-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
10-y Risks of Death and Emergency Re-admission in Adolescents Hospitalised with Violent, Drug- or Alcohol-Related, or Self-Inflicted Injury: A Population-Based Cohort Study
In a UK cohort study, Annie Herbert and colleagues compare long-term risks between adolescents hospitalized for adversity - versus accident-related injuries.
Published in the journal: 10-y Risks of Death and Emergency Re-admission in Adolescents Hospitalised with Violent, Drug- or Alcohol-Related, or Self-Inflicted Injury: A Population-Based Cohort Study. PLoS Med 12(12): e32767. doi:10.1371/journal.pmed.1001931
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001931Summary
In a UK cohort study, Annie Herbert and colleagues compare long-term risks between adolescents hospitalized for adversity - versus accident-related injuries.
Introduction
Adolescents (10–19 y olds) are a vulnerable population [1]. Community surveys of adolescents in high-income countries have estimated that up to 50%–60% are exposed to violence, drug/alcohol misuse, or self-harm [2–4]. These adverse experiences are associated with underlying psychosocial difficulties [1] and tend to co-occur [5]. There is evidence that interventions that address psychosocial difficulties have the potential to improve health and social outcomes throughout the rest of the life course [1,6,7].
A presentation to hospital for injury related to violence, drug/alcohol misuse, or self-harm provides an opportunity to assess adolescents’ psychosocial needs or initiate interventions, at a time when these individuals may be willing to consider behaviour change [8–10]. Currently, national guidance in England mandates psychosocial assessment after hospital presentations for self-harm but not after presentations for violent or drug/alcohol-related injury [11]. National guidance for managing patients with violent injury does not exist, and guidelines for managing patients with drug/alcohol-related injury focus on adult patients with drug/alcohol dependence [12,13]. If adolescents presenting with these injuries are at increased risks of future harm, then psychosocial management might be appropriate.
We have previously reported the prevalence of emergency admissions for violent, drug/alcohol-related, and self-inflicted injury for adolescents in England. Approximately 4% of girls and boys have such an admission at least once between the ages of 10 and 19 y old, accounting for one-third of adolescents admitted with any injury (the majority of the remaining two-thirds are related to accidents) [5]. In England, it is estimated that among adolescents who present to hospital with self-inflicted injury, 27.3% re-present with another self-inflicted injury in the next 1–7 y [14], and at least 9.9/1,000 die in the next 1–10 y. In a recent US study of young people presenting with violent and/or drug/alcohol-related injury, 22.4%–36.7% of those surveyed within the 2 y after discharge had re-presented with a violent injury [15]. We found no published studies reporting risks of death or re-admission through any cause following all three types of adversity-related injury (violent, drug/alcohol-related, or self-inflicted injury).
We used national hospitalisation data for England to determine the cumulative risks of death and emergency re-admission in adolescents over the 10 y after discharge following an admission for violent, drug/alcohol-related, or self-inflicted injury. We determined whether risks after adversity-related injury were increased compared with after accident-related injury (our hypothesis was that they would be). We also examined whether risks of death or emergency re-admission differed by sex and age or were associated with underlying chronic conditions, ethnicity, or deprivation.
Methods
Study Design and Setting
We used anonymised Hospital Episode Statistics (HES) data comprising all hospital admissions to the National Health Service (NHS) in England from 1 April 1997 to 31 March 2012 [16]. We compared outcomes for adolescents admitted to the emergency department for an adversity-related injury with those admitted with an accident-related injury. HES data captured the vast majority of our population of interest, i.e., patients admitted to hospital for injury in England [17]. Therefore, we did not carry out a sample size calculation.
We identified adolescents (aged 10–19 y inclusive) who had one or more emergency (acute, unplanned) admissions for injury. We considered any multiple admissions within 1 d of each other, or relating to a hospital transfer, to be the same admission. We defined “emergency” admissions by the HES “method of admission” variable [18], and “injury” by the use of any “S” or “T” International Classification of Diseases–10th Revision (ICD-10) diagnosis code in the admission record [19]. Most adolescents (89%) had only one emergency admission for injury at age 10–19 y and between 1 April 1997 and 31 March 2012, which was defined as the index admission. For adolescents who had two or more emergency admissions for injury, we randomly selected one as the index admission. We chose to select an index admission randomly rather than using the first admission as this would better represent presentations seen in practice. Adolescents who died at the index admission, had an invalid discharge date, or were not discharged by 31 March 2012 were excluded from analyses.
We received a standard, de-identified data extract from the Health and Social Care Information Centre (HSCIC), which does not require research ethics approval or patient consent [20]. The original study design and analysis plan (at the outset of the study) and deviations from this plan are summarised in S1 Table.
Exposure and Outcome
We used ICD-10 codes recorded in the index admission record to define two cohorts of adolescents who were alive at discharge (Fig 1). We defined one cohort of adolescents whose index admission was for “adversity-related injury”, i.e., codes indicating any injury coupled with violence, intentional self-harm, or drug/alcohol misuse We defined drug/alcohol “misuse” as any codes indicating drug or alcohol use, since emergency admission for injury combined with drug or alcohol use indicates clinically important evidence of harm. The comparison cohort comprised adolescents whose index admission record had no codes indicating adversity-related injury but codes indicating “accident-related injury”. Codes used to define adversity and accidents are described elsewhere [5] and have been validated using hospital clinician records [21]. An admission may be categorised as being for more than one type of adversity-related injury because up to 20 ICD-10 codes can be recorded per admission. Adolescents who had an emergency admission for injury with no codes for adversity or accident were excluded from the analyses. The majority of those excluded had complex conditions or complications of surgery [5].
