-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
preLekára.sk / Odborné časopisy / Česká a slovenská neurologie a neurochirurgie / 2017 - Supplementum 1Differential Diagnosis in Pressure Ulcers and Medical Devices
Diferenciální diagnostika dekubitů a dekubity vznikající v souvislosti s přístrojovou technikou
Východiska:
Dekubity jsou považovány za nežádoucí událost, představují výzvu pro zdravotnické pracovníky a instituce.Cíl:
Zhodnotit prevalenci a incidenci dekubitů na pracovišti intenzivní péče a obtíže při klasifikaci dekubitů u kriticky nemocných z pohledu všeobecných sester.Soubor a metody:
Retrospektivní kohortová analýza elektronických zdravotnických záznamů pacientů (2012 – 2013). Dotazník k hodnocení bariér klasifikace dekubitů u ošetřujícího personálu.Výsledky:
Epidemiologická studie (n = 600) záznamů a diferenciální diagnostická studie u 27 všeobecných sester. U 98 pacientů byl záznam s alespoň jedním dekubitem za hospitalizace (prevalence 16,3 %). Z nich u 40,8 % dekubitus při přijetí, u 59,2 % vznikl dekubitus po 24 hod od přijetí (n = 58), incidence 11,4 %. Zjištěná kategorizace dekubitů: nejčastější druhý stupeň (36,1 %), následně čtvrtý (35,4 %), první (13,1 %) a třetí stupeň (10,8 %). Uváděné bariéry diferenciální diagnostiky: 77,7 % hodnocení dekubitů u pacientů s periferním arteriálním onemocněním; 92,5 % hodnocení prvního stupně na tmavé kůži; 81,5 % charakteristika dekubitů na sliznici; 40,7 % v souvislosti se zdravotnickými prostředky. Vzdělávání jako cestu ovlivnění subjektivity hodnocení uvedla většina všeobecných sester (96,3 %).Závěr:
Prevence dekubitů v intenzivní péči vyžaduje speciální pozornost. Incidence dekubitů je vyšší v souvislosti se zdravotnickými prostředky. Prevence zahrnuje více strategií (vzdělávání a sdílení zkušeností) k redukci subjektivizace diferenciální diagnostiky.Klíčová slova:
incidence – prevalence – ošetřovatelské hodnocení – intenzivní péče – Portugalsko – dekubitus – hodnocení rizika
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors: P. Alves 1–3; T. Eberhardt 4; R. Soares 4; M. Pinto 5; C. Pinto 5; L. Vales 3,5; J. Morais 6; I. Oliveira 2
Authors place of work: Centre for Interdisciplinary Research in Health, Catholic University of Portugal Porto, Portugal 1; Catholic University of Portugal – Institute of Health Sciences, Porto Portugal 2; Portuguese Wound Management Association APTFeridas, Porto, Portugal 3; Universidade Federal de Santa Maria Santa Maria, Brazil 4; Centro Hospitalar São João, Serviço Urgência Adultos, São João, Portugal 5; Centro Hospitalar Vila Nova de Gaia/ Espinho, Vila Nova de Gaia, Portugal 6
Published in the journal: Cesk Slov Neurol N 2017; 80(Supplementum 1): 29-35
Category: Původní práce
doi: https://doi.org/10.14735/amcsnn2017S29Summary
Background:
Pressure ulcers (PU) are considered to an adverse event and constitute a constant challenge for all health professionals and institutions.Aim:
Study the prevalence and incidence of PU in a intensive care unit (ICU) and the difficulties of classification and characterization of the lesions in critical ill patients.Materials and methods:
Retrospective cohort analysis of electronic health record database from adult patients admitted to a ICU during 2012/ 1013. Barriers/ difficulty’s to classification of PUs were also studied in the nursing staff.Results:
Epidemiologic sample study included 600 participants, and differential diagnoses study 27 nurses. The episodes in the study period (n = 600), 98 were identified with at least one PU present during hospitalization period, corresponding to a prevalence rate of 16.3%. The remaining 502 had no PU recording at entry or during hospitalization, 98 patients who were identified with PU, 40.8% presented it upon admission, and 59.2% developed ulceration in the service after 24 hours of admission (n = 58), which resulted in an incidence rate of 11.4%. The categorization of the PU ulcers identified in the present study, the most prevalent was category II (36,1%), followed by IV (35,4%), then I (13.1%) and III (10.8%). Regarding barriers of the differential diagnosis, 77.7% reported difficulty in evaluating PU in patients with peripheral arterial disease; 92.5% referred difficulty in evaluating Category I in dark skin; 81.5% referred subjectivity in the characterization in the mucosa; 40.7% reported difficulty PU associated to medical devices; 96.3% considered essential training as a way to reduce subjectivity.Conclusion:
Extra attention needs to be taken to prevent PU in ICU. The incidence of PU is higher if associated with a medical device, Staff must adopt multiple strategies to prevent it. More education and sharing experiences is needed to reduce the subjectivity of differential diagnosis in PU.Key words:
incidence – prevalence – nursing assessment – intensive care – Portugal – pressure ulcer – risk assessmentIntroduction
Pressure ulcers (PUs) continue to be a contest worldwide [1 – 3]. PUs are considered to be an adverse event and constitute a constant challenge for all health professionals and institutions, both for human and material resources, and for the pain and suffering caused to patients and their families. In fact, the development of PUs is complex and multifactorial [4] and nursing staff needs to manage several PU risk factors [5,6] in order to prevent PU development.
