Multifarious uses of the pedicled SCIP flap – a case series
Authors:
Adhikari S.; Bhattacharya D.
Authors‘ workplace:
Institute of Post Graduate Medical Education & Research, Kolkata, West Bengal, India
Published in:
ACTA CHIRURGIAE PLASTICAE, 64, 3-4, 2022, pp. 148-154
doi:
https://doi.org/10.48095/ccachp2022148
Introduction
The groin flap which is nourished by the superficial circumflex iliac artery (SCIA) has been the workhorse for plastic surgeons both as a pedicled flap and as a free flap. In fact, it was the first free flap that was successfully performed by Daniel and Taylor [1]. The primary advantages of the groin flap have been the availability of a large area of skin and the resultant scar after elevation, which lies in a hidden area making it especially popular in women and children. The free groin flap has then slowly lost popularity because of the anatomical variation of the SCIA, the short pedicle length, the mismatch between the donor and the recipient vessels and the availability of other technically easy free flaps [2–4].
After the development of perforator flaps, it became clear that the entire territory of the flap could be harvested based on small perforators and there was no need to dissect the entire flap based on the source major pedicle vessels [5]. The SCIP flap has evolved similarly from the groin flap in which the entire skin territory of the groin flap can be harvested based on the perforators of the SCIA and only a part of the SCIA can be taken along with. Anatomical studies have demonstrated that the SCIA divides into superficial and deep branches with the superficial branch running above the deep fascia of the sartorius muscle and the deep branch lying below it. The relationship between the calibre of the superficial and deep branches is reciprocal in most cases with the superficial branch being absent at times [6]. That is why a preoperative color doppler study should be instituted in order to depict the arterial anatomy of the SCIA [7].
Although the SCIP flap has been used mainly as a free flap for reconstruction in a variety of defects, the pedicled SCIP flap can also be utilized in a large number of cases and can even be used as a pedicled flap with lymphovenous anastomosis to restore lymphatic continuity [8]. Additionally, it has been used in penile and urethral reconstruction either alone or in combination with other flaps [9].
In this article we would like to describe the multifarious uses of the pedicled SCIP flap as have been performed in our patients. This is not a complete list of the uses of this flap and other uses would continue to evolve with time.
Patients and methods
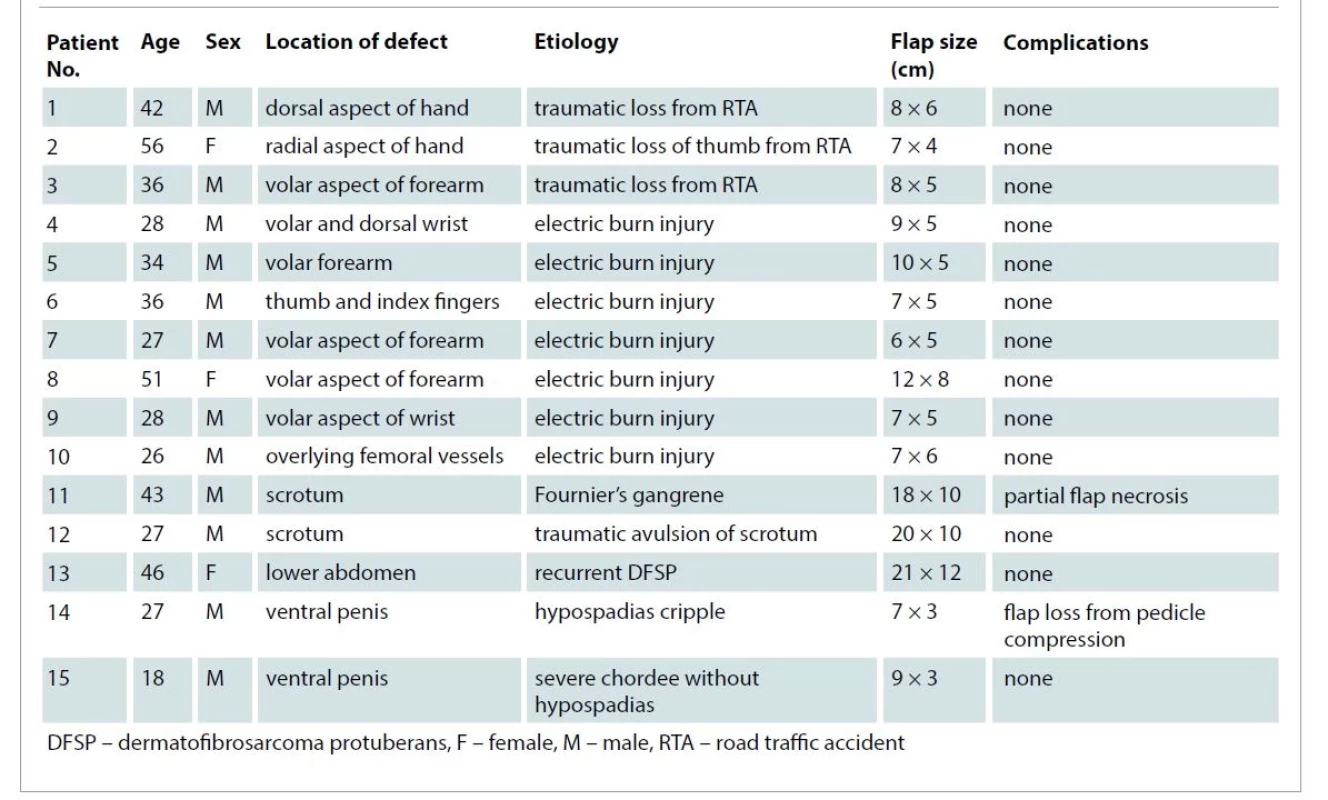
Between January 2022 to July 2022, 15 patients were operated on using the pedicled SCIP flap. Patients were informed about the surgery in details, the resultant scar and the possible management in the advent of complications and informed consent was obtained prior to the surgery. For patients who were subjected to reconstruction of the hand/forearm, it was informed that the hand would be attached to the abdomen for a period of 3 weeks following the surgical procedure and that they would be requiring another procedure for detachment of the flap after 3 weeks following a prior dermotomy.
