-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Conservative management of a ruptured Galassi III middle fossa arachnoid cyst
Konzervativní management prasklé Galassi III arachnoideální cysty střední jámy lební
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors: J. Lodin; A. Hejčl; T. Radovnický; M. Sameš
Authors place of work: Neurosurgical Department, J. E. Purkyne of Masaryk Hospital Krajská Zdravotní a. s., Ústí nad Labem, Czech Republic
Published in the journal: Cesk Slov Neurol N 2019; 82(6): 695-696
Category: Dopis redakci
doi: https://doi.org/10.14735/amcsnn2019695Summary
Background: Arachnoid cysts (ACs) are congenital benign collections of cerebrospinal fluid (CSF) making up to 1% of intracranial lesions and with an estimated at 2,6% in the pediatric population. Conservative and surgical treatment is available for these lesions, yet no specific treatment algorithm is widely accepted. Treatment of choice various based on clinical symptoms, cyst size and location and associated complications such as subdural or intracystic hemorrhage. There is general consensus is that symptomatic ACs are indicated for surgical treatment.
Case Description: The following case report depicts the case of a 15-year-old boy with a large Galassi Type III arachnoid cyst, which was firstly asymptomatic and later presented with transient focal neurological deficits following rupture. A conservative approach was used throughout the case and resulted in spontaneous resolution of the cyst. A short literature review of conservatively treated symptomatic ACs is presented.
Conclusion: This case report demonstrates that a conservative approach of arachnoid cyst treatment may be successful in specific cases of large, symptomatic Galassi III arachnoid cysts, thus avoiding potential surgical risk. Although we believe that a surgical approach is warranted in the majority of cases with symptomatic ACs, a conservative approach should be considered in ACs with mild, transient or vague clinical symptoms and stable diagnostic imaging.
Key words: arachnoid cyst – conservative treatment – hemorrhage – symptomatic
Introduction
Arachnoid cysts (AC) are congenital benign collections of cerebrospinal fluid (CSF) enclosed within arachnoid membranes of the meninges. These entities make up to 1% of intracranial lesions and their prevalence in the pediatric population is estimated at 2,6%, with estimates increasing due to greater availability of MRI and CT scans [1]. The Sylvian fissure is the most frequent location of ACs, making up approximately half of all pediatric ACs [1,2]. The majority of ACs are clinically silent and static in nature, whereas others undergo dynamic changes such as expansion, rupture or spontaneously disappear. A minority of ACs are clinically symptomatic, due to increased intracranial pressure, compression of neighboring structures or changes within the cyst such as intracystic or extracystic hemorrhage. A therapeutic algorithm for symptomatic ruptured arachnoid cysts is not set, however surveys have shown general preference of surgical treatment among surgeons [3]. There is general consensus is that large ACs which are clinically symptomatic should be treated surgically [4,5]. The following case report depicts the case of a 15-year-old boy with a Galassi Type III arachnoid cyst, with two instances of transient focal neurological symptoms following cyst rupture and later spontaneous resolution of the cyst without requiring surgical intervention. Although cases of conservatively managed symptomatic arachnoid cysts are described in literature, usually a conservative approach is not considered, even though it could, in specific circumstances, benefit the patient.
Case report
A male patient was diagnosed with a pigmentous nevus at the age of 3. At 6 years, he underwent a diagnostic algorithm for epidermal nevus syndrome, which included a diagnostic MRI. The MRI scan revealed a large Galassi III arachnoid cyst 8.5 × 3.0 × 9.0 cm in the left frontotemporal region (Fig. 1). It showed slight protrusion of the overlying bone with compression of the underlying brain parenchyma. However, due to the lack of clinical symptoms a conservative approach involving regular follow-ups was decided after discussion with the patient`s parents. One of the routine MRI scans was performed when the patient was 15 and showed subtle signs of intracystic hemorrhage (Fig. 2). However, the patient showed no clinical signs of a neurological deficit, therefore no surgical or pharmaceutical action was taken. One month later, the patient was admitted following a spontaneous episode of transient aphasia, right-sided facial nerve and arm hemiparesis. A CT scan was performed upon admission and showed merely a stable arachnoid cyst with signs of older bleeding (Fig. 3). There was no sign of acute hemorrhage, arachnoid cyst expansion or other intracranial pathology. Even so, the patient was admitted to the pediatric ward for observation. Once admitted, one further identical episode of neurological deficits spontaneously occurred and resolved after approximately 10 minutes. Fundoscopy was performed with normal intracranial pressure and the patient was consequently observed for a total of 5 days. No further episodes of transient neurological deficits occurred, and the patient was released on the fifth day of hospitalization with a planned check-up in the outpatient clinic of the Neurosurgical Department. Sixth months later a follow-up brain MRI was performed and showed almost complete resolution of the entire arachnoid cyst (Fig. 4). A further MRI was performed one year later and showed a stable remnant of the arachnoid cyst. The patient remained symptom free for the entire follow-up period.