Fig. 1. Formation of adversity-related injury and accident-related injury cohorts among 10–19 y olds. 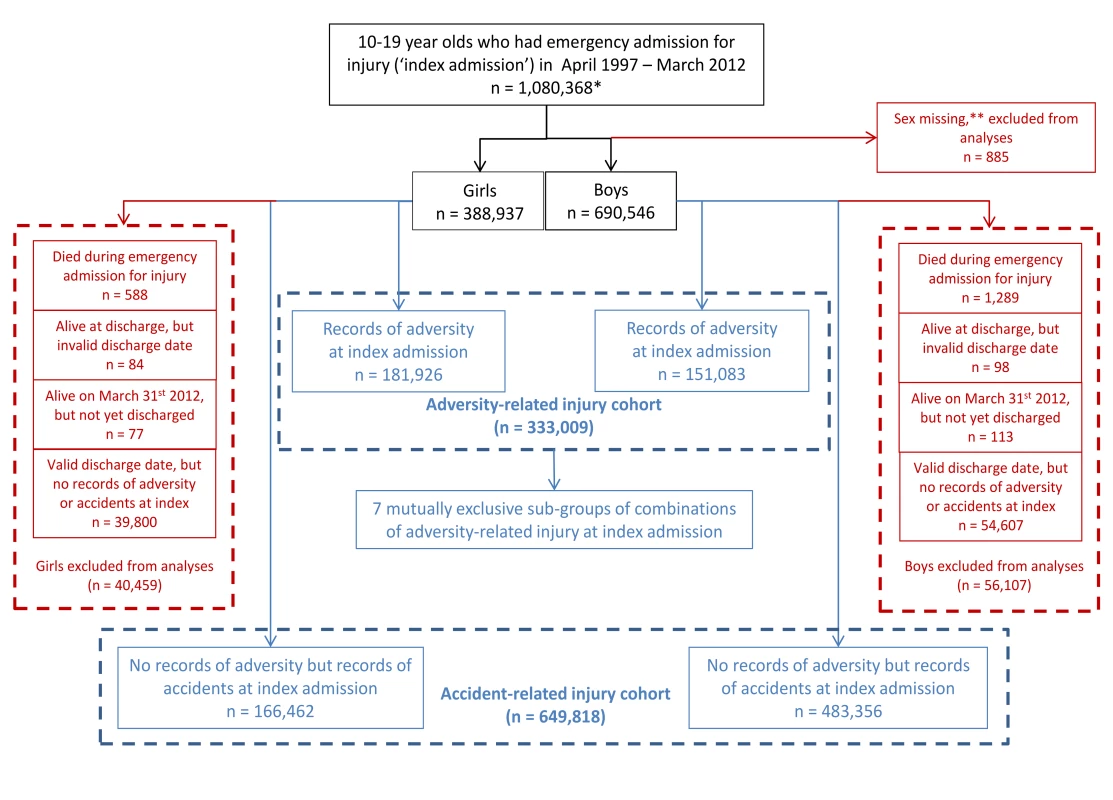
*49,784 girls and 80,205 boys had more than one emergency admission for injury between 10 and 19 y. For each of these adolescents, one emergency admission for injury was randomly selected as the index emergency admission for injury. **Not possible to impute any missing values at 0–30 y old. The outcomes were death and emergency re-admission at least 1 d after discharge from the index admission and up to 10 y later. Death was captured by linking hospital admissions to UK death registration data from the Office for National Statistics [22]. Re-admissions were captured by linking records for the same person using a HES pseudo-identifier, which was specific to our data extract. These identifiers are generated by the HSCIC using a deterministic algorithm to link all episodes of care within the English NHS using sex, date of birth, NHS number, and postcode [23]. Linkages are carried out by the HSCIC before sending out standardised data extracts.
Confounders and Risk Factors
We included age, chronic condition status, deprivation (socioeconomic status), and ethnicity, as recorded at the index admission, as possible confounding variables, or independent risk factors, for death and re-admission, based on previous studies that have shown associations between these factors and harm in adolescents [5,24]. Other factors, such as family and neighbourhood factors, are associated with risks of future harm [25]. We did not include these confounding factors in our analyses as they are unlikely to be used by clinicians or service providers to identify groups at high risk of subsequent harm who might benefit from interventions.
We grouped adolescents into three age groups (10–14, 15–17, 18–19 y) to reflect stages of development [5]. We defined a chronic condition as any record of a chronic physical or mental condition at the index or any preceding admission based on a previously validated cluster of ICD-10 codes (excluding codes for adversity) [5]. This cluster defines a chronic condition as one requiring at least 1 y of medical treatment or follow-up [26]. We grouped the 16 ethnicity categories provided in HES into five categories (white, black, Asian, mixed, other) [27], such that groups would be large enough to stratify analyses by age and sex. Deprivation was grouped according to quintiles of Index of Multiple Deprivation (IMD) score based on residential postcode (with the least deprived areas having a score lower than the first quintile and the most deprived areas having a score higher than the fourth quintile) [18,28]. We grouped deprivation by quintile because previous research has shown differences between quintiles in the incidence of admission for violent injury [29].
We addressed data quality by replacing missing or inconsistent variables with the corresponding modal value for all admission records on the same individual. We replaced 0.8% of records with modal values for sex, 30.2% for ethnicity, and 1.8% for deprivation value. We analysed any residual missing variables for sex, ethnicity, or deprivation as “missing”. No data were missing for age or chronic condition status.
Analyses
All analyses were carried out separately for girls and boys, given well-established differences in the frequency of adversity-related injury between the sexes [5]. We used time-to-event analysis methods (Kaplan–Meier estimates and Cox regression) to account for variation in the length of follow-up.
To determine the absolute risks of death and emergency re-admission in each cohort, we calculated Kaplan–Meier cumulative probabilities and 95% confidence intervals (CIs) for each age group from 1 d to 10 y after discharge from the index admission. We also calculated 1-, 5-, and 10-y risks of death and re-admission following any violent, any drug/alcohol-related, and any self-inflicted injury. To allow comparison of the risks of death in the adversity-related and accident-related injury cohorts with those in the general population, we derived general population estimates of risks of death in 10–19 y olds in 1997–1999 for the next 1–10 y in 1-y increments using aggregate statistics published by the Office for National Statistics (see S2 Table for details on how these numbers were derived) [30]. A comparison of risks of re-admission in our cohorts with risks for adolescents in the general population was not possible as only 12% of the general population of adolescents had an emergency admission for injury at all [5].
We tested for differences in risks of death and emergency re-admission over time between the two cohorts using Cox regression, and present hazard ratios (HRs) with 95% CIs. Models were adjusted for confounders in stages. We first estimated crude HRs between the two cohorts, and then estimated HRs adjusting for age; age and chronic condition status; and age, chronic condition status, ethnicity, and deprivation. Estimated HRs were attenuated after adjusting for age, (e.g., by 15.5% for death in girls). However, further adjustments for chronic condition status, ethnicity, and deprivation did not substantially alter age-adjusted HRs. We therefore present the main comparison of the two cohorts adjusted by age only. However, because chronic condition status and deprivation were independently associated with death and re-admission, we report the absolute 10-y risks of these outcomes after adversity-related and accident-related injury in Table A6 in S1 Text.
As different types of adversity-related injury tend to co-occur [5], we estimated age-adjusted HRs of death and emergency re-admission for seven mutually exclusive combinations of violent, drug/alcohol-related, and self-inflicted injury (all versus accident-related injury). To determine whether there were additional risks of multiple emergency re-admissions for adolescents with adversity-related injury, we also estimated age-adjusted HRs of a second, third, fourth, and fifth emergency re-admission (less than 5% of adolescents had more than five re-admissions).
We tested the goodness of fit of the Cox regression models by plotting the Nelson–Aalen estimate of the cumulative hazard function against Cox–Snell residuals [31]. Analyses were conducted in Stata/SE 12 (StataCorp).
Results
Study Population
Of the 1,080,368 adolescents who had an emergency admission for injury, nearly one-third (n = 333,009) formed the adversity-related injury cohort, and 60% (n = 649,818) formed the accident-related injury cohort (Fig 1). The remaining 9% were excluded (0.2% who died at the index admission, 0.04% who either had an invalid discharge date or were not discharged by 31 March 2012, and 8.7% who were admitted with other causes of injury).