Scientific evidence has shown that PUs are not only the responsibility of the nursing team, but of an entire multidisciplinary team, even with current knowledge of its aetiology, the incidence and prevalence are still very high.
It can be seen that the epidemiology of PUs varies greatly between countries, the area where the patient is hospitalized (nursing homes, hospital admissions, intensive care, etc.) and the method of data collection.
The use of a rigorous methodological design (with methods to measure the consistent variables, including the clear definition of the study population, the confidence interval and skin evaluations performed by two trained auditors), the comparison of organizational data between performance areas. The incidence of PU, the description of the most frequent anatomical locations of PU, the reference to whether or not to include category one of PUs in the study and the inclusion PUs developed in the mucous membranes (lips, nose, genitals, etc.) without assigning them category. It is crucial to obtain more reliable and internationally comparable data to facilitate the study of the problem in the future.
The prevalence of PUs in hospitals is 17.4% in medicine, 7.1% in surgery, 15.3% in emergency and 16.6% in intensive care unit (ICU). In long-stay units in mainland Portugal, the estimated prevalence was 23%, with lot of differences between the districts [7].
Internationally, in the most recent study, Pokorna et al. [8] presented reported prevalence of PU in the Czech Republic of 0.3% in a total of 46,224 patients identified with the diagnosis of PU. For ICU, studies have reported rates of incidence of PUs in the USA between 5.2 and 45%, with prevalence rates between 22 and 28.7%, and, on the other hand, studies in ICUs in developing countries such as Indonesia, report an incidence of approximately 33.3% [9].
In the review study conducted by Cuddigan [10], which analyses the prevalence and incidence data on ICU worldwide, data were obtained with a great deal of variability, and part of the data is summarized in the Tab. 1.
Tab. 1. Prevalence and incidence reported in international studies (adopted from [10]). ![Prevalence and incidence reported in international studies (adopted from [10]).](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image/ee92ee09c279fd92cf48178e52d8a945.png)
As can be seen from the systematized data in the Tab. 1, there is a great variability of values. This may be related to the possible inclusion of data on category one PUs, as well as characteristics of the ICU considered in the study, namely units with exclusive inclusion of surgical patients.
The correct classification of the ulcers allows to identify the severity of the ulcers and to evaluate their aggravation, if this occurs, and the evaluation of PUs should include the size, the wound bed, present exudate (which will allow classification), pain and the state of the surrounding skin (to manage analgesia and prevent area worsening), and the anatomical location of the lesion is also important [11].
Correct diagnosis and classification of these lesions is essential, promoting quality of care and patient safety [12]. Injuries such as skin breakdowns, moisture lesions, incontinence-associated dermatitis and ischemic lesions [13], are poorly defined and referred to as PUs.
The main difficulties described by several authors on the classification/ categorization of ulcers are the evaluation of erythema, bleachable or non-bleachable. The distinction between PU and moisture injury and the differentiation of categories II and III [11,14 – 16].
The evaluation of erythema, whether bleached or not bleached, in black individuals is hampered by the impossibility of evaluating a category one related bleaching of tissues and, in order to reduce this error, other elements that could be evaluated as discoloration of skin, presence of heat, oedema, pain and/or hardening that differentiate the existence or not of a PU [1]. According to Moore [17], citing the study by Barczak form the seventeen’s, reported that black individuals had more severe PUs mainly due to the difficulty of identification, in category one and, consequently, absence of performance.
Incontinent Associated Dermatitis (IAD) is often confused and mixed with PUs. In its aetiology, the predominant factor is humidity and not pressure [18], as these lesions appear in individuals with a clinical history of excessive humidity (urinary and/or faecal incontinence, wound drainage, vomiting and/ or sweating) and is in a place where the humidity is excessive. Usually found outside the bony prominences, they are superficial lesions, with shallow and poorly defined borders. It is also characteristic of this type of lesions, not having devitalized or necrotic tissue [15]. A correct distinction between PUs and moisture injuries is important because the preventive attitudes to be taken are different [15]. Regarding categorization II or III of PUs, the purpose is to identify the deepest affected tissue [19], thus, the ulcer will be categorized according to the worst level of tissue injury present, and will remain in the worst category throughout treatment and evolution [17].
The main differentiation between the two categories is based on the type of tissue reached, defined as partial loss of skin, category II PUs or superficial ulcer, involving the epidermis and/or dermis, the category III and IV of PU involve all layers of fabric. The observation of the different injured tissues has been shown to be a difficult to health professionals [15].
Incorrect classification or diagnosis may result in a misalignment of prevention and/ or treatment strategies. It is essential to use the patient‘s integral observation, pondering signs and symptoms that help the health professional, in the differential diagnosis of PU. There are several tools to support the diagnostic decision-making, where it is possible to identify symptoms and signs that will support the correct diagnosis of PU, compared to skin breakdowns, IAD among others [15,20].
Research in this area, with a correct diagnosis of the epidemiological situation and identification of the determinants of the development of ulcers in the critically ill person, can help to validate and increase knowledge on the subject and ultimately improve scientific knowledge.
Aim
This study had two objectives: to study the prevalence and incidence of PUs in an intensive care unit and the difficulties of classification and characterization of the lesions in critical ill patients from nurses point of view.
Materials and methods
Study design
This study has two different steps. The epidemiologic study was designed as a retrospective cohort analysis of electronic health record database from adult patients admitted to a polyvalent Intensive Care Unit of a Central Portuguese hospital. The questionnaire study was designed to the nursing staff of the same unit.