Twelve patients were males and 3 patients were females. The average age was 35 years with a range of 18–56 years. Regarding the distribution of the defects, 9 patients presented with a defect in the hand/forearm, 2 patients had a defect in the scrotum, 2 patients had a defect in the penis, 1 patient had a defect in the inguinal region overlying the femoral vessels post electric burn injury and 1 patient had a defect in the lower abdomen after excision of the tumor (Tab. 1)
Surgical technique
All patients were operated under spinal anesthesia supplemented with a brachial block wherever needed (in cases involving upper limb reconstructions). Owing to resource constraints, only a handheld doppler was used in assessing the course of the superficial branch of the SCIA in all cases and colour doppler imaging or CT angiography were not performed. The course of the superficial branch was outlined by joining the inguinal crease with the anterior superior iliac spine (ASIS) and the doppler study was then performed. The design of the flap was contemplated as per the perforators evident in the doppler study and the course of the superficial branch. As per previous studies, the major perforator is usually located medial to the anterior superior iliac spine at a distance of around 3 cm in the course of the superficial branch and should be included in the flap [6]. The required dimensions of the flap were marked and a pinch test performed to ensure that the defect could be closed primarily with the hip in extended position. In many cases, the flap was marked beyond the ASIS. Extension beyond the costal margin was not done in any case.
In some cases, a small incision was made in the area overlying the superficial branch near the femoral artery to confirm the presence of the superficial branch. The vessels could be seen below the deep fascia. Once the vessels were seen, dissection proceeded as in other cases. In other cases, the flap incision was made in the superior part and dissection continued until one reached the plane between the superficial and deep layers of fat [9]. The incision was then continued medially until one saw the superficial branch with its attendant perforators. If the superficial branch could not be seen then the lateral incision was made deeper including the deep layer of fat and above the abdominal muscles to include the perforators emanating from the deep branch within the flap. The incision was then carried lower down to trace the transverse branch, which is a division of the deep branch and also acts as a guide for locating the deep branch [11]. The dissection of the deep branch was tedious and was carried out after ligating the branches supplying the lateral femoral cutaneous nerve as well as the sartorius. Depending on the requirement, pedicle dissection towards the source vessel was continued till the flap reached the target area and could be apposed without any tension. When the flap was islanded entirely on its pedicle, a cuff of soft tissue was kept along with the vessels to avoid undue traction and kinking of the vessels. Following this, in some cases, where requirement of an extremely thin flap was desired as in coverage of hand defects, the flap was thinned by taking off extra fat using scissors while staying away from the perforator and the superficial branch of the SCIA. The surrounding areas were then mobilized after the inset of the flap and the wound closed in 2 layers. Stitches were removed usually 10–12 days after surgery.