Fig. 1. Fig. 1. A Galassi III middle fossa cyst diagnosed at the age of 6.
Obr. 1. Galassi III cysta střední jámy lebni diagnostikována v 6 letech.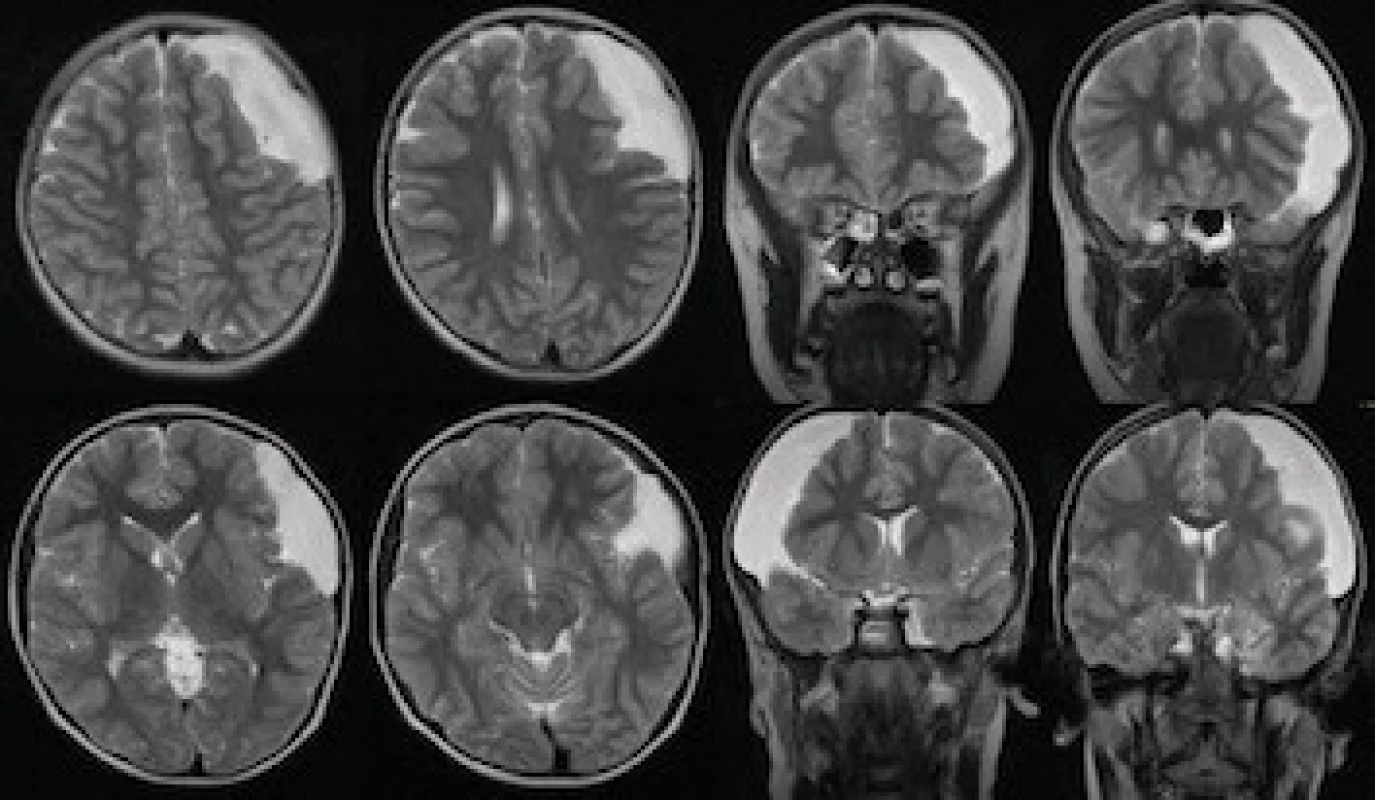
Fig. 2. Signs of older intracystic hemorrhage into the patient`s arachnoid cyst on a routine MRI at age 15.