There were similar numbers of girls and boys in the adversity-related injury cohort, but boys outnumbered girls by 2 : 1 in the accident-related injury cohort (girls: 166,462, boys: 483,356). Compared with the accident-related injury cohort, adolescents in the adversity-related injury cohort were on average older at their index admission, more likely to have a chronic condition, and more likely to be from the most deprived areas according to IMD score (Table 1). The most common chronic conditions were chronic respiratory disorders (e.g., asthma), affecting 39.8% to 55.4% of the girls and boys with either adversity - or accident-related injury who also had a chronic condition (Table A1 in S1 Text). Mental health or behavioural disorders (that were not already in the definition for “adversity”) affected 33.0% to 33.5% of the girls and boys with an adversity-related injury and a chronic condition, but only 9.0% to 12.3% of the girls and boys with an accident-related injury and a chronic condition.
Tab. 1. Characteristics at discharge from index emergency admission for injury. 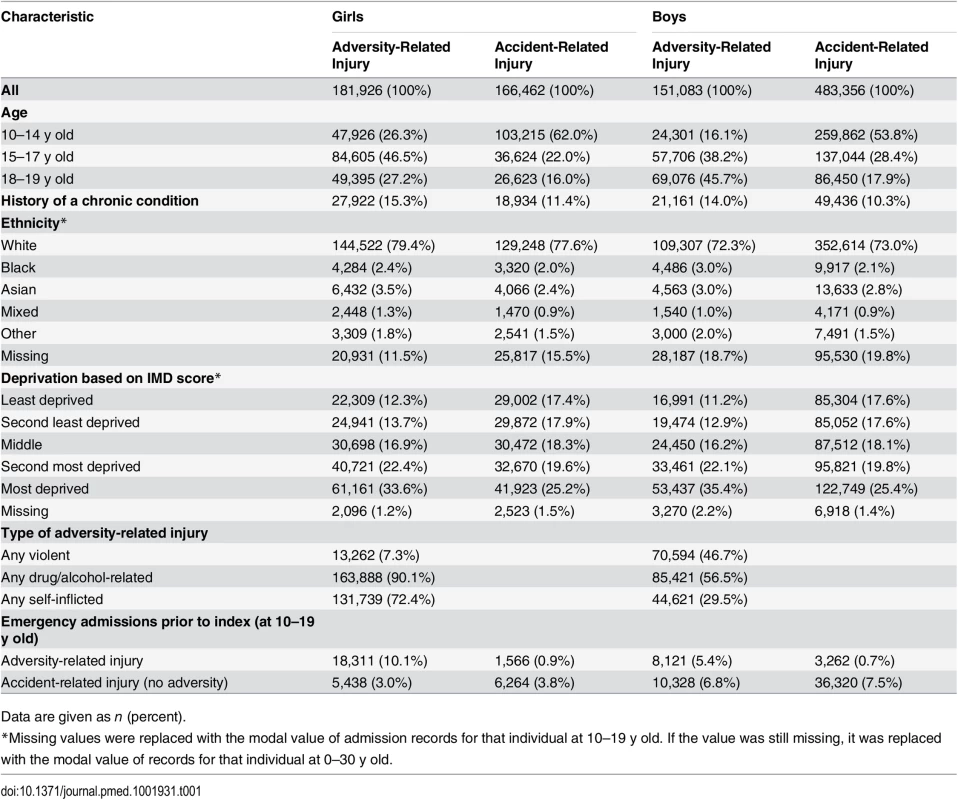
Data are given as n (percent). In the adversity-related injury cohort, girls were admitted predominantly for drug/alcohol-related (90.1%) or self-inflicted (72.4%) injury, while boys were most often admitted for violent (46.7%) or drug/alcohol-related (56.5%) injury. The distribution of ethnicity did not differ substantially between the two cohorts. The median follow-up time from the index admission ranged from 6.8 to 7.7 y in both cohorts (Table A2 in S1 Text).
Risk of Death
There were 4,782 deaths within 10 y of discharge (2,415 after adversity-related injury; 2,367 after accident-related injury) (Table A2 in S1 Text). There were twice as many deaths during the 10 y after discharge as during hospitalisation for the index admission: 71.8% of all deaths between the index admission date and 10 y later occurred after discharge from the index admission. The average time to death post-discharge in the two cohorts ranged from 3.1 y for boys admitted with accident-related injury to 4.1 y for girls admitted with accident-related injury.
At 10 y, the cumulative risk of death after hospital discharge in the adversity-related injury cohort was 7.3/1,000 for girls (equivalent to one in 137; 95% CI, one in 147 to one in 128) and 15.6/1,000 for boys (one in 64; 95% CI, one in 68 to one in 61), compared with 3.7/1,000 girls (one in 270; 95% CI, one in 294 to one in 244) and 6.0/1,000 boys (one in 167; 95% CI, one in 175 to one in 159) in the accident-related injury cohort (Table A3 in S1 Text). Risks of death after discharge were higher following adversity-related injury than accident-related injury at all time points (Figs 2 and 3), and risks after either adversity-related or accident-related injury were higher than in the general population (Fig 4). Among girls and boys, the age group with the highest risk of death was 18–19 y olds (Figs 2 and 3). For girls in this age group, one in 90 died by 10 y after discharge from an admission for an adversity-related injury compared with one in 175 after an accident-related injury (Table A3 in S1 Text). The corresponding figures for boys in this age group were one in 52 and one in 115.
