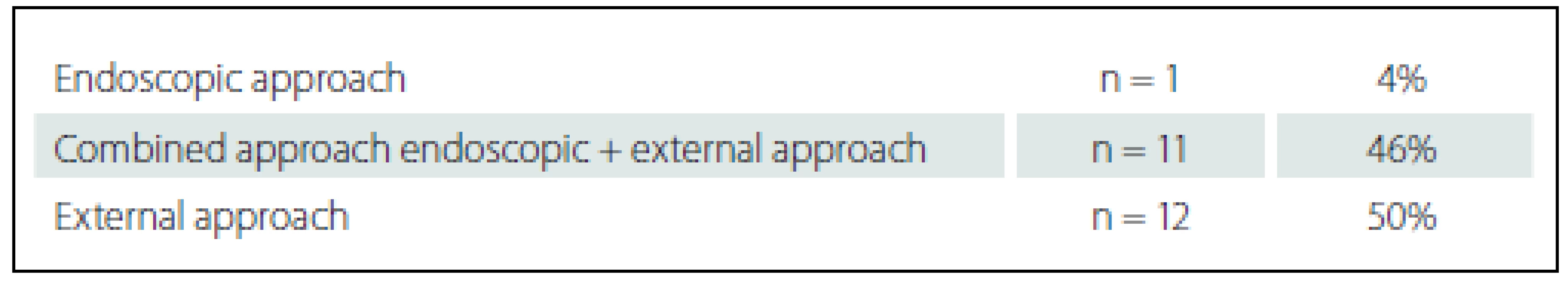
Postsurgical eye finding: amaurosis 0 (0%), persisting diplopia in two patients (11%), normal postsurgical eye examination in 15 patients (83%) (Tab. 4).
Tab. 4. Orbital cellulitis – mortality and postsurgical eye finding (n = 18 patients). 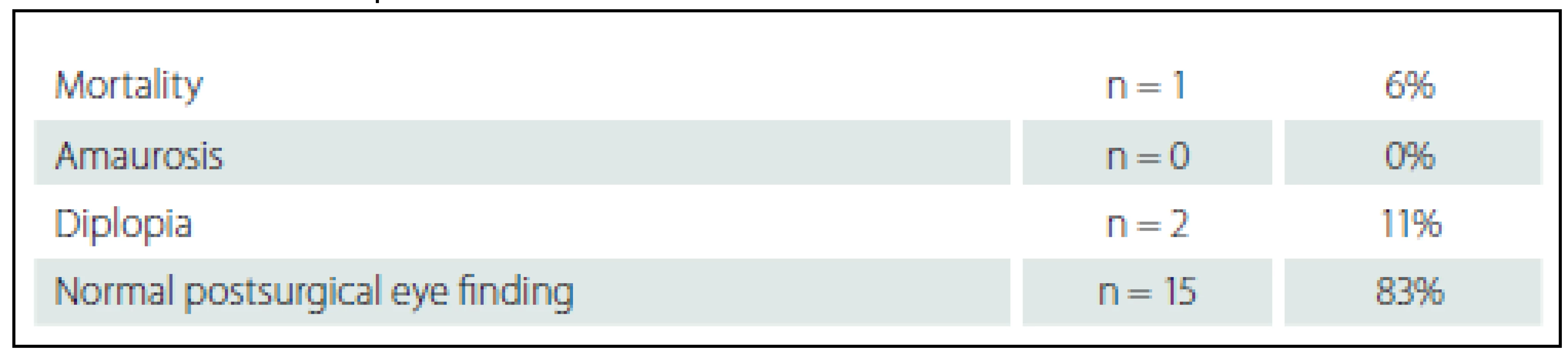
Case report
A 75-year-old diabetic male, afebrile, with a discrete finding of preseptal cellulitis on the left, lasting for five days. There were no signs of rhinosinusitis endoscopically during the initial investigation. Sinus CT scan revealed partial mucosal thickening of the left ethmoids only, without signs of orbital cellulitis. Oral antibiotic treatment was initiated. Conservative treatment approach was selected. On the next day, the patient was taken to hospital by emergency ambulance in poor overall condition with substantial progress of his illness, signs of orbital cellulitis on the left side. He was febrile and his DM was decompensated (Fig. 1). The patient was admitted to hospital and parenteral broadspectrum antibiotic treatment (amoxicillin + clavulanate) was initiated. Combined surgical approach (endoscopic and external; Jansen-Ritter procedure) was urgently performed. MRI showed cerebritis as a new concurrent intracranial complication in progress (CRP 285, procalcitonin 0,527). Thus, the patient was treated in an intensive care unit in cooperation with anaesthesiologists and neurosurgeons (new parenteral antibiotics ceftriaxon + metronidazol) (Fig. 2, 3). Bacterial and mycological cultivation showed negative nasal swab, negative sputum, and negative cerebrospinal fluid. Despite intensive treatment (artificial pulmonary ventilation), the patient died of fulminant devastating neuroinfection on the fourth day after the surgery. The autopsy found orbitocellulitis phlegmonosa l. sin. et sinusitis purulenta sinus frontalis et ethmoidalis l. sin., encephalitis septica gravis, abscessus aliquot telencephali et trunci cerebri.