Obr. 2. Známky staršího krvácení do arachnoideální cysty zobrazeném na rutinní MR v 15 letech.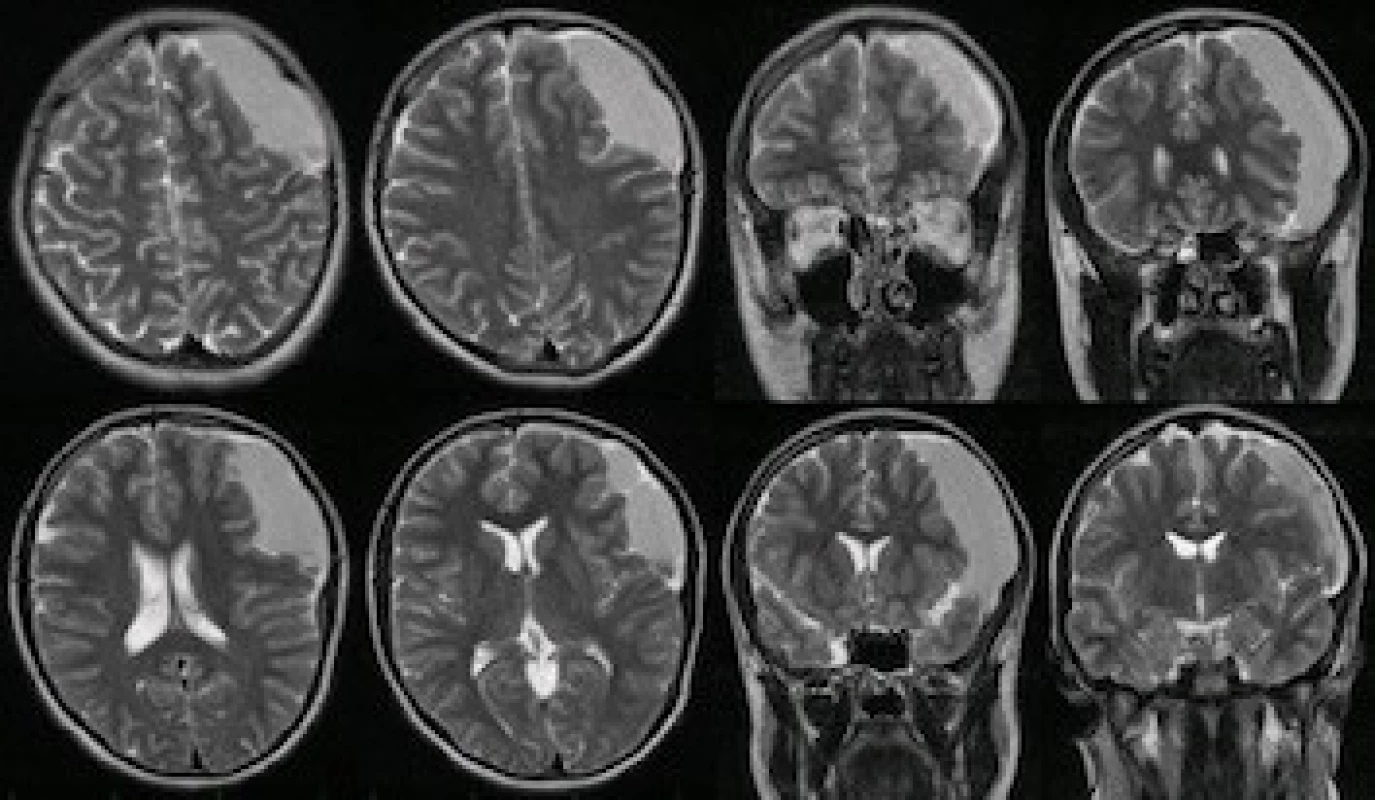
Fig. 3. The patient`s CT scan at admission showing a stable arachnoid cyst.
