Determination of the adequate vascular perfusion time of cross-leg free latissimus dorsi myocutaneous flaps in reconstruction of complex lower extremity defects
Authors:
Elyounsi M. 1; Ali M. 2; Makboul M. 1; Asklany A. 1; El-Shazly M. 1
Authors‘ workplace:
Department of Plastic Surgery, Assiut University Hospitals, Egypt
1; Department of Orthopedics, Assiut University Hospitals, Egypt
2
Published in:
ACTA CHIRURGIAE PLASTICAE, 64, 3-4, 2022, pp. 124-128
doi:
https://doi.org/10.48095/ccachp2022124
Introduction
The management of defects of the lower leg is a complex problem especially when they are large with deep soft tissue loss. In such cases, it is difficult to cover the defect with a local skin flap, a distant skin flap or even a conventional free flap because of the compromised recipient vessels [1–5]. The widespread use of free flaps had made it possible to repair these complex defects. A successful repair is achieved not only by appropriate convenient flap planning by an experienced microsurgery team, but also by identifying the suitable donor vessels which could not be frequently found when joints, tendons, nerves, or vessels are open or where fracture lines and bone defects accompany periosteal bone structures [6].
The use of long venous grafts or A-V loops as solutions for these challenging cases may not be easy or preferred to vascularize free flaps away from the zone of injury as it requires another donor site and increases the number of vascular anastomoses which in turn increases the risk of thrombosis and failure of the free flap. An arterial jump graft from the ipsilateral popliteal artery is another option for reconstruction of the defect at the same leg but there is a possibility of kinking of the grafts and stenosis of the distal anastomosis [7].
In such cases, the vascular pedicle of the free flap could be anastomosed to the recipient vessels in the contralateral healthy leg temporarily and then divided after adequate neo-vascularization of the flap from the wound bed, hence the name ''cross leg free flap'', first described by Taylor et al in 1979 using an osteocutaneous iliac flap [8].
However, since that time, no reports had tried to reach a scientific calculation and/or assessment of the needed time to have the full vascular perfusion of these flaps. The timing of the second surgical stage for division of such cross-pedicles is still to date a subjective evaluation. Those patients usually have critical general conditions and challenging local wounds and should not have more risks for complete or partial necrosis of these unusual free flaps. The hypothesis of this work is to investigate the ideal time to divide such pedicles to have the maximum success rate possible for these challenging conditions and procedures.