Drains were usually not required as the deep space was obliterated using plicating sutures taking the deep layer to omit the space. During or after the surgery, flexion of the hip was not required in a single patient even in those where large flaps were harvested although the patients were asked to restrict activities for a week after surgery.
Results
Scrotal reconstruction
In total, 2 cases of scrotal reconstruction were done using the pedicled SCIP flap. In the first patient, who was a case of Fournier’s gangrene, an 18 × 10 cm flap was elevated and inset into the defect following further debridement. However, the distal 3 cm of the flap underwent necrosis. This was managed with debridement followed by primary closure after further mobilization of the remaining scrotal skin. In the second case which resulted from traumatic avulsion of the scrotum and penile skin, a 20 × 10 cm flap was elevated and perforators from both the superficial and deep branches were kept in the flap along with dissection of both branches. The flap settled without any complications. The penile skin was restored using a split thickness skin graft (Fig. 1)

Penile reconstruction
Two cases of coverage of the ventral surface of the penis were done using the pedicled SCIP flap. One patient was a case of severe chordee without hypospadias which needed extensive release of the chordee and division of the urethral plate. The resection of the chordee reached till the tunica albuginea and following resection, a deep excavated wound was noted in the ventral aspect of the penis. To achieve proper contour, a pedicled SCIP flap was then raised and used to fill in the defect. The other was a case of hypospadias cripple with scarred ventral surface which needed resurfacing. This patient had a loss of buccal mucosal graft applied to the ventral surface of the penis and was then subjected to pedicled SCIP flap reconstruction. However, this patient had a total loss of flap from vascular compression and had to be resurfaced again with a buccal mucosal graft. On the other hand, the first patient had very good take of the flap and the flap was detached after 3 weeks. Both patients are currently in the process of undergoing urethroplasty (Fig. 2)

Femoral vessels coverage
In 1 patient with a contact electric burn injury who had an eschar overlying the femoral vessels and also in the lateral part of the groin, the patient was subjected to initial debridement. It was observed that the femoral vessels were exposed following debridement of the eschar and coverage of the defect was accomplished using a 7 × 6 cm pedicled SCIP flap to prevent blow out, which settled nicely. The lateral wound was covered with a split thickness skin graft after debridement (Fig. 3).

Lower abdominal coverage
In 1 patient who had recurrent dermatofibrosarcoma protuberans of the lower abdomen, the resection resulted in a large defect. A frozen section was obtained from the wound margins and the coverage attempted only after getting a negative report. Part of the anterior rectus sheath had to be removed. A pedicled SCIP flap was outlined having a size of 21 × 12 cm. The flap was raised and inset into the defect and there were no complications (Fig. 4).

Coverage of hand defects
In 9 patients with electric burn injury to the hands (5 cases) and traumatic defects of the hand (4 cases) whose general condition was poor with multiple comorbidities and which precluded performance of a microvascular surgery, we used the pedicled SCIP flap to cover the defects based on the superficial branch. The flaps were raised in the plane between the superficial and deep layers of fat and were then used to cover the defects after adequate debridement. All the flaps settled nicely without any necrosis and were detached after 3 weeks (Fig. 5).

In one case a bilobed design was made by splitting the flap in the midline. This was done to accomplish coverage of the thumb and index fingers of the dominant hand in a case of electric burn injury. Again, the handheld doppler was important in ensuring that the flap was centered over the superficial branch of the SCIA (Fig. 6).

In total, 15 flaps were raised with 13 flaps being based on perforators from the superficial branch of the SCIA only while in the rest 2 both the perforators from the superficial and deep branches were taken in the flap. The operative time ranged from 20 to 90 min. The area of the flaps raised varied from 21 to 252 cm2 (the size varied from 7 × 3 cm to 21 × 12 cm, the largest ones required for lower abdominal and scrotal reconstructions). The flap thickness varied from 4 to 10 mm.