Setting
The survey was performed in a polyvalent ICU of a Central Portuguese hospital. All data were extracted from electronic health record database with the collaboration of Hospital Informatics and Systems Analysis Service. The period under analysis was from 1st June 2012 to 31st May 2013. The questionnaire was applied to all nurses of the ICU during the month of January 2015.
Participants
The research was implemented after Hospital Council Board and Ethics Committee approval (Reference Number 149/ 2014).
The study was divided into two phases: the first was a random, probabilistic sample (including patients admitted without any selection), with a sequential character, including all patients admitted to a Polyvalent Intensive Care Unit of a hospital in the north of Portugal between the period from 1st June 2012 to 31st May 2013 (1 year).
The period studied was chosen so that access to the computer data needed for the analysis was possible, since it was conditioned by the introduction of the current software in the service, which only occurred in September 2011, but whose configuration and optimization only took place during the next year. By obtaining data after May 2012, these would already be reliable and the information obtained adequate to give robustness to the study.
The second stage is related to the differential diagnosis between PUs and other lesions, namely incontinence-associated, intertrigo (not only diaper rash) and cutaneous dermatitis. A questionnaire was carried out to the nursing team (N = 30) to identify barriers and difficulties in the classification and categorization of PUs and other skin lesions.
Variables
The data were extracted from electronic health record database and included the following.
Variables divided in categories:
- Socio-demographics: age, gender.
- Clinical information: Type of admission (elective or urgent surgery, medical or trauma); clinical diagnosis of admission; length of hospitalization; APACHE II value and probability of death predicted at admission; outcome (high or deceased).
- Braden Scale Risk Assessment: value resulting from the Braden scale and its subscales at admission. First PU risk assessment, all skin and tissue assessment records.
- PUs present: Number of PUs identified in the clinical process, categories, location, diagnosis of nursing described in the identification of PUs (to obtain category and location); date of creation of nursing diagnoses and attitudes related to PUs.
From the nurse‘s questionnaire, differential diagnosis of PU was evaluated: associated factors; diagnostic criteria; subjectivity of the evaluation; mucosal PUs; medical devices.
Data sources/ measurement
Data collection were performed by a registered nurse and/or a clinical nurse specialist at admission in inpatient setting and were documented in the patient electronic health record, following national and international guidelines [1] the pressure ulcer risk assessment (Portuguese version of Braden Scale) and the skin and tissue integrity assessment. The risk assessment and the skin and tissue assessment were updated daily in the patient electronic health record. All data were recorded on the same electronic Health record with exception to the questionnaire that was answered online via Survey Monkey Software.
Bias
Bias could be associated to data recording because the study was designed as a retrospective cohort analysis of electronic health record database. In recent studies in NHS hospitals in England [6,21] showed high levels of underreporting for all pressure ulcer categories and provided some recommendations to improve care quality, patient safety and future pressure ulcer monitoring. He found that some data records contained significant missing information that if left unaddressed could reduce the validity of the data. We found also that in several situations is difficult to differentiate between missing data and undesirable values. These analyses of the database help to reduce error and later improve the registration in some fields that we signed as crucial.
Study size
The chosen time interval of 1 year was decided to allow the sample size to be sufficiently large, in order to reduce the sampling error associated with this type of samples.
The results refer to the 604 records of hospitalization that occurred in the ICU unit during the study period (1st June 2012 to 31st May 2013). Four records were excluded because it was not possible to collect any type of data.
Statistical methods and data analysis
Descriptive statistics were calculated for the demographic and clinical variables and sample characterization.
For the quantitative variables, the use of parametric tests was chosen according to the sample size which was higher than 30 [22], it was not necessary to perform tests of normality analysis and assumed was the same distribution normality. For the verification of homogeneity of variances the Levene test was used [22,23]. One-Way ANOVA test, making a multiple comparison of means through the Post Hoc tests of Tukey HSD and Scheffé test, being considered the most robust to deviations from normality and homogeneity of variances [23]. The level of significance was set at 5%. To perform these calculations and processing of data, IBM® software, SPSS® version 20.0 for Windows® was used.
Results
The results section is divided into two parts with respect to the two main goals of the study.
Results from retrospective health records analyses
This study included health electronic records from 600 hospitalised patients (electronic health records). As regards age (Tab. 2), it varies between 18 and 92 years, with a mean of 56.8 ± 15.60 years and a median of 58 years, with a predominance of males (52.7%).
