-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Population Approaches to Prevention of Type 2 Diabetes
Martin White argues that whole population interventions will be needed in addition to those targeted to people at high risk in order to respond to the global challenge of type 2 diabetes.
Published in the journal: Population Approaches to Prevention of Type 2 Diabetes. PLoS Med 13(7): e32767. doi:10.1371/journal.pmed.1002080
Category: Perspective
doi: https://doi.org/10.1371/journal.pmed.1002080Summary
Martin White argues that whole population interventions will be needed in addition to those targeted to people at high risk in order to respond to the global challenge of type 2 diabetes.
With the prevalence of Type 2 Diabetes Mellitus (T2DM) continuing to rise in most high-income, low-income, and middle-income countries [1], strategies to stem the emerging pandemic are urgently needed. To date, the best evidence for prevention of T2DM comes from randomized controlled trials of lifestyle interventions (e.g., to modify diet and physical activity and achieve weight loss) delivered to individuals at high risk, usually those with impaired glucose tolerance or prediabetes [2]. However, strategies that focus on changing individual behavior have limited reach due to the challenges of identifying at scale those in whom an intervention may be beneficial. Thus, while the behavioral interventions themselves have been shown to be meet acceptable cost-effectiveness thresholds, the cost-effectiveness of both identifying and intervening at the scale needed to achieve population impact remains less clear [3]. It is likely that, in the short term, such strategies will be unaffordable by all but the most affluent nations. Demonstration projects attempting to identify and deliver interventions to all those at high risk in the population (estimated to be >10% of adults in England, for example), such as the NHS Diabetes Prevention Programme, will therefore be watched with interest [4].
Behavioral interventions targeting individuals can also have variable effectiveness across population subgroups due to differential access, uptake, and compliance, resulting in lesser benefits in people from socioeconomically disadvantaged backgrounds [5]. Such interventions could therefore widen inequalities in incidence and prevalence of T2DM [6]. Such strategies will be of value to help stem the tide of new cases of T2DM but realistically need to be accompanied by more affordable and wider reaching population-level interventions to change diet and physical activity, reduce obesity, and thus reduce incidence of T2DM. Population intervention strategies will be particularly important for low-income and middle-income countries, for whom individual-level interventions may be unaffordable [7]. Such approaches have been advocated by WHO, which calls for “multisectoral action that simultaneously addresses different sectors that contribute to the production, distribution, and marketing of food, while concurrently shaping an environment that facilitates and promotes adequate levels of physical activity” [8].
Population approaches to prevention aim to reduce key risk factors for T2DM in the whole population, irrespective of individual level of risk. They achieve this by bringing about small changes in risk factor levels in the whole population, resulting in a shift in the population distribution of risk. Such shifts in the distribution of disease risk can theoretically lead to substantial population benefit [9], and the principle has been well demonstrated in relation to, for example, salt consumption and blood pressure [10]. Such approaches may not be entirely without harm, however. For example, not everyone in a population needs to reduce weight, reduce blood pressure, or become more active [11]. But given the small expected change in risk at an individual level, and their delivery in a societal context, population interventions are generally considered safe [9].
There are potential concerns also about the differential effectiveness of some population interventions. Not all population-level interventions are likely to have the same impact, and some may be less equitable than others. This is a particular concern for interventions that require a higher level of engagement by individuals, such as food labelling, which demands literacy and numeracy as well as an ability to process and apply the information presented in making healthy food choices, often from a bewildering array of available products [12]. Interventions requiring low levels of individual engagement, such as regulation of TV advertising of unhealthy foods, may be more equitable and offer greater overall health impacts. However, such policy interventions need to be formulated to ensure population benefit and be rigorously evaluated [13].
Simulation studies have modelled the potential impacts on T2DM incidence of small changes in risk factors for T2DM, such as physical activity at a population level, demonstrating significant potential benefits [14]. The challenge is to develop and deliver interventions that can bring about such small changes across the whole population cost-effectively. Is this achievable and, if so, how?
Population level interventions can be delivered via a range of modalities. Each is underpinned by a policy measure (e.g., a law or voluntary agreement) and involves a mechanism to achieve change in risk exposure. The mechanisms are diverse and include, for example, reformulation of foods (e.g., to reduce sugar content), provision of information (e.g., food labelling), fiscal measures (e.g., taxes on less healthy food products), or structural and environmental measures (e.g., new infrastructure for active commuting, such as cycle lanes). These can usefully be categorized as technology, education, or resource-based and sometimes involve combinations of these modalities (Table 1).