Complications
There was a partial loss of one flap and a complete loss of one flap from pedicle compression. The donor site healed well in all cases with no evidence of wound disruption or seroma or hematoma formation. Stiffness was minimal in reconstructed hand cases as both active and passive movements of fingers were encouraged in the postoperative period even with the flap in place. As all the flaps were quite thin, no debulking was needed as an additional procedure.
Discussion
Groin flaps have been used as pedicled and free flaps by plastic surgeons for time immemorial. The pedicled groin flap is still in use in many centers where, because of a very high patient load, it is not possible to subject every patient to a free flap or where facilities for performing a free flap might not be available. It is also used as a lifeboat in some cases of free flap failure. The free groin flap, even though being the first successful free flap, has fallen into disrepute because of the bulky nature of the flap, the variability and short length of the pedicle and associated donor site complications.
Detailed cadaver dissection has shown that the SCIA divides into a superficial and a deep branch after emanating from the femoral artery which then give rise to perforators to supply the area of the groin flap. Based on this anatomy, it has been shown that the flap can be elevated on the perforators originating from the superficial branch only in cases where it is present thereby excluding the deep fat during harvest [12]. The superficial branch can usually be found in most patients 18 mm medial and 17 mm distal to the ASIS when a 21 mm radius circumference is drawn from that point. This marks the exit of the vessel from the Hesselbach’s fascia [13]. In some cases, where the superficial branch is absent, the perforators emanating from the deep branch have to be taken and a deep branch dissection then becomes imperative which is a tedious one. The deep branch-based flap is considerably larger than the superficial based one and has a longer pedicle, thereby increasing the reach of the flap [14].
The pedicled groin flap is extremely bulky and, in many cases, requires debulking as a secondary procedure. Apart from that, the mobility as well as the territory of the pedicled groin flap is limited where it is used as the dissection stops at the medial border of the sartorius muscle. On the other hand, conversion to a SCIP flap has many advantages.
First of all, most SCIP flaps can be raised on a dominant perforator emanating from the superficial branch of the SCIA, therefore a tedious dissection of the deep branch till the origin from the femoral artery is not needed in most cases as in a free groin flap (deep branch dissection may be needed if the superficial branch is atrophic or has an anchoring pattern where it ends abruptly). Secondly, flap elevation time is extremely short when the dissection is done between the superficial and deep layers of fat and visualization of the dominant perforator with the superficial branch is accomplished. Thirdly, in reconstructions where a thin flap is needed, primary defatting can be done with care taken not to injure the perforator or the superficial or deep branch as the case might be. The SCIP flap is extremely thin and pliable. This eliminates the need for further defatting which is imperative when a groin flap is used as the reconstructive modality. Fourthly, large flaps can be raised based on the perforator itself and still the defect can be closed primarily with the scar of the donor area falling in a concealed area.
The pedicled SCIP flap is an extremely versatile flap and can be used for coverage of a wide range of defects. It is particularly suited for scrotal reconstruction as a very thin flap can be raised which can mimic the characteristics of the scrotal skin. Authors have accomplished scrotal reconstruction using flaps from one or both sides [15] but in our patients we found it sufficient to accomplish testicular coverage and create an entire neoscrotum using a single flap only. This flap can also be used in penile reconstructions as well as for reconstructions of the lower abdomen and coverage of the femoral vessels. For hand as well as forearm defects, the advantage is that coverage with a thin flap can be accomplished which therefore does not require later defatting. We have also used a bilobed SCIP flap for coverage of the thumb and index fingers without any complications. This is of use in patients with a poor general condition where a rapid flap elevation and inset can be accomplished and the patients do not have to bear the brunt of a long anesthesia as in a microsurgical procedure. This pedicled flap can also be used as a lifeboat in cases of free flap failure. As the arc of rotation of the pedicled SCIP flap can go up to 180°, this flap is amenable for coverage of a wide range of defects as in our study. However, the anatomy of the perforators and the superficial and deep branches need to be outlined well in the preoperative period. A handheld doppler to mark out the perforators and outline the course of the superficial branch is useful but still has its limitations [16]. Therefore, use of colour doppler and CT angiography can be useful to outline this anatomy [17]. A relatively safe way of harvesting the pedicled flap and to ensure its thinness is to raise it in the level of the superficial fascia in the lateral 1/3 and then go deep down to incorporate the deep branch in case the superficial branch is found to be absent [18]. Other authors have moved on to harvesting a super thin flap of 1.5–4 mm with primary defatting [19].
