Invasive primary intracerebral infections in women caused by Streptococcus intermedius manifesting as purulent meningitis and intracerebral abscess
Invazivní primarně intracerebrální infekce u žen způsobené Streptococcus intermedius a manifestující se jako purulentní meningitida a intracerebrální absces
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors:
P. Prášil 1; V. Boštíková 2
; Z. Hermannová 1; S. Plíšek 1; P. Boštík 1,2
Authors‘ workplace:
Department of Infectious Diseases, Charles University, Faculty of Medicine and University Hospital, Hradec Králové, Czech Republic
1; Faculty of Military Health Sciences, University of Defence, Hradec Králové, Czech Republic
2
Published in:
Cesk Slov Neurol N 2018; 81(2): 220-222
Category:
Letter to Editor
doi:
https://doi.org/10.14735/amcsnn2018220
Overview
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Dear Editor,
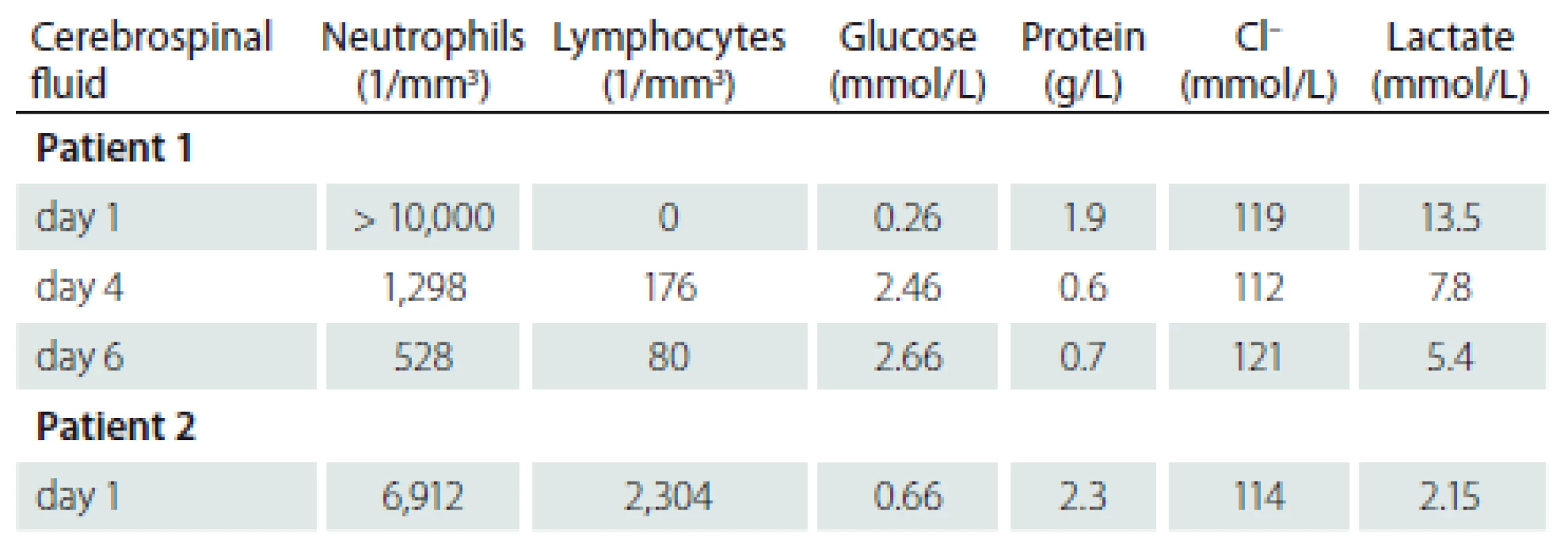
Brain abscess is characterised as a purulent infection of the brain with cerebritis leading to central necrosis that can be caused by a broad spectrum of infectious agents. Here we report two cases of invasive infections of Streptococcus intermedius in women with no identified primary focus other than the intracerebral manifestation.