Tab. 2. Distribution according to socio-demographic characteristics (N = 600). 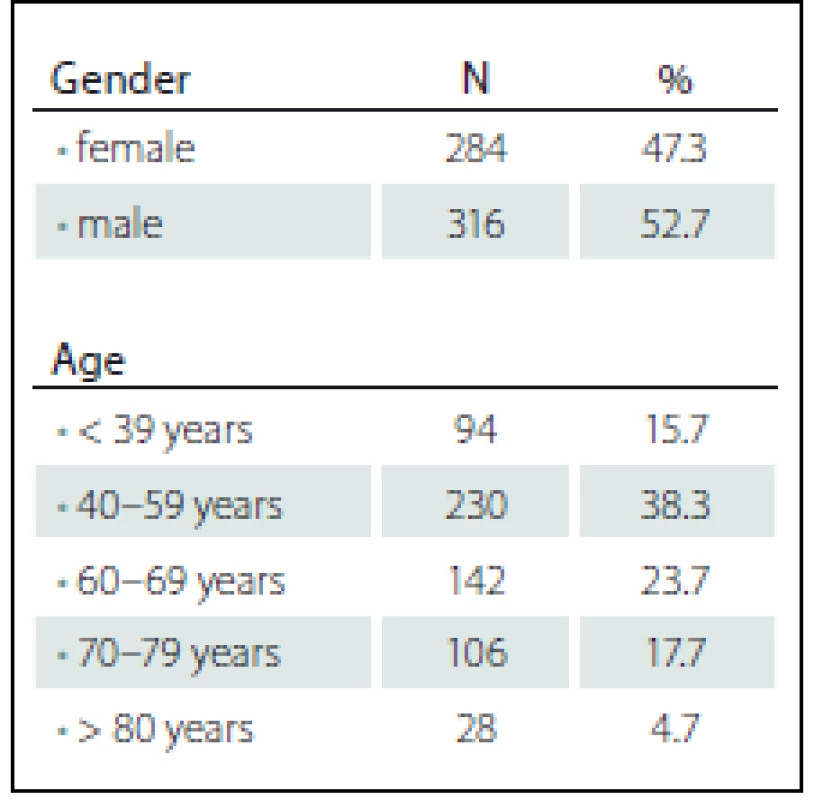
The hospitalization time ranged from 0 days (less than 24 hours) to 50 days, with an average time of 6.5 ± 6.234 days, with a median of 4 days.
The severity of the individuals at entry, evaluated by the APACHE II score, was obtained in 600 of the records, ranging from 1 to 48, with an average value of 20.9 ± 8.7, with a median of 20.
The APACHE II values reported above corresponded to a death probability between 0.032 and 0.96, with a mean of 0.404 ± 0.247 and a median of 0.35. Data that can be verified in Tab. 3.
Tab. 3. Descriptive statistics of hospitalization time and severity of cases admitted considering APACHE II. 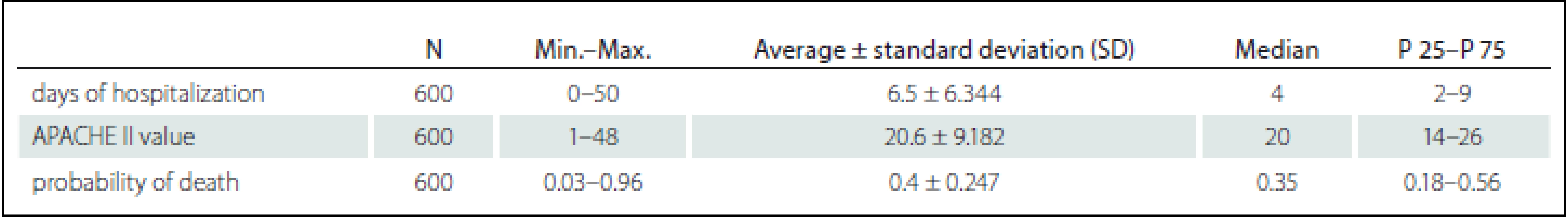
With respect to comorbidities, only 21.3% of the patients had no comorbidities at admission, and in the remaining 78.7% was reported one or more comorbidities.
Thus, hypertension (60.3%) followed by obesity and / or dyslipidaemia (47.5%) are the most frequent. Diabetes and heart disease are present in 20.1% of patients.
Of the admitted cases, there was a mortality rate of 18.5%, corresponding to a total of 111 persons who had died during the retrospective study period.
For the analysis of incidence and prevalence of PUs, the research was carried out in the service data registration program, which included all the nursing diagnoses collected with the focus „Pressure ulcer“, as well as all records created with the attitude „Pressure ulcer“. In this way, all records of PUs created by the nursing team were obtained, since the software allows registration in both formats.
Ulcers present at admission were those identified in the nursing process up to 24 hours after admission to the service. This criterion was chosen taking into account the practice of the service that, when patients are admitted to the immediate postoperative period, due to the frequent hemodynamic and electrical instability verified as well as the discomfort provoked, patients with complete bed rotation are not mobilized for evaluation of the posterior region of the body, this evaluation being done later (especially during hygiene care).
Of the total analysed admission episodes in the study period (N = 600), 98 were identified with at least one PU present during the hospitalization period, corresponding to a prevalence rate of 16.3%. The remaining 502 patients had no PU recording at entry (upon admission) or at any time during hospitalization.
Of the 98 patients who were identified with ulcers, 40.8% presented it upon admission, and 59.2% developed ulceration in the service after 24 hours of admission (N = 58), which resulted in an incidence rate of 11.4%.
Considering the number of ulcers per person, 79.2% had one ulcer (N = 103), 12.3% had two ulcers (N = 16), 4.6% presented three ulcers (N = 6), 3.1% had four ulcers (N = 4), and only 0,8% ulcer (n = 1), which resulted in a total of 130 PUs.
The distribution of these 130 ulcers by category reveals that the most prevalent category was category II (36.1%) followed by category IV (35.4%), then category I (13.1%), and category III (10.8 %). It was also observed that in 4.6% electronic records of PU were no description of the category, because they were on mucosae.
The most common sites of development were found (Tab. 4), and the most prevalent location was the sacral (50.7%), followed by the calcaneus (9.2%), the nose (6.9%), buttock (6.2%), trochanter (4.6%) and back (3.8%). The ulcers presented a very pronounced dispersion and the total locations were grouped according to the anatomical areas where they were, to facilitate the interpretation.