Tab. 1. Potential examples of population level interventions to change diet and physical activity behaviors, by principal modality. 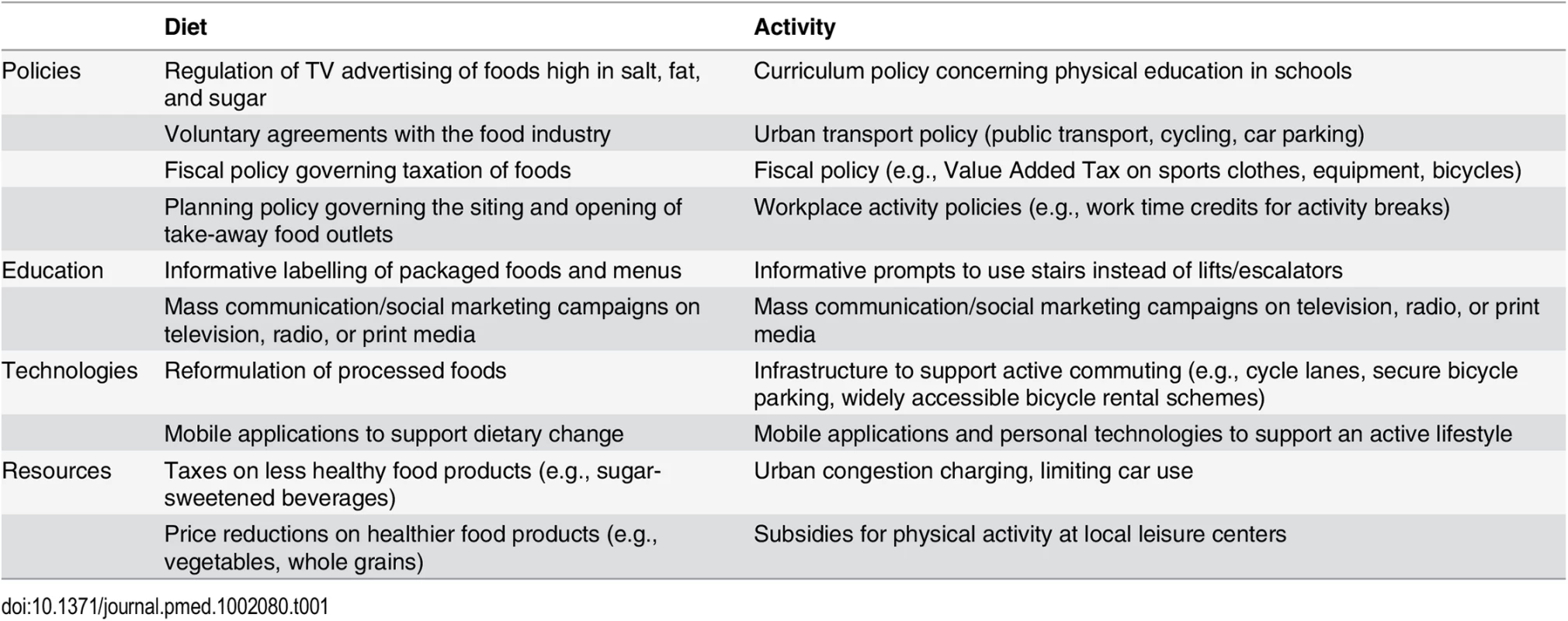
Many such interventions have been implemented with apparent success [15–17]. While the primary aim has usually not been T2DM prevention specifically, their contributions to this goal may be considerable. For example, an evaluation of a new guided busway in Cambridgeshire, United Kingdom, found that it resulted in an increase in active commuting; participants living 4 km from the busway were one-third more likely to have increased their cycle commuting between 2009 and 2012 than those living 9 km away, reporting a mean increase of 87 minutes of cycling per week [18]. Similarly, early evaluation of the tax on sugar-sweetened beverages in Mexico suggests a decrease in purchases of taxed beverages and an increase in purchases of untaxed beverages [19]. Some evidence suggests that exposure to favorable diet and physical activity environments, such as healthy food provision and physical activity resources at neighborhood level, may have measureable effects on T2DM incidence [20]. In these intervention examples, it is possible that planned environmental changes will impact total activity level, or total sugar and energy consumption, with potentially important consequences for body mass, glucose regulation, and associated health outcomes at a population level.
Evaluating the impact of population-level preventive interventions on health outcomes is a challenging long-term goal that needs investment in routine data systems, data linkage, and new paradigms of experimental research that are able to capture impacts across a range of potential outcomes at a system level, taking into account their contextual complexity. The challenges of such evaluations have been helped considerably by methodological developments in recent years, which have been given prominence by guidance on evaluation of natural experiments from the UK Medical Research Council [21]. Nevertheless, evaluating population interventions is likely to continue to prove challenging, especially in countries with poorly developed routine heath information systems.