There are a couple of disadvantages of the pedicled SCIP flap especially when it is used for reconstruction of the upper limb. The hand has to be attached to the abdomen for a period of 3 weeks after the procedure which can be quite cumbersome and uncomfortable to the patient. It can also result in joint stiffness as early physiotherapy cannot be instituted following the procedure. If the patients are not cooperative and are unable to follow instructions, flap avulsion with a need for further suturing and a resultant further period of immobilization might be needed. This flap is also usually not done in children where a free SCIP flap is a better option when coverage of hand defects is needed. Especially in cases where a large flap might be harvested, it might be difficult to close the donor site primarily or might require the thigh to be kept flexed for a period of time. In these cases, another propeller flap based on a perforator from the lateral branch can be used to close the donor site [20].
Conclusion
To conclude, the SCIP flap has been used as a free flap for a wide variety of reconstructions from head to toe but it is also useful as a pedicled flap for a wide range of defects. Large flaps can be raised with primary closure of the donor site with the scar appearing in a concealed site. The dependability of the pedicled SCIP flap implies that this flap should be used more often in reconstructions in and around the genital area. In centers where a large number of pedicled groin flaps are being done, the same might be effectively replaced with the pedicled SCIP flap with its attendant advantages. The procedure is quick when the vessel anatomy has been outlined preoperatively making it especially of use in frail and debilitated patients who would be unable to tolerate the long hours of a microvascular surgery. This can also be used as a lifeboat in free flap failure cases.
Conflicts of interest: The author describes no conflict of interest.
Financial support: The author declares that there was no financial support or non-financial support obtained during the preparation of this article.
Declaration: All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Roles of authors: The first author has been actively involved in the planning, preparation, analysis and interpretation of the findings and processing of the article. The second author has assisted the first author in the cases and in revising the manuscript.
Dr. Souvik Adhikari, MBBS, MS, MCh
Associate Professor of Plastic Surgery
Institute of Post Graduate Medical
Education & Research
244, A. J. C. Bose Road
Kolkata – 700020
West Bengal, India
e-mail: souvikadhikari@yahoo.com
Submitted: 24. 8. 2022
Accepted: 15. 1. 2023
Sources
1. Daniel RK., Taylor GI. Distant transfer of an island flap by microvascular anastomoses. A clinical technique. Plast Reconstr Surg. 1973, 52(2): 111–117.
2. Cooper TM., Lewis N., Baldwin MA. Free groin flap revisited. Plast Reconstr Surg. 1999, 103(3): 918–924.
3. Chuang DC., Colony LH., Chen HC., et al. Groin flap design and versatility. Plast Reconstr Surg. 1989, 84(1): 100–107.
4. Hahn SB., Kim HK. Free groin flaps in microsurgical reconstruction of the extremity. J Reconstr Microsurg. 1991, 7(3): 187–195.
5. Koshima I., Soeda S. Inferior epigastric skin flap without rectus abdominis muscle. Br J Plast Surg. 1989, 42(6): 645–648.
6. Koshima I., Nanba Y., Tsutsui T., et al. Superficial circumflex iliac artery perforator flap for reconstruction of limb defects. Plast Reconstr Surg. 2004, 113(1): 233–240.
7. Tashiro K., Harima M., Kato M., et al. Preoperative color Doppler ultrasound assessment in planning of SCIP flaps. J Plast Reconstr Aesthet Surg. 2015, 68(7): 979–983.
8. Scaglioni MF., Meroni M., Fritsche E., et al. Combined pedicled superficial circumflex iliac artery perforator (SCIP) flap with lymphatic tissue preservation and lymphovenous anastomosis (LVA) for defect reconstruction and lymphedema-lymphocele prevention in thigh sarcoma surgery: preliminary results. J Surg Oncol. 2021, 123(1): 96–103.