Fig. 2. Cumulative risk of death in girls, by age group. 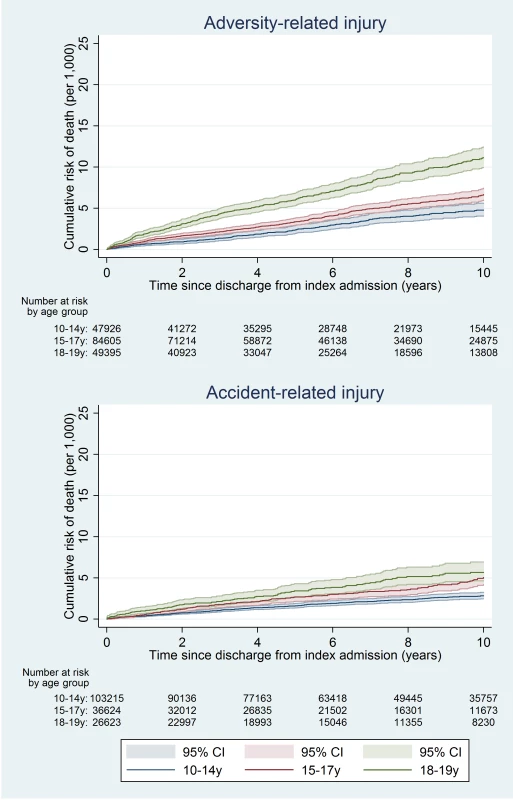
Fig. 3. Cumulative risk of death in boys, by age group. 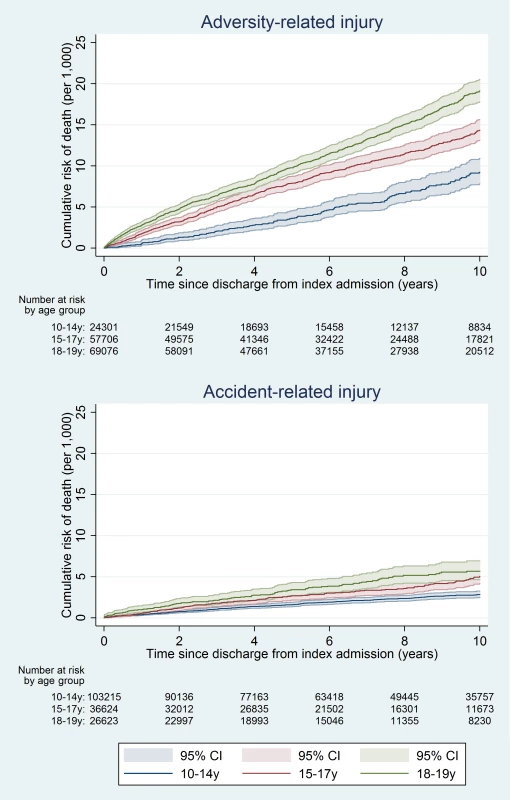
Fig. 4. Estimated cumulative risk of death for girls and boys in the general population, by age group. 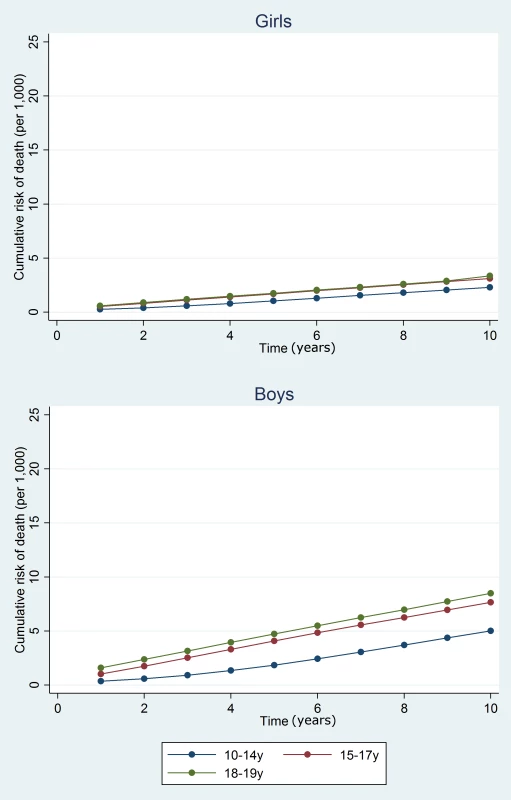
On average over the 10 y after discharge, risks of death in the adversity-related injury cohort compared with the accident-related injury cohort were 61% (95% CI 43%–82%) higher in girls and 113% (95% CI 98%–129%) higher in boys, after adjusting for age (95% CIs greater than unity; Table 2). Risks of death were increased in girls and boys after all combinations of violent, drug/alcohol-related, and self-inflicted injury, compared with accident-related injury (age-adjusted HRs 1.09 to 5.35; Figs 5 and S1). These risks were highest after combinations of adversity-related injury that included drug/alcohol-related injury (age-adjusted HRs: 1.61 to 5.35), though not statistically significantly for girls admitted for all three types of adversity-related injury (age-adjusted HR 2.43, 95% CI 0.91–6.51). Results of models adjusted for clinically relevant variables selected a priori are presented in Table A4 in S1 Text.
Fig. 5. 10-y risk of death by type of injury. 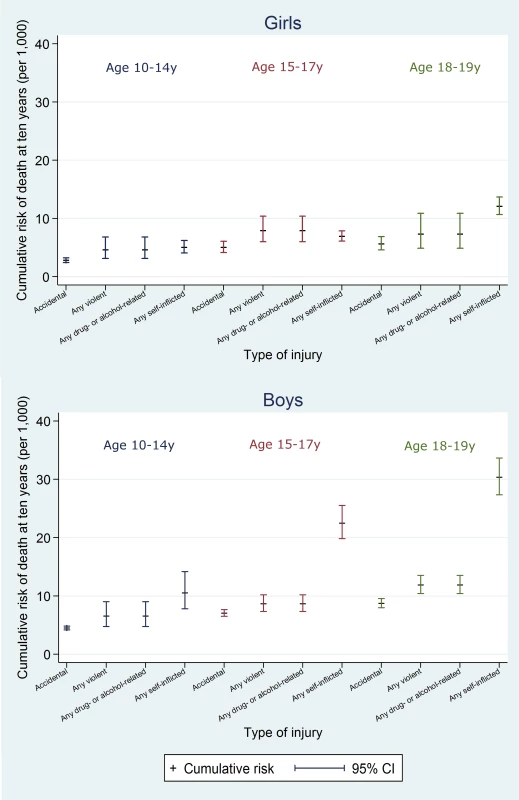
Tab. 2. Relative risks of death and emergency re-admission within 10 y of index admission. 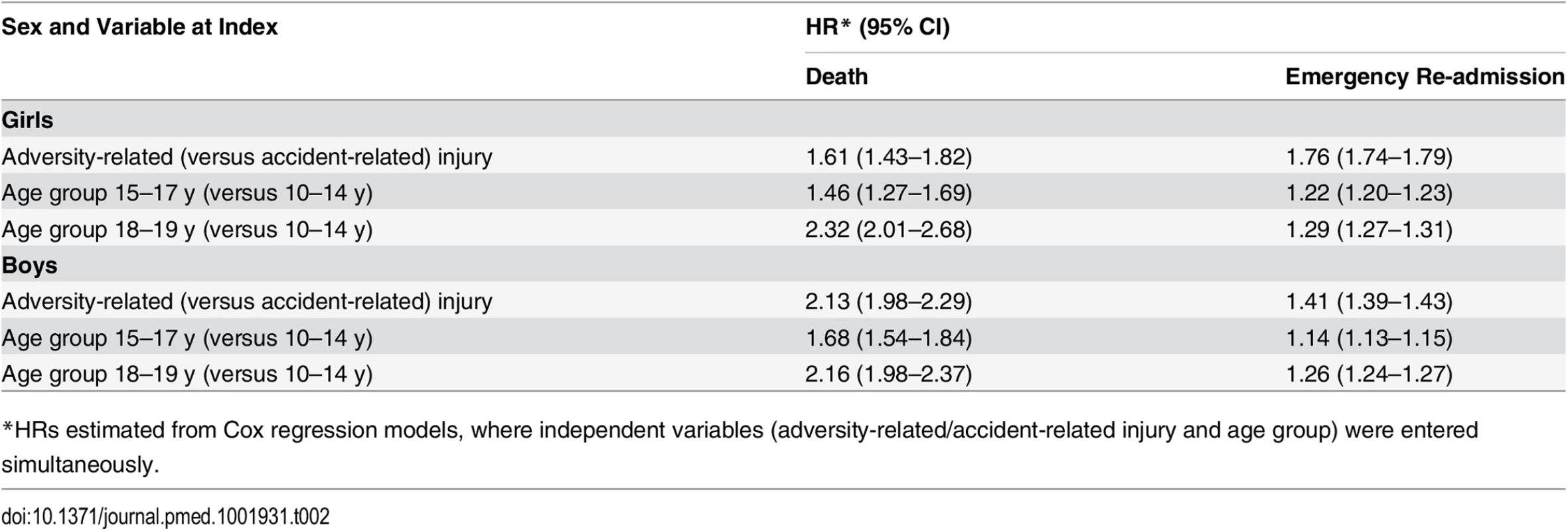
*HRs estimated from Cox regression models, where independent variables (adversity-related/accident-related injury and age group) were entered simultaneously. Risk of Emergency Re-admission
There were 621,050 emergency re-admissions in both cohorts in total (Table A2 in S1 Text). On average, adolescent girls and boys in the adversity-related injury cohort had their first emergency re-admission 586 and 750 d, respectively, after discharge from the index admission, 6 and 12 mo sooner than for the accident-related injury cohort.