Obr. 3. Pacientovo vstupní CT mozku zobrazující stabilní arachnoideální cystu.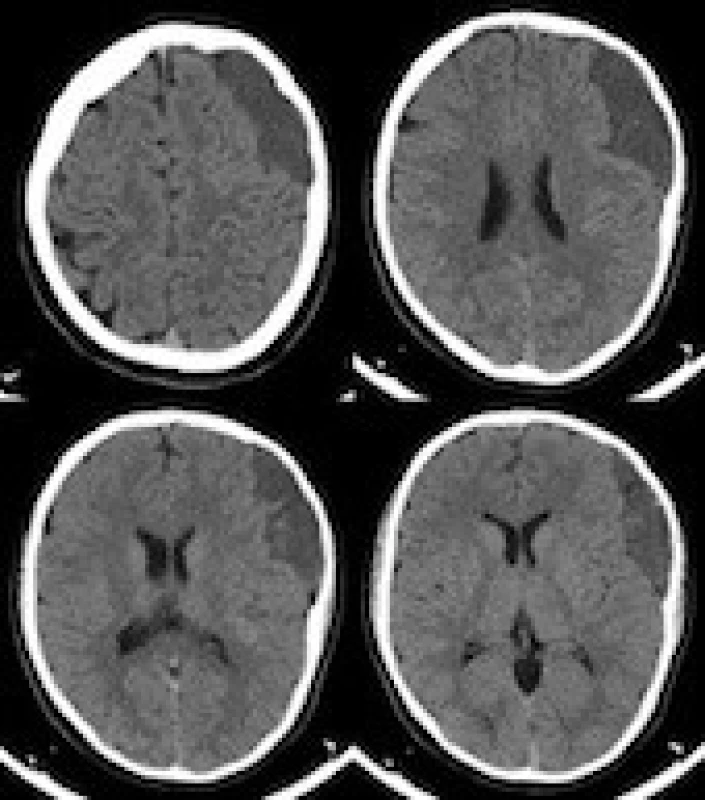
Fig. 4. Near-total resolution of the arachnoid cyst on a 6-month follow-up MRI. Obr. 4. Významná regrese arachnoideální cysty zobrazené na kontrolní MR po 6 měsících. 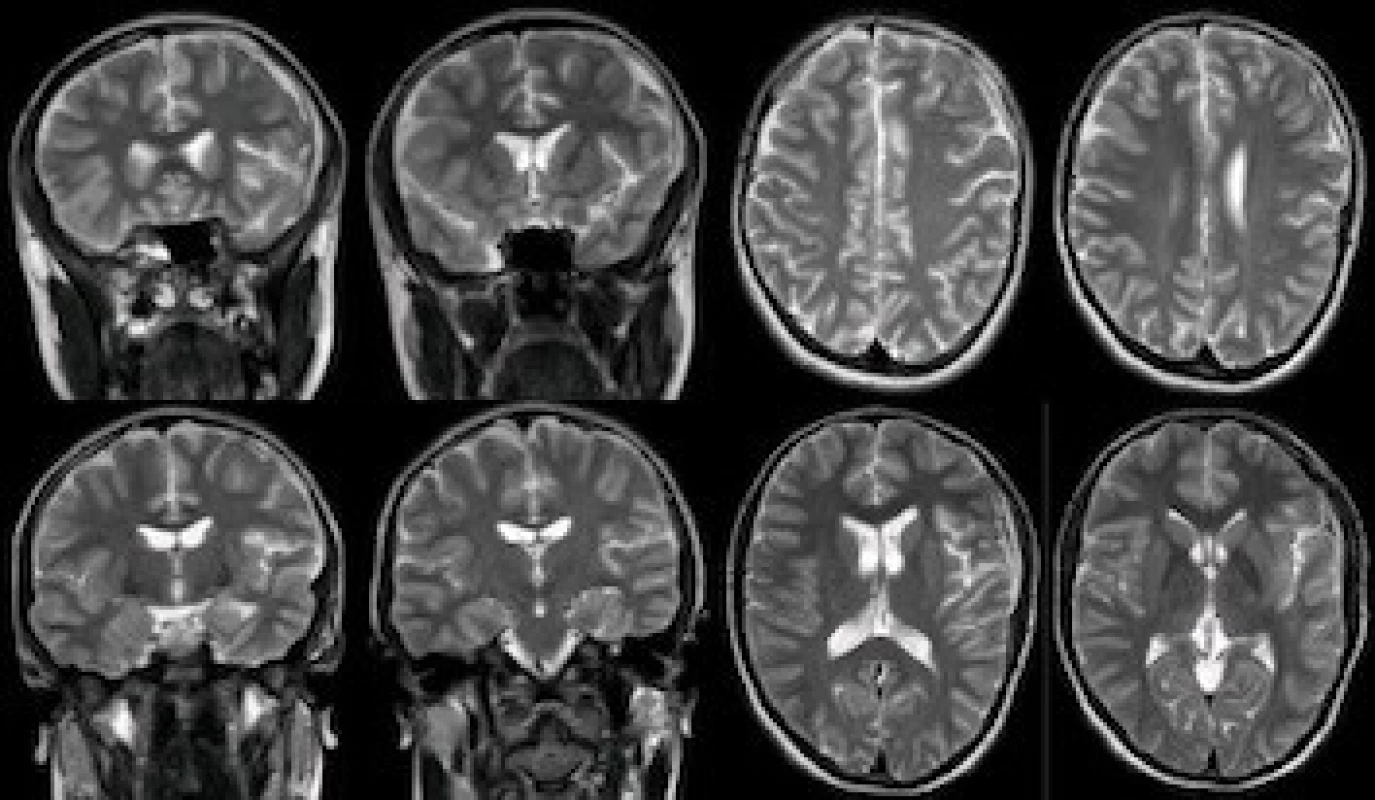
Discussion
Treatment algorithms of ACs in the pediatric population remain a controversial issue, however some universal guidelines have been proposed throughout literature. General management of these lesions can be divided into two categories - cases of asymptomatic ACs which are stable in size and presentation and cases of ACs accompanied by clinical symptoms and/or dynamic changes such as cyst growth, rupture or hemorrhage.
In cases of asymptomatic ACs, there is ongoing debate on the ideal therapeutic approach, with some surgeons preferring a conservative and others a surgical approach. The main argument for a prophylactic surgery is fear of complications such as cyst rupture, which can lead to formation of subdural hematomas or hygromas [3]. A recent article by Cress et al showed that risk factors for cyst rupture or hemorrhage include cyst size above 5 cm and recent head trauma within the previous 30 days, which suggests that for these patients an active approach could be beneficial [6]. On the other hand, it is estimated that 8–27% of ACs are complicated by delayed subdural or intracerebral hematomas following minor head injury, however most of them overlooked and resolve without surgical intervention [7]. Furthermore, hemorrhage can result in spontaneous resolution of ACs, due to the spilling of its contents into subarachnoid or subdural space [8–10]. Consequently, the final decision on whether to treat an asymptomatic AC conservatively or surgically is largely based on surgeon an patient preference. Initially, our case presented as an asymptomatic Galassi III cyst with a diameter over 5 cm, causing slight protrusion of the overlying bone with no history of head trauma. Although we believe some surgeons would choose a surgical course of action based on the cyst size and Galassi III status, we opted for a conservative approach at this stage. The decision was based on the asymptomatic course of the lesion as well as a thorough consult of the patient`s parents, who preferred conservative treatment.