Tab. 4. Distribution of all pressure ulcers identified according to anatomical location (N = 130). 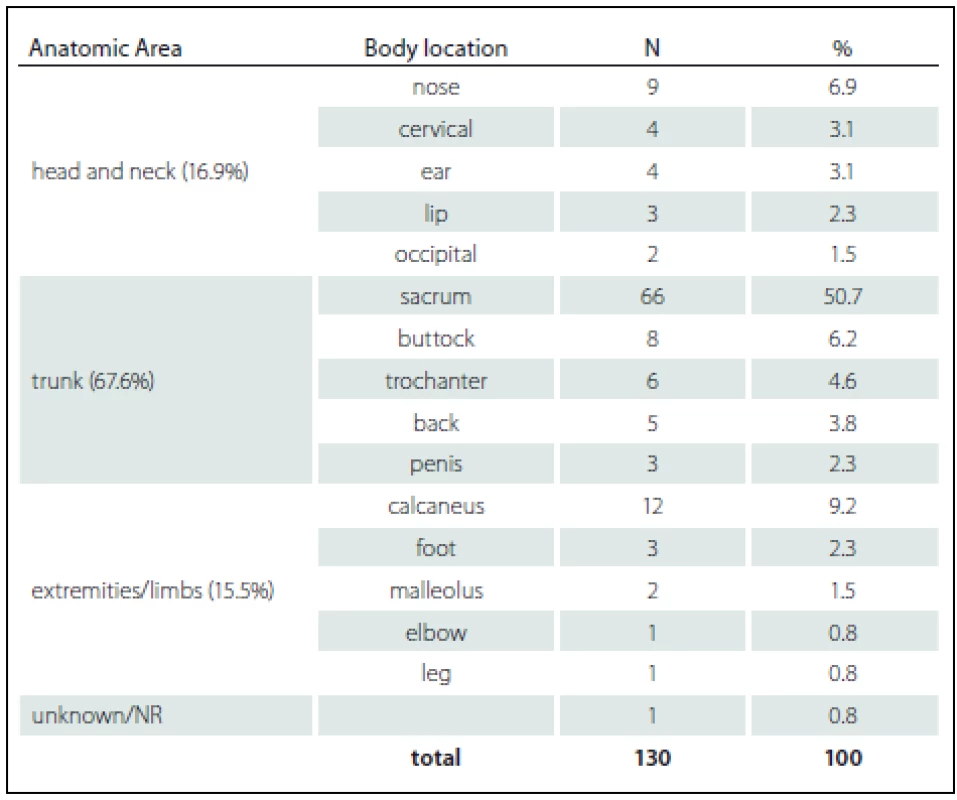
The anatomical location and description of the nursing diagnoses from which the information was obtained revealed that several PUs were associated with medical devices, such as nasogastric tubes, endotracheal tubes, neck collars, ECMO cannulas and external fixators, 29 ulcers with these characteristics were found, corresponding to 22.3% of the total number of PU.
During the time of hospitalisation, 58 patients developed at least one PU again. The mean time for the development of the first PU in the service ranged from 1 to 50 days, with a mean of 7.22 ± 6.935 days, and a median of 5 days.
Considering the analysis of the nursing diagnoses, relative to the incidence (new ulcers acquired in the service) from where the ulcer sites were obtained and considering the anatomical location identified, there were 15 PUs that could be associated with devices (25.8%), in which the ones more expressive were associated with nasogastric tubes, cervical collar, orotracheal tube, and bladder catheter.
Results from questionnaire survey
Regarding the questionnaire performed by the nurses, a response rate of 90% was obtained (N = 27), two did not accept to respond and one of the questionnaires was excluded.
Regarding the time of experience in intensive care, the team is experienced with most of its nurses being in the unit for many years, where it is verified that 55.5% of nurses have worked with critical patients for more than 10 years (Tab. 5).
Tab. 5. Distribution of nurse according professional experience in ICU (N = 27). 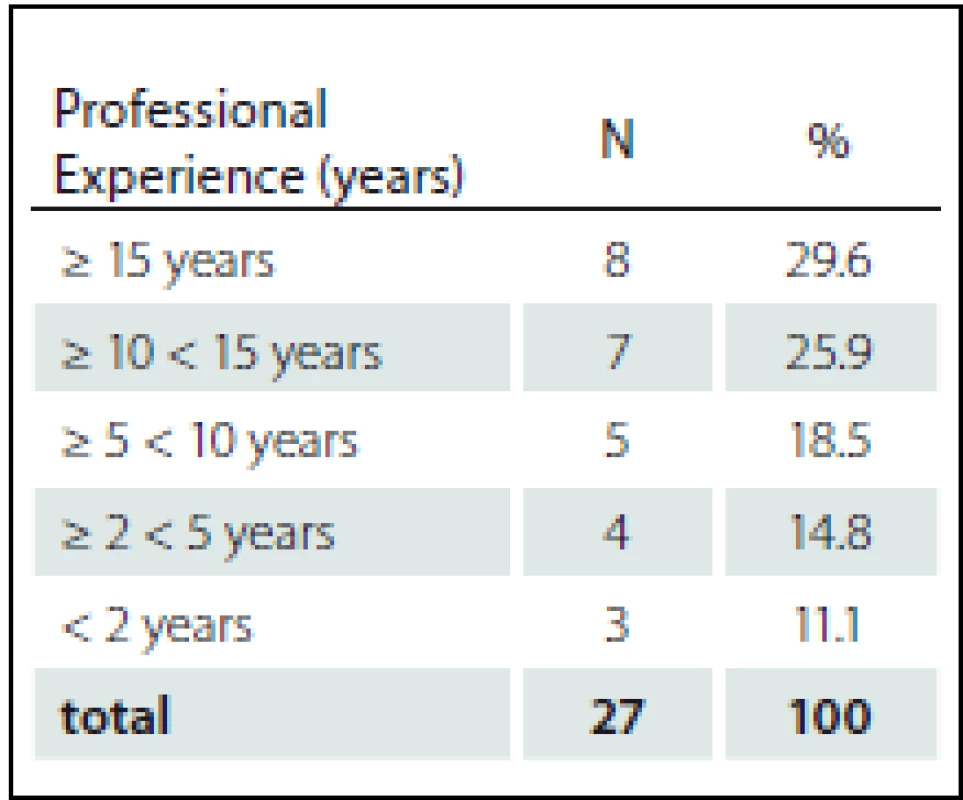
Regarding the difficulties/barriers of the differential diagnosis of PUs by nurses, 77.7% reported difficulty in evaluating PU in patients with peripheral arterial disease; 92.5% referred to the difficulty of evaluating Category I in dark skin; 96.2% reported difficulty in ategory I certainty (bleachable erythema disappears after 1 to 2 hours); 74.07% reported that one of the limitation in the evaluation of PUs is the delay of the first assessment after admission; 81.5% refers to subjectivity in the characterization of UP in the mucosa; 40.7% reported difficulty in the evaluation of PU associated with medical devices; and 51.8% reported difficulty in the differential diagnosis between PU and incontinence associated dermatitis (IAD). The majority of nurses (96.3%) considered it essential to train and upgrade PUs as a way of reducing the subjectivity of PU classification.