The 10-y risk of emergency re-admission was 54.2% for girls (95% CI 53.9%–54.5%) and 40.5% for boys (95% CI 40.2%–40.9%) (Table A5 in S1 Text). The cumulative risk of emergency re-admission was higher in the adversity-related injury cohort than in the accident-related injury cohort at all time points for all age–sex groups (Figs 6 and 7). In contrast to the patterns observed for cumulative risk of death, girls had a higher risk of emergency re-admission than boys for all age groups in both cohorts at all time points. The 10-y risks of emergency re-admission were higher after all types of adversity-related injury than risks in the accident-related injury cohort, for both sexes; in boys, risks were highest after self-inflicted injury (Fig 8).
Fig. 6. Cumulative risk of emergency re-admission in girls, by age group. 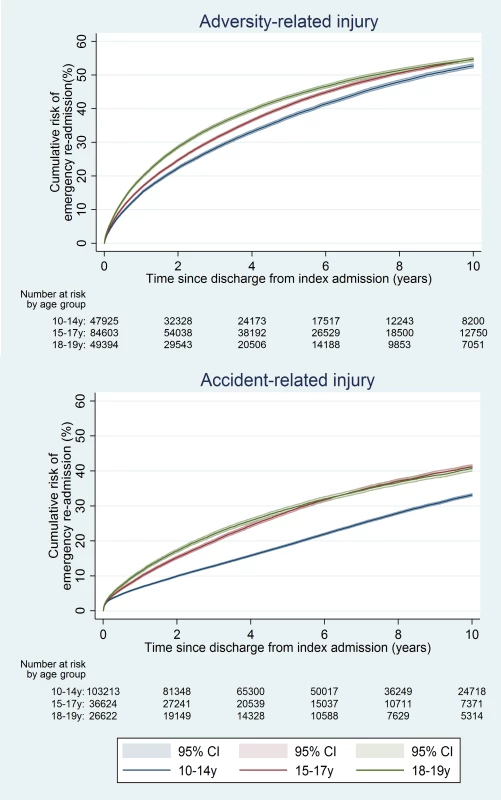
Fig. 7. Cumulative risk of emergency re-admission in boys, by age group. 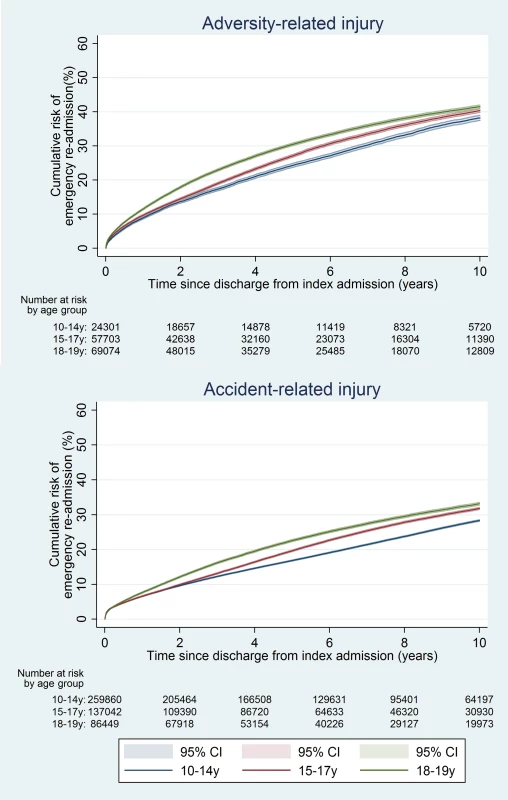
Fig. 8. 10-y risk of emergency re-admission by type of injury. 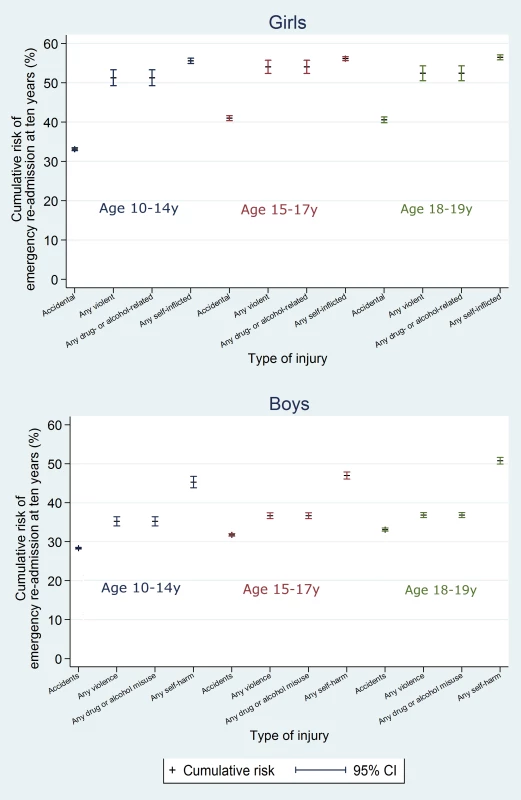
By 10 y after discharge, the risk of emergency re-admission was 76% higher for girls and 41% higher for boys in the adversity-related injury cohort than for those in the accident-related injury cohort (95% CIs for age-adjusted HRs greater than unity; Table 2). Risks of emergency re-admission were highest after an injury that included self-inflicted injury in both girls and boys (age-adjusted HRs 1.29 to 3.10; S1 Fig). Results of models adjusted for clinically relevant variables selected a priori are presented in Table A4 in S1 Text.