Patients and methods
This study was performed in the period from February 2017 to June 2021 for patients who had cross-leg free latissimus dorsi flaps for reconstruction of soft tissue defects of the lower limbs – as shown in Fig. 2 and 3 – at the Department of Plastic and Reconstructive Surgery, Assiut University, Egypt. The study included 16 patients (10 males and 6 females) with a mean age of 27.4 years (range 7–39) who did not have a suitable adjacent recipient vessel for conventional free flap reconstruction.


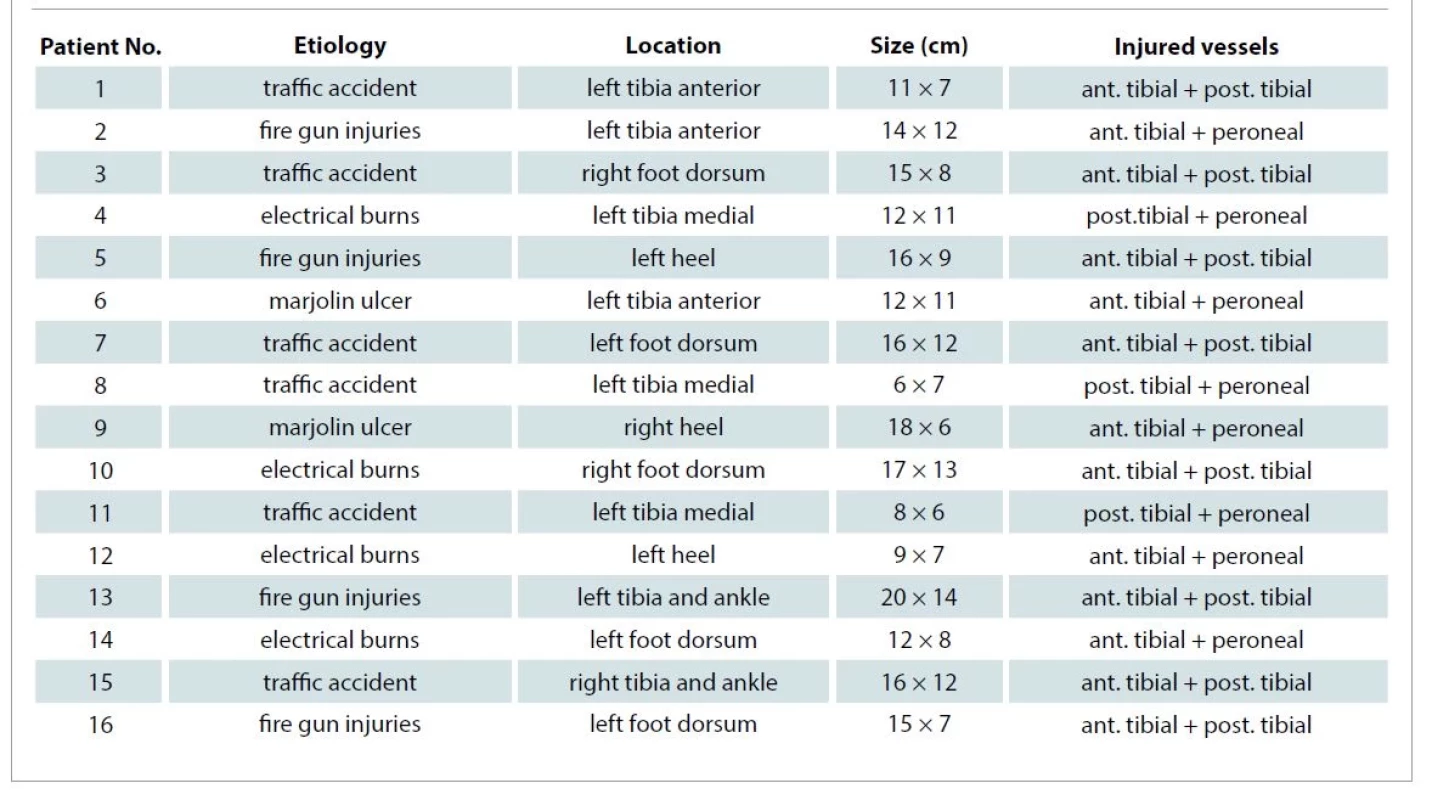
The etiology of the injuries consisted of traffic accidents in 6 patients, fire gun injuries in 4 patients, electrical burns in 4 patients, and Marjolijn ulcer in 2 patients. The mean soft tissue defect dimension was 12 × 11 cm (the smallest: 6 × 7 cm; the largest: 20 × 14 cm). Gustilo type 3B tibial fractures present in 12 patients, while no fractures were present in the other 4 patients.
Tab. 1 shows the defects’ etiology, location, size and the injured vessels.
Preoperatively, arterial angiography was performed for all patients. Intraoperatively, the posterior tibial vessels of the contralateral leg were exposed as recipient vessels via H-shaped skin incision on the medial side of the leg. The vascular pedicle of the myocutaneous latissimus dorsi flap, combining with the subscapular and circumflex scapular vessels, forms a T-shaped vascular pedicle.
Both lower extremities were fixed using external fixators to maintain immobilization for 4–6 weeks. End to end anastomosis was performed to the posterior tibial artery and vein of the contralateral leg. All patients were hospitalized during this period.
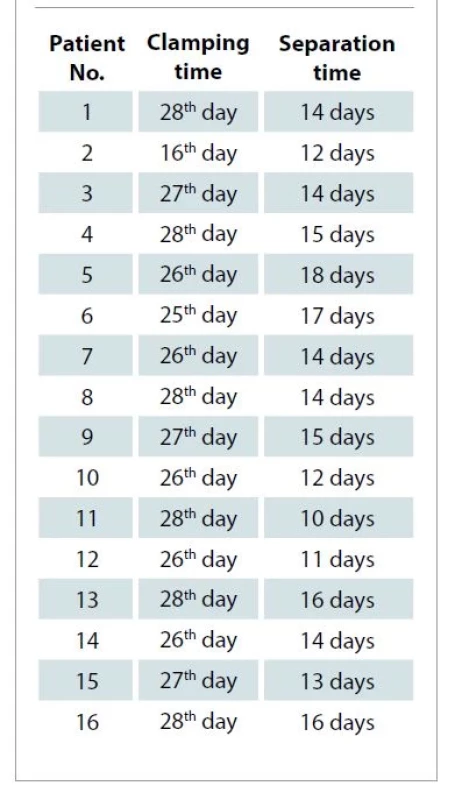
The patients were managed with a prophylactic low dose of heparin to guard against deep venous thrombosis due to the long recumbency time. After the fourth week post-operatively, fine vascular tourniquet was applied around the pedicle for 15 minutes. The clamping time was increased by 15 minutes on each consequent day in cases with good flap vascularity but in cases of diminished vascularity we released the clamp and started again next day with the same clamping time and force till reaching fresh blood through a needle prick test. On the last 2 days before the separation, the pedicle was clamped for 2 hours continuously as shown in Fig. 3, and the flap vascularity was assessed by a needle prick test. The bright red blood bleeding in the distal part of the flap was noted as a sign of sufficient circulation and full neo-vascularization. Tab. 2 shows the clamping and separation time of each flap.