Discussion
Considering the cut-off point of 16 points of Braden scale established by Portuguese guidelines, the totality of the study population was identified at “high risk of PU development” at the first PU risk assessment.
Socio-demographic data showed a predominance of male subjects, corresponding to 52.7% of the admissions, similar to other studies. In a multipurpose ICU, this data is in agreement with data found in a surgical intensive care unit, which present a percentage of 56.4% of male inpatients in their study [24]. Similar data was reported in the study of 256 German hospitals, where were mainly male hospitalised (57.1%), were the majority were females in the hospitals [25].
There was a statistically significant relationship (p = 0.000) between the sex of hospitalized patients and the development of PUs, with the male being the most at risk of developing them, a confirmed finding by the study in a ICU in Germany [26] and in contrast to others authors who did not verify this relation [27,28].
As for the severity status of the persons entering the ICU, in this study the value of APACHE II was considered for their analysis, with an average APACHE II value of 20.9. This value is higher than that in other studies, which indicates mean APACHE II values of 17.26 [4], and with APACHE II of 14.6 [29]. This difference translates to a greater severity of the people admitted to the unit of the present study, and effectively, an effective mortality rate was verified superior to the previous work (effective mortality rate of 10%) [4], comparing with the rate of mortality in this study, of 18.5%, corresponding to 111 deaths in the period studied.
Regarding the categorization of the total ulcers identified in the present study, it was verified that the most prevalent category was category II (36,1%) followed by category IV (35.4%), then category I (13.1%), and category III (10.8 %). The higher percentage of these categories may be associated to the time they take to develop, which may mean that the nursing care after its detection is reinforced and effective in its development and subsequent aggravation.
As to the anatomical location of the ulcers identified in this study, it was verified that the most prevalent location was the sacrum, followed by the calcaneus, nose, buttock and trochanter. These data are similar to those reported by Cox [4], with 58% of ulcers in the sacrum, 34% in the buttocks, 5% in calcaneus and 3% in other sites and also by Pokorna et al. [30], who examines incidence of iatrogenic wounds with these locations: 26.0% in buttock, 16.6% sacrum, 5.9% calcaneus, 4.1% abdominal area, 3.6% nasogastric tube, 0.6 urinary catheter and 4.1% other invasive input.
The high number of ulcers identified in the sacrum is highlighted, which may be associated with the higher severity status of the individuals in the present study, justifying a less possibility of bed mobilization due to inherent instability and the need to keep the trunk elevated by invasive ventilation (indicated by the ventilator-associated pneumonia prevention bundle). In a Finnish study, similar data were found, with 45% of ulcers in the sacrum, 22% in the calcaneus and 15.7% in the nose, but the latter associated with non-invasive ventilation masks [31].
High incidences of PUs on the mucosae (lips and penis) made us reflect on the importance of constant evaluation, fixation and change of location of the devices. The high percentage of ulcers associated with medical devices verified in the present study reinforces their association in the incidence and importance of prevention for nursing.
Regarding the Questionnaire to nurses the response rate was of 90% (N = 27), which may insinuate the interest of nurses in this area. Two nurses did not agree to respond and one of the questionnaires was not used as have not been fully filled.
Barriers were identified regarding the time of the first evaluation of the skin, as well as the identification of PU in the mucous membranes or when associated with medical devices. Regarding the old question of the differential diagnosis between PU and IAD, the problem is reported by 51.8% of the sample as observed in other studies [32].
The majority of nurses (96.3%) considered it essential to train and update PUs as a way of reducing the subjectivity of PU classification, as it is also supported by several authors [30,31].
It was identified a great variability of the PU description in the open field destined to the effect, which can lead to the conclusion of subjectivity when classifying and categorizing PU, compatible with other author where it refers the importance of the differential diagnosis of the lesions [30]. One of the more complex cases to characterize about what type of injury to consider were the users who entered the post cardio respiratory arrest unit that came from the pre-hospital external automatic compressor. This fact reinforces the difficulty of differential diagnosis of the lesions, as well as their association with medical devices. The Fig. 1 – 3 presents several lesions caused by external automatic compression.