Risk of Multiple Emergency Re-admissions
Compared with the accident-related injury cohort, adolescents in the adversity-related injury cohort were more likely to have multiple emergency re-admissions after discharge (girls: 23.2% versus 11.64%, boys: 13.4% versus 7·0%; Table A2 in S1 Text) and were more likely to have a higher number of re-admissions (Table A6 in S1 Text). This was the case for all combinations of adversity-related injury, after adjustment for age, in both girls and boys.
Independent Risk Factors
Relative risks of death and emergency re-admission for adversity-related injury (versus accident-related injury, estimated from Cox regression models), adjusted for age, chronic condition status, ethnicity, and deprivation are presented in Table A4 in S1 Text. In both the adversity-related and accident-related injury cohorts, presence of a chronic condition increased the risks of death and emergency admission by 2 - to 5-fold in girls and boys, and girls and boys living in the most deprived areas based on IMD score had the highest risks of death and emergency re-admissions. This association persisted across all deprivation levels for deaths in boys and for emergency admissions in girls and boys (Table A7 in S1 Text).
We found no association between ethnicity and long-term risks of death or emergency re-admission after adjusting for deprivation and underlying chronic condition (Table A4 in S1 Text). Missing information on ethnicity or deprivation was associated with reduced risks of death and emergency re-admissions in girls and boys, possibly because of a failure to link recurrent admissions for individuals with incomplete data.
Discussion
We report cumulative risks of death and emergency re-admission in adolescents in the 10 y after discharge from an admission for adversity-related injury versus accident-related injury. We found increased long-term risks of death and re-admission among adolescents discharged after hospitalisation for violent, drug/alcohol-related, or self-inflicted injury, compared with those discharged after accident-related injury. Risks of harm after both adversity-related and accident-related injury were higher than for adolescents in the general population. In the 10 y after discharge following an adversity-related injury, one in 137 girls and one in 64 boys died across all adolescent age groups. These risks for 18–19 y olds were one in 52 and one in 90. However, risks of death and re-admission were highest after any drug/alcohol-related injury or self-inflicted injury for both sexes. Having a chronic condition (typically respiratory or mental health/behavioural disorders for adolescents in this study) and living in the most deprived areas (based on residential postcode) increased the risks of death and re-admission.
Strengths and Limitations
One strength of our study is the use of administrative data to study the entire population of adolescents hospitalised with injury within the English publicly provided NHS. Second, linkage of all hospital admissions and death records made it possible to study outcomes 10 y after discharge from the index admission. Third, this is the first study to our knowledge that has quantified risks of harm in adolescents after all three of violent, drug/alcohol-related, and self-inflicted injury within the same cohort. Long-term follow-up has previously been reported only after self-inflicted injury [14].
One limitation of our study is potential misclassification of violent, drug/alcohol-related, or self-inflicted injury as accident-related injury [32,33], which would likely lead to underestimation of the increased risk associated with adversity-related injury. For example, a study in one US hospital site showed that for up to 25% of cases of violent injury in children where violence was recorded in the medical notes, violence was not coded in the electronic discharge records [34]. Misclassification as accident-related injury may be more likely in boys, for whom behaviours such as violence or misuse of alcohol may be normalised and less likely to be noted in hospital records than for girls [35].
Another limitation is that linkage error may lead to a failure to capture death or re-admission and is more common in certain ethnic minorities. For example, in a study where the HES linkage algorithm was applied in another routine paediatric dataset, children and adolescents with black or “other” (i.e., not white, black, Asian, or mixed) ethnicity were approximately 2.4 to 4.1 times more likely to have a false or missed match than their white counterparts [36]. Failure to link events would favour underestimation of the risks of death and re-admission for these groups.
Finally, HES data do not include information on interventions received by the adolescents during or after admissions, such as referral to mental health services. Effective interventions could have confounded the association between adversity-related injury and later harm. This confounding could have caused underestimation of the association between adversity-related injury and later harm if adolescents in the adversity group were more likely to receive effective interventions than those in the accident-related injury group. In practice, however, psychosocial assessments are routinely recommended only for adolescents with self-inflicted injury [11], and it is estimated that only 60% actually receive such an assessment [37].
Generalisability of the Study and Comparison with Other Findings
Our estimates of the relative increase in risks of death and emergency re-admission are likely to be generalisable to other hospitalised adolescent populations within the UK. However, generalisability to other countries and healthcare systems depends on the similarities of their populations of adolescents admitted with adversity-related injury to that of England. Generalisability also depends on the availability and intensity of psychosocial support for vulnerable adolescents after hospital discharge. Patterns of self-harm and drug/alcohol use during adolescence in other parts of Europe [4,38], but not in the US [39,40], have been shown to be similar to those in England.
Mortality rates in this study were either similar to or slightly higher than those reported for 14–24 y olds presenting with violent injury to the emergency department in the US [15]. The risk of violent death 2 y after a violent or drug/alcohol-related injury presentation (including non-admission) was 0.8/1,000. This figure is consistent with the risk of all causes of death 1 y after violent injury in our study (girls: 0.5/1,000; boys: 1.2/1,000). A prospective cohort study in England reported a mortality rate of 10/1,000 in 10–18 y olds followed for a median time period of 6 y after presentation to hospital for self-harm [14]. Our risks of mortality at 5 y after self-inflicted injury were similar (girls: 4.0/1,000; boys: 12.7/1,000).
Implications for Policy, Practice, and Research
Adolescents discharged from hospital after an adversity-related injury have substantially increased risks of death and emergency re-admission during the next 10 y compared with adolescents discharged after an accident-related injury; 10 y after discharge from hospital in England for an adversity-related injury, one in 52 boys and one in 90 girls aged 18–19 y will have died. These risks may be underestimated because of under-recording of adversity in hospital discharge records.
The risk of future harm was increased after all types of adversity-related injury. These findings justify extending national policy for psychosocial assessment after self-inflicted injury to all types of adversity-related injury. Consideration of psychological and social circumstances is good clinical practice, particularly for vulnerable adolescents. However, extending mandated psychosocial assessment from self-inflicted injury to all three types of adversity-related injury may have implications for services, as injured young people aged 16 y or older are often managed on adult surgical wards in the NHS, where expertise in psychosocial assessment and support for young people may be limited. Those who are male, older, have an underlying chronic condition, or are from deprived areas, and those exposed to multiple types adversity (e.g., drug/alcohol misuse and self-harm) have the highest risks of future harm (Table A7 in S1 Text; S1 Fig). Whether interventions should be targeted at these groups requires evidence of the effectiveness, feasibility, and cost-effectiveness of interventions.
There is a lack of evidence regarding effective interventions to reduce the risk of future harm in adolescents exposed to adversity-related injury. Our confirmation that there are increased long-term risks for these adolescents highlights the need to develop and evaluate interventions. Although some interventions in the UK for self-inflicted injury have shown positive effects, these were in samples too small to provide conclusive results [3]. Brief psychosocial interventions to address violent behaviour or alcohol misuse [41–47] have shown promise for improving outcomes and for cost-effectiveness [41,48,49], but follow-up was limited to 18 mo. In addition, these interventions have been evaluated predominantly in the US, where there are cultural differences in violence and drinking behaviours, healthcare systems, and social welfare support.