Fig. 1. A 75-year-old diabetic male with left side orbital cellulitis, initial CT (A1, A2) and the next day CT (B1, B2) demonstrates left eyelids swelling and was a partial mucosal thickening of the left ethmoids. 
Frontal sinuses are ventilated. Oedema development in the left frontal lobe. Fig. 2. A 75-year-old diabetic male with left side orbital cellulitis, MRI scans first day after surgery – drain in left ethmoid and frontal sinuses, orbital oedema on the left side. 
Fig. 3. A 75-year-old diabetic male with left side orbital cellulitis, MRI first day after surgery – extensive cerebritis of the left frontal lobe. 
Discussion
Orbital cellulitis with concurrent intracranial complications is a life-threatening disease [6]. Management of patients with orbital cellulitis requires close cooperation between an otolaryngologist, ophthalmologist, infectious disease specialist and neurosurgeon [20]. Clinically, these patients have eyelid oedema, proptosis, chemosis and orbital pain [21]. In severe cases, ocular motility may be limited and visual acuity may be impaired. Significant decrease in visual acuity is considered to be an indication for immediate surgical intervention but visual monitoring is difficult in very small children [19 – 21].
Hansen et al. reported mortality of 6% in their study. All patients who died had intracranial complications. We identified similar results in our cohort with mortality of 6%. One patient who died had decompensation of diabetes and intracranial complications. The urgency for prompt surgical treatment is much higher in immunocompromised patients. Orbital cellulitis is associated with a risk of death in 5 to 10% of patients [4,7].
Patt et al. suggested that amaurosis from orbital complications still occurs and is associated with DM [22]. Because of the correlation between this serious complication and DM, these patients deserve close follow-up and immediate surgical drainage [23].
Although CT is very useful in the diagnosis of orbital cellulitis, imaging must be conducted in association with clinical findings. Possible inaccuracy in CT diagnosis could be related to interpretation errors, time lag between a CT scan and progression of symptoms, or inadequate CT slice widths or resolution limits [6,24 – 27]. MRI is a useful imaging modality in patients suspected of developing intracranial complications [6,24].
Ketenci et al. analysed 36 patients with rhinosinusitis complicated with subperiosteal orbital abscesses (SPOA) in a retrospective study. They used medical management as the only treatment modality in nine patients, seven of which were under the age of 10 with small medial SPOA. Of the 13 with medial SPOA, trans-nasal endoscopic approach was performed in 10 and external approach in three to drain the abscess. As for the 12 patients with superior SPOA, eight were treated via combined approach and four via external approach. Total loss of vision developed in two adults with DM. One patient with superior SPOA died due to frontal lobe abscess. Young children with small medial SPOA without significant ocular signs may be successfully managed medically. Surgical drainage is indicated in non-medial abscesses, large medial abscesses with severe visual loss and with insufficient response to medical management. The risk of blindness from SPOA is higher in patients with DM [6].
Czech authors Kastner et al. published a case of a patient with odontogenic maxillary sinusitis combined with an orbital complication – preseptal inflammatory oedema was treated using the endoscopic approach and was followed by meningitis and subdural abscess [4]. The patient survived with hemiparesis as the only sequela.
Kastner et al. mention concomitant occurrence of orbital and intracranial complications in 20% of patients with orbital complications. The same coincidence occurred in one patient (6%) in our cohort. At present, surgical approaches to treatment of orbital cellulitis are not restricted to external procedures since they comprise both external and endoscopic procedures whilst incorporating CT navigation [4].
We preferred combined endoscopic and external approaches in our patients due to higher occurrence of pansinusitis and ostitis in the medial and upper walls of the orbit. Our analysis of data from previous 15 years showed that surgical approaches have mainly been alternated during the last fewyears. Our long-term experience with the combined approach and its good treatment results support our decision to maintain this more radical method of surgery.