Results
Sixteen cross-leg free latissimus dorsi flap transfers were performed. Fourteen flaps survived completely, and two flaps developed distal flap necrosis which was managed by split thickness skin graft later. We found that the two flaps with distal necrosis had been separated at earlier time three weeks ago, so we prefer not to start clamping before the 4th 4th and to continue clamping for about a two-week interval before separation; the pedicle was divided in the 5–6th weeks.
Minor infection had been observed in the recipient site in two cases which were successfully managed with more frequent dressings and aggressive antibiotics. Seroma occurred in the donor area in two cases. No pathology associated with the bone union had been observed in the patients with bone fractures. Satisfactory cosmetic results in the reconstructed areas and equal limb lengths were achieved in all patients.
Discussion
Once free flap reconstruction is planned for a challenging soft tissue defect, there would be limited options for the flap inset and donor vessels in cases of unsuitable conventional vascular anastomoses. Lin et al reported a case series of 65 traumatic limb injuries reconstructed with free tissue transfers using vein grafts of significant length (> 20 cm for the arterial gap). They used vein grafts for arterial defects, and a temporary arteriovenous loop in the case of both artery and vein defect. They observed a higher re-exploration rate associated with greater graft length, although this did not achieve statistical significance [9].
The “cross-leg free flap,” first described by Taylor et al in 1979 was used to repair skin and bone defects in the lower leg with a free osteocutaneous flap. Various successful results have been published later using the cross-leg method. Yu et al published a case series of 85 patients using the cross-bridge method and reported a success rate of 95.29% [10]. The advantages of reconstruction with cross-leg free flaps include the possibility of preparation with the required tissue components such as bone and muscle of the requisite sizes and allowing the anastomosis line to be completely outside the trauma zone. The most important advantage of the cross-leg free flap is the possibility of saving the limb by transferring well-vascularized tissue to the leg in injuries with serious defects, even when amputation is considered. This method is especially suitable for patients with sensation in the soles of the feet and with a stable bone skeleton [11].
In this work, we applied the cross leg free latissimus dorsi flaps and applied external fixators for leg stabilization. Separation time of the cross-leg free flap vascular pedicle depends on the tissues included in the flap (muscle or fasciocutaneous), the size, and the recipient bed condition. One experimental study with 25 dogs demonstrated that approximately a period of 3 weeks is sufficient to establish revascularization of a random pedicled flap.
In this series, we started clamping the flap pedicle 4 weeks after the first operation in all cases (except those with distal flap ischemia) and continue to increase clamping time by 15 minutes daily with monitoring the vascularity on each clamping trial regularly. During the surgery, clamps were placed on the pedicles to confirm flap circulation. No problems in flap circulation after clamp application were observed in any of the cases. We prefer not to start clamping before the fourth week and to continue clamping for about a two-week interval before separation.
Conclusion
Microvascular free tissue reconstructions for lower leg, heel, and foot are invaluable methods for the common complex wounds in these areas [12,13]. In this retrospective cohort study, we reported our experience treating a wide range of lower limb defects with cross leg latissimus dorsi myocutaneous flaps and assessed the ideal time to divide the crossed vascular pedicles to have the maximum success rate possible for these challenging conditions and procedures.
Our message from this research is to ensure adequate vascularity to the cross leg latissimus dorsi myocutaneous flaps by clamping the pedicle before separation and to determine the optimal time of this critical step which found to be ideal between 5–6th week after anastomoses of the pedicle with the recipient vessels.