Supporting Information
Zdroje
1. Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, et al. (2012) Adolescence and the social determinants of health. Lancet 379 : 1641–1652. doi: 10.1016/S0140-6736(12)60149-4 22538179
2. Currie C, Zanotti C, Morgan A, Currie D, de Looze M, et al. (2012) Social determinants of health and well-being among young people. Health Behaviour in School-Aged Children (HBSC) study: international report from the 2009/2010 survey. Copenhagen: WHO Regional Office for Europe.
3. Hawton K, Saunders KE, O’Connor RC (2012) Self-harm and suicide in adolescents. Lancet 379 : 2373–2382. doi: 10.1016/S0140-6736(12)60322-5 22726518
4. Hibell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, et al. (2012) The 2011 ESPAD report: substance use among students in 36 European countries. Stockholm: Swedish Council for Information on Alcohol and Other Drugs.
5. Herbert A, Gilbert R, González-Izquierdo A, Li L (2015) Violence, self-harm and drug or alcohol misuse in adolescents admitted to hospitals in England for injury: a retrospective cohort study. BMJ Open 5:e006079. doi: 10.1136/bmjopen-2014-006079 25667148
6. Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D (2014) Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J Public Health (Oxf) 36 : 81–91.
7. Kelly-Irving M, Lepage B, Dedieu D, Bartley M, Blane D, et al. (2013) Adverse childhood experiences and premature all-cause mortality. Eur J Epidemiol 28 : 721–734. doi: 10.1007/s10654-013-9832-9 23887883
8. Barnett NP, Lebeau-Craven R, O’Leary TA, Colby SM, Rohsenow DJ, et al. (2002) Predictors of motivation to change after medical treatment for drinking-related events in adolescents. Psychol Addict Behav 16 : 106–112. 12079248
9. Johnson SB, Bradshaw CP, Wright JL, Haynie DL, Simons-Morton BG, et al. (2007) Characterizing the teachable moment: is an emergency department visit a teachable moment for intervention among assault-injured youth and their parents? Pediatr Emerg Care 23 : 553–559. 17726415
10. Norton R, Kobusingye O (2013) Injuries. N Engl J Med 368 : 1723–1730. doi: 10.1056/NEJMra1109343 23635052
11. National Institute for Health and Clinical Excellence (2004) Self-harm. The short term physical and psychological management and secondary prevention of self-harm in primary and secondary care. NICE guideline 16. London: National Institute for Health and Clinical Excellence.
12. Pilling S, Strang J, Gerada C, National Institute for Health and Clinical Excellence (2007) Psychosocial interventions and opioid detoxification for drug misuse: summary of NICE guidance. BMJ 335 : 203–205. 17656545
13. National Institute for Health and Clinical Excellence (2011) Alcohol-use disorder: diagnosis, assessment and management of harmful drinking and alcohol dependence. NICE guideline 115. London: National Institute for Health and Clinical Excellence.
14. Hawton K, Bergen H, Kapur N, Cooper J, Steeg S, et al. (2012) Repetition of self-harm and suicide following self-harm in children and adolescents: findings from the Multicentre Study of Self-Harm in England. J Child Psychol Psychiatry 53 : 1212–1219. doi: 10.1111/j.1469-7610.2012.02559.x 22537181
15. Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, et al. (2015) Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr 169 : 63–70. doi: 10.1001/jamapediatrics.2014.1900 25365147
16. Health and Social Care Information Centre (2014) Hospital episode statistics. Leeds: Health and Social Care Information Centre. Available: http://www.hscic.gov.uk/hes. Accessed 28 August 2014.
17. The King’s Fund (2014) The UK private healthcare market. London: The King’s Fund.
18. Health and Social Care Information Centre (2010) Data dictionary: inpatients. Leeds: Health and Social Care Information Centre. Available: http://www.hscic.gov.uk/media/1358/HES-Hospital-Episode-Statistics-HES-Admitted-Patient-Data-Dictionary/pdf. Accessed 9 May 2013.
19. World Health Organization (2013) International classification of diseases–10th revision. Geneva: World Health Organization.
20. Medical Research Council, National Health Service Health Research Authority (2015) Do I need NHS REC approval? Available: http://hra-decisiontools.org.uk/ethics/. Accessed 18 September 2015.
21. Gonzalez-Izquierdo A, Ward A, Smith P, Walford C, Begent J, et al. (2014) Notifications for child safeguarding from an acute hospital in response to presentations to healthcare by parents. Child Care Health Dev 41 : 186–193. doi: 10.1111/cch.12134 24635011
22. Health and Social Care Information Centre (2011) A guide to linked mortality data from Hospital Episode Statistics and the Office of National Statistics. Leeds: Health and Social Care Information Centre. Available: http://www.hscic.gov.uk/media/11668/HES-ONS-Mortality-Data-Guide/pdf/hes_ons__mortality_data_guide.pdf. Accessed 2 May 2013.
23. Health and Social Care Information Centre (2014) Methodology for creation of the HES patient ID (HESID). Leeds: Health and Social Care Information Centre.
24. Hale DR, Viner RM (2013) Risk behaviour and gender, socioeconomic status and ethnicity: exploring a key component of health inequality in adolescence. J Adolesc Health 52: S97–S98.
25. Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF (2003) The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med 37 : 268–277. 12914833
26. Hardelid P, Dattani N, Davey J, Pribramska I, Gilbert R (2013) Overview of child deaths in the four UK countries. London: Royal College of Paediatrics and Child Health. Available: http://www.rcpch.ac.uk/system/files/protected/page/CHRUK_Module%20A%20low%20res%20(2).pdf. Accessed 31 October 2013.
27. Rodham K, Hawton K, Evans E, Weatherall R (2005) Ethnic and gender differences in drinking, smoking and drug taking among adolescents in England: a self-report school-based survey of 15 and 16 year olds. J Adolesc 28 : 63–73. 15683635
28. Office of the Deputy Prime Minister (2010) Index of multiple deprivation 2004 [dataset]. Available: https://data.gov.uk/dataset/imd_2004. Accessed 24 November 2015.
29. Bellis MA, Hughes K, Wood S, Wyke S, Perkins C (2011) National five-year examination of inequalities and trends in emergency hospital admission for violence across England. Inj Prev 17 : 319–325. doi: 10.1136/ip.2010.030486 21393417
30. Office for National Statistics (2014) England and Wales, National life tables, 1980–82 to 2011–13. Available: http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-365199. Accessed 29 November 2015.