Persisting diplopia in two of our patients was present in extreme eye positions only while full mobility of the eye bulbs was maintained. We attribute this diplopia to the relative enophtalmos that developed following partial removal of the lamina papyracea and ablation of the base of the frontal sinus.
Summary and conclusions
Orbital cellulitis is often presented as a complication of rhinosinusitis of adult age. It is a fast developing severe disease that could be diagnosed too late. The risk of death rises significantly when orbital cellulitis is associated with concurrent intracranial complications. Patients with DM must be closely monitored to minimize the risk of severe complications. Early diagnosis is crucial for successful treatment. To facilitate successful treatment, we use a scoring system. If the score reaches 5 points or above, surgical treatment in adults should be performed promptly. Conservative treatment is preferred in children under the age of 7 as the sinuses are not fully developed. Treatment of fully developed orbital cellulitis always involves surgical intervention supported with antibiotics. For surgical management we use either a combined or external approach. Serious complications are intracranial, amaurosis and death. Multidisciplinary approach is crucial in patients with complications.
This research was supported by the Ministry of Defence MO 1012 research project, Czech Republic.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Richard Holý MD, PhD
Department of Otorhinolaryngology and Maxillofacial Surgery
3rd Faculty of Medicine of Charles University
Military University Hospital Prague
U Vojenské nemocnice 1200
169 02 Praha
e-mail: Richard.Holy@uvn.cz
Accepted for review: 1. 10. 2015
Accepted for print: 2. 3. 2016
Zdroje
1. Wald ER. Periorbital and orbital infections. In: Long SS (ed). Principles and practice of pediatric infectious diseases. 3rd ed. Philadelphia, Pa: Elsevier Churchill Livingstone 2008 : 1236 – 8.
2. Charvát F, Markalous B. Zobrazení hlavy, paranazální dutiny, lební baze a obličejová část. II. upravené a rozšířené vydání. Praha: Triton 2006 : 253 – 6.
3. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope 1970;80(9):1414 – 28.
4. Kastner J, Taudy M, Lisy J, et al. Orbital and intracranial complications after acute rhinosinusitis. Rhinology 2010;48(4):457 – 61. doi: 10.4193/ Rhino09.130.
5. Fokkens WJ, Lund VJ, Mullol J, et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinology 2012;50(1):1 – 12. doi: 10.4193/ Rhino50E2.
6. Ketenci I, Unlü Y, Vural A, et al. Approaches to subperiosteal orbital abscesses. Eur Arch Otorhinolaryngol 2013;270(4):1317 – 27. doi: 10.1007/ s00405-012-2198-x.
7. Hansen FS, Hoffmans R, Georgalas C, et al. Complications of acute rhinosinusitis in The Netherlands. Fam Pract 2012;29(2):147 – 53. doi: 10.1093/ fampra/ cmr062.
8. Lang EE, Curran AJ, Patil N, et al. Intracranial complications of acute frontal sinusitis. Clin Otolaryngol 2001;26(6):452 – 7.
9. Clayman GL, Adams GL, Paugh DR, et al. Intracranial complications of paranasal sinusitis: a combined institutional review. Laryngoscope 1991;101(3):234 – 9.
10. Mortimore S, Wormald PJ. Management of acute complicated sinusitis: a 5-year review. Otolaryngol Head Neck Surg 1999;121(5):639 – 42.
11. Lerner DN, Choi SS, Zalzal GH, et al. Intracranial complications of sinusitis in childhood. Ann Otol Rhinol Laryngol 1995;104(1):288 – 93.
12. Gallagher RM, Gross CW, Phillips CD. Suppurative intracranial complications of sinusitis. Laryngoscope 1998;108(1):1635 – 42.
13. Herrmann BW, Forsen JW. Simultaneous intracranial and orbital complications of acute rhinosinusitis in children. Int J Pediatr Otorhinolaryngol 2004;68(5):619 – 25.
14. Ferguson MP, McNab AA. Current treatment and outcome in orbital cellulitis. Aust NZ J Ophthalmol 1999;27(6):375 – 9.
15. Nwaorgu OG, Awobem JF, Onakoya PA, et al. Orbital cellulitis complicating sinusitis: a 15-year review. Nigerian J Surg Res 2004;6 : 14 – 6.
16. Tshifularo M, Monama GM. Complications of inflammatory sinusitis in children: institutional review. SA Fam Pract 2006;48(10):16.
17. Singh B, Van Dellen J, Ramjettan S, et al. Sinogenic intracranial complications. J Laryngol Otol 1995;109(10):945 – 50.