For cases of symptomatic ACs, the general consensus is that surgical treatment is indicated in cases where the clinical symptoms are directly related to the presence of the AC itself [11–13]. Data concerning treatment guidelines of ACs complicated by expansion, rupture or hemorrhage, is mostly limited to case reports [14–16]. Even so, there is a dominating tendency to treat these cases via surgical intervention, as is demonstrated by recent reviews of literature concerning these cases [7,17]. However, it is our opinion that it is necessary to differentiate between mild, transient clinical symptoms and severe permanent neurological deficits with intracranial hypertension, hydrocephalus or seizures. In our case, we opted for a conservative approach for the following reasons. Firstly, when cyst rupture occurred, it was at first asymptomatic and randomly observed on a follow-up MRI, with no signs of intracranial hypertension or focal neurological deficits. Secondly, the patient experienced only transient focal neurological deficits, which spontaneously resolved with no radiological signs of cyst expansion or hematoma formation, when compared to previous imaging. Finally, patient’s parents were thoroughly consulted and were again reluctant to allow their son to undergo surgical intervention. All these factors resulted in a collective decision of our department to manage the situation via a conservative approach, consisting of a five-day observation period and a planned follow-up visit in the outpatient clinic of the Neurosurgical Department. The patient remained symptom-free throughout follow-up and a control MRI showed near-total resolution of the arachnoid cyst, which we consider to be a satisfactory clinical and graphical result.
A literature review of conservatively managed symptomatic ACs yielded 6 cases (Tab. 1). In 3 cases a surgical procedure was planned due to progression of neurological symptoms, however a preoperative diagnostic scan showed either cyst diminishment or resolution and the surgery was canceled [18–20]. In 2 cases the patient or patient guardian was offered surgery but refused the procedure [17,21]. Follow up diagnostic scans showed complete cyst resolution in one case and a stable cyst in the second case. The only case where a surgical course of action was not considered is described by Russo et al [22]. However, in this case, the patient presented with a headache, nausea and nuchal rigidity, which are very vague symptoms attributable to a variety of conditions. The authors even state that they first considered subarachnoid hemorrhage as the cause of patient`s symptoms and when this was ruled out, they opted for a conservative approach. This is in contrast to our case Our case is, to the best of our knowledge, the only published case where a conservative approach was actively used to treat a symptomatic AC presenting with focal neurological deficits directly related to the cyst itself.
Tab. 1. Summary of literature review: symptomatic arachnoid cysts treated conservatively
Author /year
Age/ gender
Cyst location
Clinical symptoms
Surgical treatment offered/planned
Outcome
Complicating factors
Adin et al 2017 [17]
21 years, male
left middle fossa
headache, left hemifacial dysesthesia
offered, but refused
stable cyst
acute subdural hemorrhage adjacent to cyst
Russo et al 2008 [22]
43 years, male
superior cerebellar vermis
headache, nausea, vomiting, nuchal rigidity
no
cyst size reduction
none
Henriques et al 2007 [18]
10 years, male
left middle fossa
headache, vomiting, ocular deviation
planned, however cyst resolved before surgery
cyst resolution
subdural hygroma adjacent to cyst
Pandey et al 2001 [19]
7 months, male
posterior fossa
increasing head diameter, parinaud syndrome
planned, however cyst resolved before surgery
cyst resolution
obstructive hydrocephalus
Rakier et al 1995 [21]
8 years, female
right middle fossa
headache, temporal bone bulging
offered but refused
cyst resolution
none
Takagi et al 1987 [20]
1 year 11 months, male
cerebellopontine angle
left facial palsy, left-sided hearing loss
planned, however cyst resolved before surgery
cyst resolution
cyst expansion with brainstem compression
In all of the conservatively treated cases mentioned above, patients avoided a surgical procedure with acceptable results - resolved diminished or stable ACs. Although the techniques for surgical procedures for these conditions continue to be honed a become less invasive, some surgical risks remain [5,12]. We believe that when deciding on the ideal course of treatment of symptomatic AC cysts it is important to analyze the clinical symptoms in terms of nature, severity and their changes in time. We do not dispute a timely surgical approach in severe cases of permanent or repeated neurological deficits with increased intracranial pressure or hydrocephalus. However, we believe a conservative approach should be considered in cases of mild, transient or vague clinical symptoms with stable diagnostic imaging, as it may yield positive results.