Fig. 1. Compression zone without loss of skin or tissues. 
Fig. 2. Compression zone with loss of skin or tissues in alive patient. 
Fig. 3. Compression zone with loss of skin and tissues in a death patient. 
As we can verify in the images, not all living or already cadaveric individuals present lesions, it is necessary to identify the time of use of the medical device, association with gender, age, circumstances of device placement and other variables that may influence the development of these lesions. Experience, knowledge of medical devices and training in this area play a key role in the proper recording of observed injuries
Correct gauging of records is essential for the standardization and systematization of data for timely analysis and intervention. The structure of the ulcer register in the software prevents automated screening of ulcer categories and leads to the need for manual analysis and screening of the data to obtain indicators. It is proposed to optimize the computer platform, with the creation in the menu of elaboration of the nursing diagnosis, a space for unambiguous registration (drop-down type) of the category of the ulcer, evolution of the treatment.
Conclusion
The development of PUs is complex and multifactorial and nursing staff needs to manage several (modifiable and non-modifiable) risk factors in order to prevent PU development in inpatient settings.
The person in critical situation has characteristics that make them highly dependent on nursing care, presenting deficits in self-care, namely in maintaining its structural integrity.
The increase in knowledge about the factors that determine its development will allow to allocate the necessary means to reduce the incidence and prevalence of PUs at the hospital level, a factor that is valued as an indicator of quality in health care and to allow a reduction in the person in a critical situation the pernicious effect of its development.
Staff should use all available opportunities (e. g., periodic education, simulation sessions, unit briefings and huddles) to educate about the risks, differential diagnosis and management of medical devices that can cause pressure.
Interdisciplinary team performing the patient assessment should include a review of all devices used with the patient to ensure that the care plan addresses management of medical devices that could cause PUs.
It is considered pertinent to carry out further studies in the field, prospective studies, with evaluation of other variants, namely to evaluate the importance of vasopressors, analgesics, and others in the development of PUs.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 17. 7. 2017
Accepted for print: 26. 7. 2017
Assistant Prof. Paulo Alves, MSc., Ph.D.
Institute of Health Sciences
Catholic University of Portugal
Rua de Diogo Botelho 1 327
4169-005 Porto,
Portugal
e-mail: pjalves@porto.ucp.pt
Zdroje
1. Emily Haesler, ed. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Cambridge Media: Osborne Park, Western Australia 2014.
2. Dealey C, Brindle CT, Black J, et al. Challenges in pressure ulcer prevention. Int Wound J 2015;12 : 309 – 12. doi: 10.1111/ iwj.12107.
3. Coleman S, Nixon J, Keen J, et al. A new pressure ulcer conceptual framework. J Adv Nurs 2014;70(10):2222 – 34. doi: 10.1111/ jan.12405.
4. Cox J. Predictors of pressure ulcers in critical care patients. AM J Crit Care 2011;20(5):364 – 75. doi: 10.4037/ ajcc2011934.
5. Coleman S, Nelson EA, Keen J, et al. Developing a pressure ulcer risk factor minimum data set and risk assessment framework. J Adv Nurs 2014;70(10):2339 – 52. doi: 10.1111/ jan.12444.
6. Coleman S, Smith IL, Nixon J, et al. Pressure ulcer and wounds reporting in NHS hospitals in England part 2: Survey of monitoring systems. J Tissue Viability 2016;25(1):16 – 25. doi: 10.1016/ j.jtv.2015.11.002.
7. Pini L, Alves P. Prevalência, risco e prevenção de úlcerade pressão em unidades de cuidados de longa duração. Tese de Mestrado em Evidência e Decisão em Saúde-Faculdade Medicina da Universidade do Porto 2012;47 – 73.
8. Pokorná A, Benešová K, Jarkovský J, et al. PressureInjuries in Inpatient Care Facilities in the Czech Republic:Analysis of a National Electronic Database. J Wound Ostomy Continence Nurs 2017;44(4):331 – 5. doi: 10.1097/ WON.0000000000000344.
9. Suriadi, Sanada H, Sugama J, et al. Development of a new risk assesment scale for predicting pressure ulcers in an intensive care unit. Nursi Crit Care 2008;13(1):34 – 43. doi: 10.1111/ j.1478-5153.2007.00250.x.
10. Cuddigan J. Critical care. In: Pieper B, ed. National Pressure Ulcer Advisory Panel, editors. Pressure ulcers: prevalence, incidence, and implications for the future. Washington, DC: NPUAP 2012.
11. Dealey C. The care of wounds. A guide for nurses. USA: Wiley-Blackwell 2006 : 127 – 48.
12. Glover D. Let’s own up to the real cost of pressure ulcers. J Wound Care 2003;12(2):43.
13. Flanagan M. Wound Heaing and Skin Integrity: Principles and Practice. Oxford: Jonh Wiley & Sons 2013 : 119 – 33.
14. Briggs SL. How accurate are RGNs in grading pressure ulcers? Br J Nurs 2006;15(22):1230 – 4.
15. Beeckmann D, Schoonhoven L, Fletcher J, et al. EPUAP classification system for pressure ulcers: European reliability study. J Adv Nurs 2007;60(6):682 – 91.