While rigorous science is needed to build the evidence base for population interventions, this alone will not be sufficient to ensure that the range of interventions needed to reshape population risk of T2DM is delivered by countries and regions. Such interventions are delivered in real world contexts by policy makers at local and national levels outside the control of researchers. Scientific evidence is just one of a number of inputs to the policy-making process, and political and economic considerations are usually of equal or greater importance [22,23]. Research thus needs to focus on these too, identifying, in particular, the economic case for such interventions, not just in terms of cost-savings to health systems, but also in terms of the wider benefits to society from reduced morbidity, including improved employment prospects and economic productivity.
The global challenges of obesity and T2DM are inextricably linked, and their scale and economic impact demand global action from political leaders. Interventions need to include both those targeted to people at high risk (to address the existing burden of prediabetes) and those aimed at whole populations (to reverse current upward trends). Solutions will need to be sensitive to context in low-income, middle-income, and high-income countries. Population interventions may prove the most viable options in resource-poor nations [7]. Bold policy decisions will need to be made to avert the economic and health crises that are the likely consequences of current trends in obesity and T2DM, since we cannot wait for perfect evidence [24].
Zdroje
1. NCD Risk Factor Collaboration (NCD-RisC) (2016) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387 : 1513–1530.
2. Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, et al. (2007) Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ 334 : 299. 17237299
3. Gillett M, Brennan A, Blake L, Payne N, Goyder L, et al. (2010) Prevention of type 2 diabetes: preventing pre-diabetes among adults in high-risk groups. Report on use of evidence from effectiveness reviews and cost-effectiveness modelling. London: NICE Public Health Collaborating Centre, School of Health and Related Research, University of Sheffield. 1–69 p.
4. Barry E, Roberts S, Finer S, Vijayaraghavan S, Greenhalgh T (2015) Time to question the NHS diabetes prevention programme. BMJ 351: h4717. doi: 10.1136/bmj.h4717 26346375
5. White M, Adams J, Heywood P (2009) How and why do interventions that increase health overall widen inequalities within populations? In: Babones S, editor. Health, inequality and society. Bristol: Policy Press.
6. National Institute for Health and Care Excellence (NICE) (2011) Type 2 diabetes prevention: population and community-level interventions. NICE guidelines [PH35]. London: NICE.
7. Unwin N, Whiting D, Roglic G (2010) Social determinants of diabetes and challenges of prevention. Lancet 375 : 2204–2205.
8. World Health Organization (2014) Global status report on noncommunicable diseases. Geneva: World Health Organization.
9. Rose G, Khaw KT, Marmot M (2008) Rose's strategy of preventive medicine. Oxford: Oxford University Press.
10. He FJ, MacGregor GA (2002) Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens 16 : 761–770. 12444537
11. Adams J, White M (2005) When the population approach to prevention puts the health of individuals at risk. Int J Epidemiol 34 : 40–43. 15256526
12. Adams J, Mytton O, White M, Monsivais P (2016) Why Are Some Population Interventions for Diet and Obesity More Equitable and Effective Than Others? The Role of Individual Agency. PLoS Med 13: e1001990. doi: 10.1371/journal.pmed.1001990 27046234
13. Adams J, Tyrrell R, Adamson AJ, White M (2012) Effect of Restrictions on Television Food Advertising to Children on Exposure to Advertisements for 'Less Healthy' Foods: Repeat Cross-Sectional Study. PLoS ONE 7: e31578. doi: 10.1371/journal.pone.0031578 22355376
14. Woodcock J, Tainio M, Cheshire J, O’Brien O, Goodman A (2014) Health effects of the London bicycle sharing system: health impact modelling study. BMJ 348: g425. doi: 10.1136/bmj.g425 24524928
15. Laine J, Kuvaja-Köllner V, Pietilä E, Koivuneva M, Valtonen H, et al. (2014) Cost-Effectiveness of Population-Level Physical Activity Interventions: A Systematic Review. Am J Health Promot 29 : 71–80. doi: 10.4278/ajhp.131210-LIT-622 25361461
16. McGill R, Anwar E, Orton L, Bromley H, Lloyd-Williams F, et al. (2015) Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 15 : 1–15.
17. Thorogood M, Simera I, Dowler E, Summerbell C, Brunner E (2007) A systematic review of population and community dietary interventions to prevent cancer. Nutr Res Rev 20 : 74–88. doi: 10.1017/S0954422407733073 19079861
18. Ogilvie D, Panter J, Guell C, Jones A, Mackett R, et al. (2016) Health impacts of the Cambridgeshire Guided Busway: a natural experimental study. Public Health Research 4(1).