Conclusion
The therapeutic management of ACs remains a controversial topic, with little help in the form of guidelines. The general opinion on management of symptomatic ACs is that a surgical procedure is indicated. Although we believe this is the correct approach in the majority of cases, our case, as well as similar case reports described in literature, demonstrate that a minority of patients presenting with mild, transient or vague clinical symptoms and stable diagnostic imaging, may benefit from a conservative approach. However further studies are required to support this approach further.
The authors declare they have no potential confl icts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Jan Lodin, MD
Department of Neurosurgery J. E. Purkyne University Masaryk Hospital
Rabasova 13
401 11 Ústí nad Labem
Czech Republic
e-mail: jan.lodin@kzcr.eu
Accepted for review: 25. 7. 2019
Accepted for print: 30. 10. 2019
Zdroje
1. Al-Holou WN, Yew AY, Boomsaad ZE et al. Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr 2010; 5(6): 578–585. doi: 10.3171/2010.2.PEDS09464.
2. Adeeb N, Deep A, Griessenauer CJ et al. The intracranial arachnoid mater: a comprehensive review of its history, anatomy, imaging, and pathology. Childs Nerv Syst. 2013; 29(1): 17–33.
3. Tamburrini G, Dal Fabbro M, Di Rocco C. Sylvian fissure arachnoid cysts: a survey on their diagnostic workout and practical management. Childs Nerv Syst 2008; 24(5): 593–604. doi: 10.1007/s00381-008-0585-9.
4. Mustansir F, Bashir S, Darbar A. Management of arachnoid cysts: a comprehensive review. Cureus 2018; 10(4): e2458.
5. Chen Y, Fang HJ, Li ZF et al. Treatment of Middle cranial fossa arachnoid cysts: a systematic review and meta-analysis. World Neurosurg 2016; 92 : 480–490 e2.
6. Cress M, Kestle JR, Holubkov R et al. Risk factors for pediatric arachnoid cyst rupture/hemorrhage: a case-control study. Neurosurgery 2013; 72(5): 716–722. doi: 10.1227/NEU.0b013e318285b3a4.
7. Liu Z, Xu P, Li Q et al. Arachnoid cysts with subdural hematoma or intracystic hemorrhage in children. Pediatr Emerg Care 2014; 30(5): 345–351. doi: 10.1097/PEC.0000000000000128..
8. Beltramello A, Mazza C. Spontaneous disappearance of a large middle fossa arachnoid cyst. Surg Neurol 1985; 24(2): 181–183.
9. Mori T, Fujimoto M, Sakae K et al. Disappearance of arachnoid cysts after head injury. Neurosurgery 1995; 36(5): 938–942.
10. Nadi M, Nikolic A, Sabban D et al. Resolution of middle fossa arachnoid cyst after minor head trauma – stages of resolution on MRI: case report and literature review. Pediatr Neurosurg 2017; 52(5): 346–350. doi: 10.1159/000479325.
11. Erman T, Gocer AI, Tuna M et al. Intracranial arachnoid cysts: clinical features and management of 35 cases and review of the literature. Neurosurgery Quarterly 2004; 14(2): 84–89.
12. Shim KW, Lee YH, Park EK et al. Treatment option for arachnoid cysts. Childs Nerv Syst 2009; 25(11): 1459–1466. doi: 10.1007/s00381-009-0930-7.
13. Kandenwein JA, Richter HP, Borm W. Surgical therapy of symptomatic arachnoid cysts - an outcome analysis. Acta Neurochir (Wien) 2004; 146(12): 1317–1322.
14. Khilji MF, Jeswani NL, Hamid RS et al. Spontaneous arachnoid cyst rupture with subdural hygroma in a child. Case Rep Emerg Med 2016; 2016 : 6964713. doi: 10.1155/2016/6964713.
15. Yuksel MO, Gurbuz MS, Senol M et al. Spontaneous Subdural haematoma developing secondary to arachnoid cyst rupture. J Clin Diagn Res 2016; 10(10): PD05–PD6.