31. Cleves MA (2010) An introduction to survival analysis using Stata. College Station (Texas): Stata.
32. Scott D, Tonmyr L, Fraser J, Walker S, McKenzie K (2009) The utility and challenges of using ICD codes in child maltreatment research: a review of existing literature. Child Abuse Negl 33 : 791–808. doi: 10.1016/j.chiabu.2009.08.005 19853915
33. McKenzie K, Harrison JE, McClure RJ (2010) Identification of alcohol involvement in injury-related hospitalisations using routine data compared to medical record review. Aust N Z J Public Health 34 : 146–152. doi: 10.1111/j.1753-6405.2010.00499.x 23331358
34. Winn DG, Agran PF, Anderson CL (1995) Sensitivity of hospitals’ E-coded data in identifying causes of children’s violence-related injuries. Public Health Rep 110 : 277–281. 7610215
35. Colby SM, Barnett NP, Eaton CA, Spirito A, Woolard R, et al. (2002) Potential biases in case detection of alcohol involvement among adolescents in an emergency department. Pediatr Emerg Care 18 : 350–354. 12395005
36. Hagger-Johnson G, Harron K, Fleming T, Gilbert R, Goldstein H, et al. (2015) Data linkage errors in hospital administrative data when applying a pseudonymisation algorithm to paediatric intensive care records. BMJ Open 5: e008118. doi: 10.1136/bmjopen-2015-008118 26297363
37. Kapur N, Murphy E, Cooper J, Bergen H, Hawton K, Simkin S, et al. (2008) Psychosocial assessment following self-harm: results from the multi-centre monitoring of self-harm project. J Affect Disord 106 : 285–293. 17761308
38. Madge N, Hawton K, McMahon EM, Corcoran P, De Leo D, et al. (2011) Psychological characteristics, stressful life events and deliberate self-harm: findings from the Child & Adolescent Self-harm in Europe (CASE) Study. Eur Child Adolesc Psychiatry 20 : 499–508. doi: 10.1007/s00787-011-0210-4 21847620
39. Kalesan B, French C, Fagan JA, Fowler DL, Galea S (2014) Firearm-related hospitalizations and in-hospital mortality in the United States, 2000–2010. Am J Epidemiol 179 : 303–312. doi: 10.1093/aje/kwt255 24148708
40. Cherpitel CJ, Ye Y (2008) Trends in alcohol - and drug-related ED and primary care visits: data from three US National Surveys (1995–2005). Am J Drug Alcohol Abuse 34 : 576–583. doi: 10.1080/00952990802308189 18720270
41. Snider C, Lee J (2009) Youth violence secondary prevention initiatives in emergency departments: a systematic review. CJEM 11 : 161–168. 19272218
42. Patton R, Deluca P, Kaner E, Newbury-Birch D, Phillips T, et al. (2014) Alcohol screening and brief intervention for adolescents: the how, what and where of reducing alcohol consumption and related harm among young people. Alcohol 49 : 207–212.
43. Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, et al. (2013) Protecting adolescents from self-harm: a critical review of intervention studies. J Am Acad Child Adolesc Psychiatry 52 : 1260–1271. doi: 10.1016/j.jaac.2013.09.009 24290459
44. Zun LS, Downey LV, Rosen J (2006) The effectiveness of an ED-based violence prevention program. Am J Emerg Med 24 : 8–13. 16338502
45. King CA, Kramer A, Preuss L, Kerr DC, Weisse L, et al. (2006) Youth-Nominated Support Team for Suicidal Adolescents (Version 1): a randomized controlled trial. J Consult Clin Psychol 74 : 199–206. 16551158
46. Violence Reduction Unit (2010) The violence must stop: Glasgow’s community initiative to reduce violence. Second year report. Strathclyde: Violence Reduction Unit.
47. Tait RJ, Hulse GK, Robertson SI (2004) Effectiveness of a brief-intervention and continuity of care in enhancing attendance for treatment by adolescent substance users. Drug Alcohol Depend 74 : 289–296. 15194207
48. Neville FG, Goodall CA, Williams DJ, Donnelly PD (2014) Violence brief interventions: a rapid review. Aggress Violent Behav 19 : 692–698.
49. Crawford MJ, Patton R, Touquet R, Drummond C, Byford S, et al. (2004) Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. Lancet 364 : 1334–1339. 15474136
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2015 Číslo 12- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Risks and Benefits of Nalmefene in the Treatment of Adult Alcohol Dependence: A Systematic Literature Review and Meta-Analysis of Published and Unpublished Double-Blind Randomized Controlled Trials
- Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled
- Police Killings and Police Deaths Are Public Health Data and Can Be Counted
- A Successful Failure: Missing the MDG4 Target for Under-Five Mortality in South Africa
- The Ebola Vaccine, Iatrogenic Injuries, and Legal Liability
- Progress in Medicine: Experts Take Stock
- Use of Viremia to Evaluate the Baseline Case Fatality Ratio of Ebola Virus Disease and Inform Treatment Studies: A Retrospective Cohort Study
- Acute Cardiovascular Events after Herpes Zoster: A Self-Controlled Case Series Analysis in Vaccinated and Unvaccinated Older Residents of the United States
- Moving Beyond “Food Deserts”: Reorienting United States Policies to Reduce Disparities in Diet Quality
- Public Health and International Partnerships in the Democratic People’s Republic of Korea
- Self-Administered Outpatient Antimicrobial Infusion by Uninsured Patients Discharged from a Safety-Net Hospital: A Propensity-Score-Balanced Retrospective Cohort Study
- Association between Regimen Composition and Treatment Response in Patients with Multidrug-Resistant Tuberculosis: A Prospective Cohort Study
- 10-y Risks of Death and Emergency Re-admission in Adolescents Hospitalised with Violent, Drug- or Alcohol-Related, or Self-Inflicted Injury: A Population-Based Cohort Study
- World Health Organization Global Estimates and Regional Comparisons of the Burden of Foodborne Disease in 2010
- Bariatric Surgery in the United Kingdom: A Cohort Study of Weight Loss and Clinical Outcomes in Routine Clinical Care
- Traditional and Emerging Lifestyle Risk Behaviors and All-Cause Mortality in Middle-Aged and Older Adults: Evidence from a Large Population-Based Australian Cohort
- Inequalities in Alcohol-Related Mortality in 17 European Countries: A Retrospective Analysis of Mortality Registers
- World Health Organization Estimates of the Global and Regional Disease Burden of 11 Foodborne Parasitic Diseases, 2010: A Data Synthesis
- A Molecular Host Response Assay to Discriminate Between Sepsis and Infection-Negative Systemic Inflammation in Critically Ill Patients: Discovery and Validation in Independent Cohorts
- World Health Organization Estimates of the Global and Regional Disease Burden of 22 Foodborne Bacterial, Protozoal, and Viral Diseases, 2010: A Data Synthesis
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Self-Administered Outpatient Antimicrobial Infusion by Uninsured Patients Discharged from a Safety-Net Hospital: A Propensity-Score-Balanced Retrospective Cohort Study
- Risks and Benefits of Nalmefene in the Treatment of Adult Alcohol Dependence: A Systematic Literature Review and Meta-Analysis of Published and Unpublished Double-Blind Randomized Controlled Trials
- World Health Organization Global Estimates and Regional Comparisons of the Burden of Foodborne Disease in 2010
- Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