18. Chaudhry IA, Shamsi FA, Elzaridi E, et al. Outcome of treated orbital cellulitis in a tertiary eye care center in the middle East. Ophthalmology 2007;114(2):345 – 54.
19. Vláčil O, Kincl J. Akutní orbitocelulitida – diagnostika a léčba. Pediatr Praxi 2011;12(5):304 – 5.
20. Fakhri S, Pereira K. Endoscopic management of orbital abscesses. Otolaryngol Clin North Am 2006;39(5):1037 – 47.
21. Epstein VA, Kern RC. Invasive fungal sinusitis and complications of rhinosinusitis. Otolaryngol Clin North Am 2008;41(3):497 – 524. doi: 10.1016/ j.otc.2008.01.001.
22. Patt BS, Manning SC. Blindness resulting from orbital complications of sinusitis. Otolaryngol Head Neck Surg 1991;104(6):789 – 95.
23. Weber AL, Mikulis DK. Inflammatory disorders of the paraorbital sinuses and their complications. Radiol Clin North Am 1987;25(3):615 – 30.
24. Manning SC. Endoscopic management of medial subperiosteal orbital abscess. Arch Otolaryngol Head Neck Surg 1993;119(7):789 – 91.
25. Feder HM jr, Cates KL, Cementina AM. Pott puffy tumor: a serious occult infection. Pediatrics 1987;79(4):625 – 9.
26. Bradley PJ, Manning KP, Shaw MD. Brain abscess secondary to paranasal sinusitis. J Laryngol Otol 1984;98(7):719 – 25.
27. Lund VJ. The complications of sinusitis. In: Ka G (ed). Scott Brown’s otolaryngology. Oxford: Butterworth-Heinemann 1997 : 1 – 11.
Štítky
Detská neurológia Neurochirurgia Neurológia
Článok vyšiel v časopiseČeská a slovenská neurologie a neurochirurgie
Najčítanejšie tento týždeň
2016 Číslo 6- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Neuromultivit v terapii neuropatií, neuritid a neuralgií u dospělých pacientů
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
-
Všetky články tohto čísla
- Úvodník
- Depression in Selected Neurological Disorders
- Chirurgická léčba arteriovenózní malformace
- Radiochirurgická léčba arteriovenózní malformace mozku
- Endovaskulární léčba arteriovenózní malformace
- Terapie cerebrálních arteriovenózních malformací – observace
-
Komentář ke kontroverzím
Kontroverze arteriovenózních malformací - Pain-related Fear in Chronic Low Back Pain Patients
- The Use of Transcranial Sonography at Neuro-psychiatry Interface
- Introduction to Neuromuscular Ultrasound
- Proposed MRI Safety Monitoring of Patients with Multiple Sclerosis Treated with Natalizumab
- Do not Test but POBAV (ENTERTAIN) – Written Intentional Nam ing of Pictures and their Recall as a Brief Cognitive Test
- Preoperative Visual Memory Performance as a Predictive Factor of Cognitive Changes after Deep Brain Stimulation of Subthalamic Nucleus in Parkinson‘s Disease
- Executive Function Deficits in Patients with Blepharospasm
- The Importance of Thermal Threshold Testing in Detecting of Small Fiber Neuropathy in Type 1 Diabetes Mellitus
- Orbital Cellulitis as a Complication of Acute Rhinosinusitis – our Experience with Treatment in Adult Patients
- A Case of Severe Progres sion of HIV-1 Meningoencephalitis and Lues Secundaria
- Autoimmune Encephalitis – Case Reports
- Spinal Gossypiboma 20 years after Lumbar Discectomy – a Case Report
- Anterior Cervical Osteophytes Causing Dysphagia and Dyspnea – Two Case Reports
- Surgical Treatment of Extensive Fibrous Dysplasia in the Craniofacial Region – a Case Report
- Webové okénko
-
Analýza dat v neurologii
LX. Analýza trendu ve vztahu kategoriálních znaků - Recenze knih
- Nepodceňujte oportunní infekce při léčbě roztroušené sklerózy
- Jak to bylo na neurochirurgii ve Střešovicích před 50 lety?
- Česká a slovenská neurologie a neurochirurgie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Anterior Cervical Osteophytes Causing Dysphagia and Dyspnea – Two Case Reports
- Depression in Selected Neurological Disorders
- Autoimmune Encephalitis – Case Reports
- Surgical Treatment of Extensive Fibrous Dysplasia in the Craniofacial Region – a Case Report
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