16. Bilginer B, Onal MB, Oguz KK et al. Arachnoid cyst associated with subdural hematoma: report of three cases and review of the literature. Childs Nerv Syst 2009; 25(1): 119–124. doi: 10.1007/s00381-008-0728-z
17. Adin ME, Yildiz MS, Deniz MA et al. Arachnoid cysts with spontaneous intracystic hemorrhage and associated subdural hematoma: report of management and follow-up of 2 cases. Radiol Case Rep 2018; 13(2): 516–521.
18. Henriques JG, Pianetti Filho G, Henriques KS et al. Spontaneous acute subdural hematoma contralateral to an arachnoid cyst. Arq Neuropsiquiatr 2007; 65(4A): 1034–1036.
19. Pandey P, Tripathi M, Chandra PS et al. Spontaneous decompression of a posterior fossa arachnoid cyst: a case report. Pediatr Neurosurg 2001; 35(3): 162–163.
20. Takagi K, Sasaki T, Basugi N. [Spontaneous disappearance of cerebellopontine angle arachnoid cyst: report of a case]. No Shinkei Geka 1987; 15(3): 295–299.
21. Rakier A, Feinsod M. Gradual resolution of an arachnoid cyst after spontaneous rupture into the subdural space. Case report. J Neurosurg 1995; 83(6): 1085–1086.
22. Russo N, Domenicucci M, Beccaglia MR et al. Spontaneous reduction of intracranial arachnoid cysts: a complete review. Br J Neurosurg 2008; 22(5): 626–629.
Štítky
Detská neurológia Neurochirurgia Neurológia
Článek Gunshot injury of the brainČlánek Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke? YESČlánek Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke? NOČlánek Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke?Článek Significant fall risk factors in the personal history of in-patients with neurological diseaseČlánek Recenze knih
Článok vyšiel v časopiseČeská a slovenská neurologie a neurochirurgie
Najčítanejšie tento týždeň
2019 Číslo 6- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Neuromultivit v terapii neuropatií, neuritid a neuralgií u dospělých pacientů
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- CIDP: epidemiológia, klinický obraz a diagnostika v kocke
-
Všetky články tohto čísla
- Gunshot injury of the brain
- Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke? YES
- Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke? NO
- Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke?
- Cervical plexus lesions in clinical practice
- Neurorehabilitation of gait impairment using functional electrical stimulation – current findings from randomized clinical trials
- Difficulty in respecting autonomy in patients with Parkinson’s disease
- Current management of patients with degenerative cervical spine compression
- Intraplaque hemorrhage in symptomatic and asymptomatic progressive internal carotid artery stenosis – a pilot study
- A comparison of perioperative pressure measurements in the aneurysm sac and parent artery in ruptured and unruptured aneurysm
- Significant fall risk factors in the personal history of in-patients with neurological disease
- A systematic review of the clinical efficacy of sacroiliac joint stabilization in the treatment of lower back pain
- Spinal meningiomas – 92 patients operated at our department
- Civilian and military gunshot wounds to the head
- Does choroidal thickness change in Parkinson’s disease?
- Epidural application of steroids Part 1 – Patient profile before application
- Surgical treatment of bilateral drug-resistant Menière’s disease
- Mechanical thrombectomy in the treatment of acute ischemic stroke in childhood
- Conservative management of a ruptured Galassi III middle fossa arachnoid cyst
- Facial nerve reconstruction with great auricular nerve graft following resection of recurrent basal cell carcinoma in parotidomasseteric region
- Doporučení pro mechanickou trombektomii akutního mozkového infarktu – verze 2019
- Analýza dat v neurologii LXXVIII. Směsné míry korelace u vícerozměrných souborů kvantitativních a kvalitativních dat
- Osmdesátiny doc. MU Dr. Jiřího Bauera, CSc.
- Doc. MU Dr. Eugen Eiben, CSc.
- Recenze knih
- Česká a slovenská neurologie a neurochirurgie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Cervical plexus lesions in clinical practice
- Doporučení pro mechanickou trombektomii akutního mozkového infarktu – verze 2019
- Mechanical thrombectomy in the treatment of acute ischemic stroke in childhood
- Gunshot injury of the brain
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