16. Lloyd-Jones M. Is it time to review the way we categorise pressure? Wounds 2011;7(3):92 – 8.
17. Moore Z. Pressure ulcer grading. Nurs Stand 2005; 19(52):56 – 64.
18. Alves P, Mota F, Ramos P, et al. Epidemiologia das úlceras de pressão: Interpretar dados epidemiológicos como indicador de qualidade. Revista Servir 2013;58(1 – 2):10 – 8.
19. Defloor T, Schoonhoven L. Inter-rater reliability of the EPUAP pressure ulcer classification system using photographs. J Clin Nurs 2004;13(8):952 – 9.
20. Black JM, Brindle CT, Honaker JS. Differential diagnosis of suspected deep tissue injury. Int WoundJ 2016;13(4):531 – 9. doi: 10.1111/ iwj.12471.
21. Smith IL, Nixon J, Brown S, et al. Pressure ulcer and wounds reporting in NHS hospitals in England part 1: Audit of monitoring systems. J Tissue Viability 2016;25(1):3 – 15. doi: 10.1016/ j.jtv.2015.11.001.
22. Pestana M, Gageiro J. Análise de Dados para Ciências Sociais: a Complementariedade do SPSS. Lisboa. 6th ed. Lisboa: Edições Sílabo 2014 : 81 – 134.
23. Maroco, J. Análise estatística – Com utilização do SPSS. 3th ed. Lisboa: Edições Sílabo 2003 : 81 – 143.
24. Slowikowski G, Marjorie F. Factors Associated WithPressure in a Surgical Intensive Care Unit. J WoundOstomy Continence Nurs 2010;37(6):619 – 26. doi: 10.1097/ WON.0b013e3181f90a34.
25. Lahmann N, Kottner J, Dassen, T, et al. Higher pressure ulcer risk on intensive care? – Comparison between general wards and intensive care units. J Clin Nurs 2011 : 21(2 – 4):354 – 61,354 – 61. doi: 10.1111/ j.1365-2702.2010.03550.x.
26. Compton F, Hoffmann F, Hortig T, et al. Pressure ulcers pretictors in ICU patients: nursing skin assessments versus objetive parameters. J Wound Care 2010;10 : 417 – 20.
27. Sayar S, Turgut S, Dogan H, et al. Incidence of pressure ulcers in intensive care unit patients at risk according to the Waterlow scale and factors influencing the development of pressure ulcers. J Clin Nurs 2008;18(5):765 – 74.
28. Tschannen D, Bates O, Talsma A, et al. Patient-specific and surgical characteristics in the development of pressure ulcers. Am J Crit Care 2012;21(2):116 – 25. doi: 10.4037/ ajcc2012716.
29. Shahin E, Dassen T, Halfens R. Incidence, prevention ant treatment of pressure ulcers in intensive care patients: a longitudinal study. Int J Nurs Stud 2009;46(4):413 – 21. doi: 10.1016/ j.ijnurstu.2008.02.011.
30. Pokorná A, Saibertová S, Velichová R, et al. Sorrorigenní rány, jejich identifikace a průběh péče. Cesk Slov Neurol N 2016;79/ 112(Suppl 1):S31 – 6. doi: 10.14735/ amcsnn2016S31.
31. Ahtiala M, Soppi E, Wiksten A, et al. Occurrence of pressure ulcers and risk factors in a mixed medical-surgical ICU – a cohort study. JICS 2014;15(4):340 – 3. doi: 10.1177/ 175114371401500415.
32. Beeckmann D. Incontinence-associated dermatitis – current knowledge on etiology, diagnosis, and prevention. Cesk Slov Neurol 2016;79/ 112(Suppl 1):S28 – 30. doi: 10.14735/ amcsnn2016S28.
Štítky
Detská neurológia Neurochirurgia Neurológia
Článok vyšiel v časopiseČeská a slovenská neurologie a neurochirurgie
Najčítanejšie tento týždeň
2017 Číslo Supplementum 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Neuromultivit v terapii neuropatií, neuritid a neuralgií u dospělých pacientů
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
-
Všetky články tohto čísla
- Léčba ran – farmakoekonomická data z pohledu poskytovatele a plátce péče
- Deformace je „zabiják“ buněk – implikace pro ochranu osob s poraněním míchy před vznikem dekubitů
- Vztah mezi rizikovými faktory, hodnocením rizika a patologií vzniku dekubitální léze
- Diferenciální diagnostika dekubitů a dekubity vznikající v souvislosti s přístrojovou technikou
- Možnosti hodnocení psychometrických vlastností škál pro hodnocení rizika vzniku tlakových lézí na vybraných pracovištích v intenzivní péči – pilotní studie
- Využití lalokových plastik v operační léčbě dekubitů
- Výskyt dekubitů u pacientů s lézí míšní na spinální jednotce Kliniky úrazové chirurgie LF MU a FN Brno 2013– 2016
- Kožní léze komplikující Parkinsonovu nemoc
- Validizace ošetřovatelské diagnózy akutní a chronická bolest dle NANDA International u pacientů s ránou
- Dekubity jsou pro mne stále noční můrou
- Editorial
- Datové zdroje pro sledování nehojících se ran v Národním zdravotnickém informačním systému – epidemiologie nehojících se ran v České republice – analýza Národního registru hospitalizovaných v letech 2007– 2015
- Česká a slovenská neurologie a neurochirurgie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Validizace ošetřovatelské diagnózy akutní a chronická bolest dle NANDA International u pacientů s ránou
- Využití lalokových plastik v operační léčbě dekubitů
- Diferenciální diagnostika dekubitů a dekubity vznikající v souvislosti s přístrojovou technikou
- Dekubity jsou pro mne stále noční můrou
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