19. Colchero MA, Popkin BM, Rivera JA, Ng SW (2016) Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ 352: h6704. doi: 10.1136/bmj.h6704 26738745
20. Christine PJ, Auchincloss AH, Bertoni AG, Carnethon MR, Sánchez BN, et al. (2015) Longitudinal associations between neighborhood physical and social environments and incident type 2 diabetes mellitus: The multi-ethnic study of atherosclerosis (mesa). JAMA Intern Med 175 : 1311–1320. doi: 10.1001/jamainternmed.2015.2691 26121402
21. Craig P, Cooper C, Gunnell D, Haw S, Lawson K, et al. (2012) Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health 66 : 1182–1186. doi: 10.1136/jech-2011-200375 22577181
22. Tyler C (2013) Top 20 things scientists need to know about policy-making. The Guardian, 2nd December. London: Guardian News and Media Ltd.
23. Oliver KA, de Vocht F (2015) Defining ‘evidence’ in public health: a survey of policymakers’ uses and preferences. Eur J Public Health 7: CVK082. doi: 10.1093/eurpub/ckv082 26163467
24. Whitty CMJ (2015) What makes an academic paper useful for health policy? BMC Medicine 13 : 1–5.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2016 Číslo 7- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- The Clinical and Public Health Challenges of Diabetes Prevention: A Search for Sustainable Solutions
- Screening for Dysglycemia: Connecting Supply and Demand to Slow Growth in Diabetes Incidence
- Diabetes: A Cinderella Subject We Can’t Afford to Ignore
- Prescribing Exercise and Lifestyle Training for High Risk Women in Pregnancy and Early Post-partum—Is It Worth It?
- Population Approaches to Prevention of Type 2 Diabetes
- First-Year Evaluation of Mexico’s Tax on Nonessential Energy-Dense Foods: An Observational Study
- Effects of Saturated Fat, Polyunsaturated Fat, Monounsaturated Fat, and Carbohydrate on Glucose-Insulin Homeostasis: A Systematic Review and Meta-analysis of Randomised Controlled Feeding Trials
- Leveraging Genetics to Advance Type 2 Diabetes Prevention
- Cardiometabolic Risk Factor Changes Observed in Diabetes Prevention Programs in US Settings: A Systematic Review and Meta-analysis
- Risks and Population Burden of Cardiovascular Diseases Associated with Diabetes in China: A Prospective Study of 0.5 Million Adults
- Dietary Diversity, Diet Cost, and Incidence of Type 2 Diabetes in the United Kingdom: A Prospective Cohort Study
- Detecting Dysglycemia Using the 2015 United States Preventive Services Task Force Screening Criteria: A Cohort Analysis of Community Health Center Patients
- Exercise Training and Weight Gain in Obese Pregnant Women: A Randomized Controlled Trial (ETIP Trial)
- Associations between Recreational and Commuter Cycling, Changes in Cycling, and Type 2 Diabetes Risk: A Cohort Study of Danish Men and Women
- Association of Plasma Phospholipid n-3 and n-6 Polyunsaturated Fatty Acids with Type 2 Diabetes: The EPIC-InterAct Case-Cohort Study
- Engagement, Retention, and Progression to Type 2 Diabetes: A Retrospective Analysis of the Cluster-Randomised "Let's Prevent Diabetes" Trial
- Obesity and Life Expectancy with and without Diabetes in Adults Aged 55 Years and Older in the Netherlands: A Prospective Cohort Study
- Supported Telemonitoring and Glycemic Control in People with Type 2 Diabetes: The Telescot Diabetes Pragmatic Multicenter Randomized Controlled Trial
- Mothers after Gestational Diabetes in Australia (MAGDA): A Randomised Controlled Trial of a Postnatal Diabetes Prevention Program
- Cycling and Diabetes Prevention: Practice-Based Evidence for Public Health Action
- Consumption of Meals Prepared at Home and Risk of Type 2 Diabetes: An Analysis of Two Prospective Cohort Studies
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Mothers after Gestational Diabetes in Australia (MAGDA): A Randomised Controlled Trial of a Postnatal Diabetes Prevention Program
- Consumption of Meals Prepared at Home and Risk of Type 2 Diabetes: An Analysis of Two Prospective Cohort Studies
- Obesity and Life Expectancy with and without Diabetes in Adults Aged 55 Years and Older in the Netherlands: A Prospective Cohort Study
- Effects of Saturated Fat, Polyunsaturated Fat, Monounsaturated Fat, and Carbohydrate on Glucose-Insulin Homeostasis: A Systematic Review and Meta-analysis of Randomised Controlled Feeding Trials
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