9. Yoo KW., Shin HW., Lee HK. A case of urethral reconstruction using a superficial circumflex iliac artery. Arch Plast Surg. 2012, 39(3): 253–256.
10. Hong JP., Sun SH., Ben-Nakhi M. Modified superficial circumflex iliac artery perforator flap and supermicrosurgery technique for lower extremity reconstruction: a new approach for moderate-sized defects. Ann Plast Surg. 2013, 71(4): 380–383.
11. Yoshimatsu H., Yamamoto T., Hayashi A., et al. Use of the transverse branch of the superficial circumflex iliac artery as a landmark facilitating identification and dissection of the deep branch of the superficial circumflex iliac artery for free flap pedicle: anatomical study and clinical applications. Microsurgery. 2019, 39(8): 721–729.
12. Fuse Y., Yoshimatsu H., Karakawa R., et al. Deep fat saving elevation of the superficial circumflex iliac artery perforator flap. Medicina (Kaunas). 2022, 58(5): 670.
13. Fernandez-Garrido M., Nunez-Villaveiran T., Zamora P., et al. The extended SCIP flap: an anatomical and clinical study of a new SCIP flap design. J Plast Reconstr Aesthet Surg. 2022, 75(9): 3217–3225.
14. Zubler C., Haberthür D., Hlushchuk R., et al. The anatomical reliability of the superficial circumflex iliac artery perforator (SCIP) flap. Ann Anat. 2021, 234 : 151624.
15. Scaglioni MF., Meroni M., Fritsche E. Pedicled superficial circumflex iliac artery perforator flap for male genital reconstruction: a case series. Microsurgery. 2022, 42(8): 775–782.
16. Schiltz D., Lenhard J., Klein S., et al. Do-it-yourself preoperative high-resolution ultrasound-guided flap design of the superficial circumflex iliac artery perforator flap (SCIP). J Clin Med. 2021, 10(11): 2427.
17. Pereira N., Parada L., Kufeke M., et al. A new planning method to easily harvest the superficial circumflex iliac artery perforator flap. J Reconstr Microsurg. 2020, 36(3): 165–170.
18. Boissière F., Luca-Pozner V., Vaysse C., et al. The SCIP propeller flap: versatility for reconstruction of locoregional defect. J Plast Reconstr Aesthet Surg. 2019, 72(7): 1121–1128.
19. Lee KT., Park BY., Kim EJ., et al. Superthin SCIP flap for reconstruction of subungual melanoma: aesthetic functional surgery. Plast Reconstr Surg. 2017, 140(6): 1278–1289.
20. Zhang YX., Hallock GG., Song D., et al. Synchronous closure of a large medial perforator-based superficial circumflex iliac artery perforator free flap donor site using an ipsilateral lateral perforator-based superficial circumflex iliac artery perforator propeller flap. Ann Plast Surg. 2020, 85(2): 146–148.
Labels
Plastic surgery Orthopaedics Burns medicine TraumatologyArticle was published in
Acta chirurgiae plasticae

2022 Issue 3-4
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Safety and Tolerance of Metamizole in Postoperative Analgesia in Children
-
All articles in this issue
- Editorial
- Evaluation of resection margins in oral squamous cell carcinoma
- 3D color doppler ultrasound for postoperative monitoring of vascularized lymph node flaps
- Preservation of supraclavicular nerve while harvesting supraclavicular lymph node flap
- Determination of the adequate vascular perfusion time of cross-leg free latissimus dorsi myocutaneous flaps in reconstruction of complex lower extremity defects
- Wichterle hydron for breast augmentation – case reports and brief review
- The ideal timing for revision surgery following an infected cranioplasty
- Adult orbital xanthogranuloma – a case report
- Mini-invasive technique of sclerotherapy with talc in chronic seroma after abdominoplasty – a case report and literature review
- Multifarious uses of the pedicled SCIP flap – a case series
- In memoriam
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Mini-invasive technique of sclerotherapy with talc in chronic seroma after abdominoplasty – a case report and literature review
- Multifarious uses of the pedicled SCIP flap – a case series
- 3D color doppler ultrasound for postoperative monitoring of vascularized lymph node flaps
- Evaluation of resection margins in oral squamous cell carcinoma