Clamping trials on consequent days with increasing time intervals in each trial is a fundamental adjunctive procedure to determine the optimal timing at which we can safely separate such critical flaps which are different from ordinary free flaps.
Roles of authors
Mohamed Elyounsi and Awny Asklany: collection the data and clinical search and performing the analysis;
Mugahed Ali: conception and design of the study;
Mohamed Makboul: collection the data and clinical search, performing the analysis, writing the article with final approval of the version to be published;
Mohamed El-Shazly: conception and design of the study, writing the article and performing the final approval of the version to be published.
Mohamed El-Shazly, MMBCh, MSc, PhD, MD
Chairman of Plastic Surgery Department
Assiut University Hospitals
Egypt
e-mail: elshazly@aun.edu.eg
Submitted: 19. 3. 2022
Accepted: 1. 11. 2022
Sources
1. Scott LL., Baumeister S. Lower extremity. In: Wei FC, Mardini S (eds). Flaps and Reconstructive Surgery. Philadelphia, PA: Saunders 2009: 62–70.
2. Economides JM., Patel KM., Evans KK., et al. Systematic review of patient-centered outcomes following lower extremity flap reconstruction in comorbid patients. J Reconstr Microsurg. 2013, 29(5): 307–316.
3. Cho EH., Garcia RM., Blau J., et al. Microvascular anastomoses using end-to-end versus end-to-side technique in lower extremity free tissue transfer. J Reconstr Microsurg. 2016, 32(2): 114–120.
4. Kolbenschlag J., Hellmich S., Germann G., et al. Free tissue transfer in patients with severe peripheral arterial disease: functional outcome in reconstruction of chronic lower extremity defects. J Reconstr Microsurg. 2013, 29(9): 607–614.
5. Fischer JP., Wink JD., Nelson JA., et al. A retrospective review of outcomes and flap selection in free tissue transfers for complex lower extremity reconstruction. J Reconstr Microsurg. 2013, 29(6): 407–416.
6. Akyürek M., Safak T., Ozkan O., et al. Technique to re-establish continuity of the recipient artery after end-to-end anastomoses in cross-leg free flap procedure. Ann Plast Surg. 2002, 49(4): 430–433.
7. Boontje AH. Occlusion of femoropopliteal bypasses (Biografts). J Cardiovasc Surg. 1984, 25(5): 385–389.
8. Taylor GI., Townsend P., Corlett R. Superiority of the deep circumflex iliac vessels as the supply for free groin flaps. Clinical work. Plast Reconstr Surg. 1979, 64(6): 745–759.
9. Lin CH., Mardini S., Lin YT., et al. Sixty-five clinical cases of free tissue transfer using long arteriovenous fistulas or vein grafts. J Trauma. 2004, 56(5): 1107–1117.
10. Yu ZJ., Huang MJ., Zheng L. Influence of pedicle severance at different time on the survival of canine skin flap. Chin Med J. 1984, 64: 449.
11. Pei GX., Xie CP., Li QD. Musculocutaneous flap transfer bridged by the posterior tibial vessels from the healthy limb in the reconstruction of severe lower limb trauma. Chin J Traumatol. 1992, 8: 266.
12. El-Shazly M., Makboul M. Microsurgical free tissue transfers as a valuable reconstructive procedure in foot reconstruction. Indian J Plast Surg. 2007, 40: 141–146.
13. El-Shazly M., Yassin O., Kamal A., et al. Soft tissue defects of the heel: a surgical reconstruction algorithm based on a retrospective cohort study. J Foot Ankle Surg. 2008, 47(2): 145–152.
Labels
Plastic surgery Orthopaedics Burns medicine TraumatologyArticle was published in
Acta chirurgiae plasticae

2022 Issue 3-4
- Metamizole vs. Tramadol in Postoperative Analgesia
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Current Insights into the Antispasmodic and Analgesic Effects of Metamizole on the Gastrointestinal Tract
- Obstacle Called Vasospasm: Which Solution Is Most Effective in Microsurgery and How to Pharmacologically Assist It?
- Spasmolytic Effect of Metamizole
Most read in this issue
- Mini-invasive technique of sclerotherapy with talc in chronic seroma after abdominoplasty – a case report and literature review
- Multifarious uses of the pedicled SCIP flap – a case series
- Evaluation of resection margins in oral squamous cell carcinoma
- Preservation of supraclavicular nerve while harvesting supraclavicular lymph node flap