Patient 1 is a 55-years-old woman treated chronically for depression. She was admitted to the local department of neurology for fatigue and sleeplessness and showed slowed psychomotor reactions, dysarthria, lesion the of the right VIIth nerve and positive meningeal signs. Blood tests showed an elevation of C-reactive protein (CRP) (141 mmol/ L) and leucocytosis (14.9 × 109/ L). A native CT scan showed vasogenic edema in the left frontal lobe (50 × 40 × 55 mm) with a centrally localized focus (21 × 20 × 20 mm). IV anti-edematic therapy was started together with IV amoxycilin/ clavulanate. The next day, a contrast enhanced CT scan identified a circular tumor-like focus in the left frontal lobe with surrounding edema. The suspected diagnosis of glioblastoma was made and the patient was transferred to the Department of Neurology of the University Hospital. There, the cerebrospinal fluid (CSF) was examined with results supporting a diagnosis of a brain abscess (Tab. 1). The anti-edematic therapy was continued, but the antibiotic therapy was changed to a combination of ceftriaxon + metronidazol + vancomycin.After a non-invasive approach was indicated, the patient was transferred to the Department of Infectious Diseases (DID). Symptomatically she was afebrile, somnolent, able to follow only simple command, with positive meningeal signs, lesion of the right VIIth nerve and Glasgow Coma Scale (GCS) of 12. CSF showed high inflammatory markers, but the cultivation was negative. CT scan of the brain on day 4 at the DID showed an abscess in the left frontal lobe with communication to the ventricles, vetriculitis and surrounding edema. The panbacterial DNA test identified Streptococcus intermedius, which was confirmed later on by anaerobic CSF cultivation. The cultivation from all other biological samples was negative and additional examinations identified no other potential focus of the infection. After 4 days of therapy, the status of the patient improved. Despite some dysarthria, the patient started to communicate, neurological symptoms and the inflammatory markers improved and the CSF laboratory markers also showed improvement (Tab. 1).
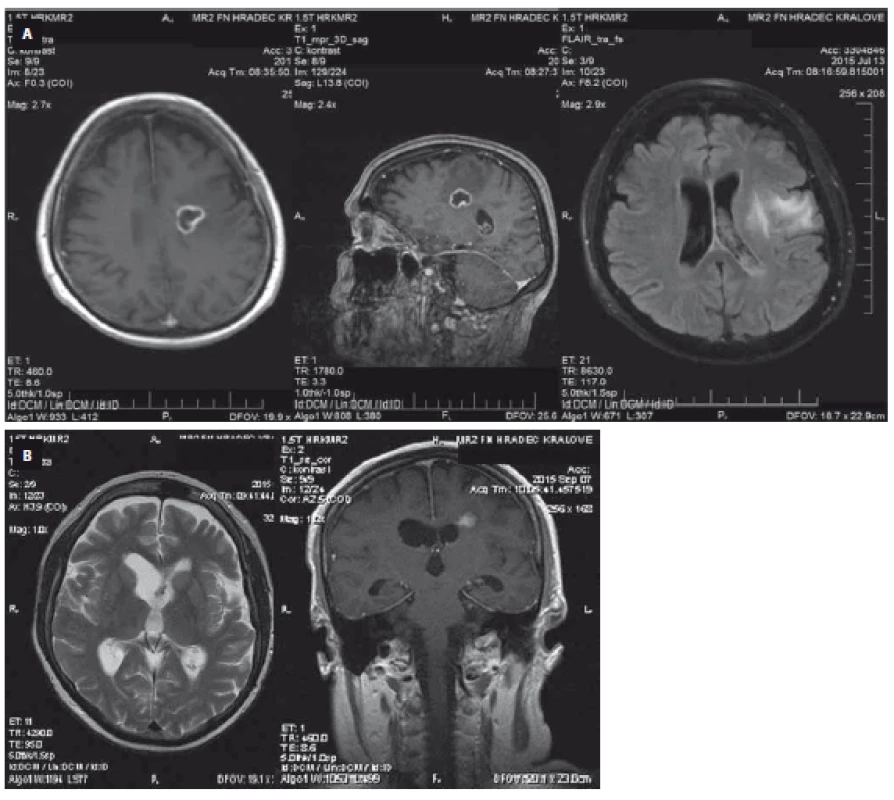
On day 6 at DID, the patient continued to improve. She suffered only from minor dysarthria, inflammatory markers returned to normal (leucocytes 7.7 × 109/ L, CRP 5.5 mmol/ L) and CSF laboratory results further improved (Tab. 1). On day 10, the MRI showed the brain abscess and ventriculitis. In addition, however, a pathological content of the lateral ventricle appeared as small abscesses (Fig. 1A). Based on these findings, a drainage of the abscess was initiated with confirmatory bacteriological findings from the abscess material. At this point, the sensitivity of the identified agent was established as having minimal inhibitory concentrations (MIC) for penicillin (MIC = 0.008 mg/ L). Therefore, the antibiotic combination was terminated and a high dose of crystalline penicillin was administered instead (48 MIU/ day). The ventricular drainage continued for 4 days and then was terminated. The MRI performed on day 32 showed further regression of brain edema, a decrease of abscess size and no CSF circulation pathology. Antibiotic therapy was terminated on day 62, when the MRI showed a disappearance of the liquid in the site of the former abscess and signs of scarring in the surrounding tissue (Fig. 1B). The patient finally recovered with no residual finding.
Patient 2 is a 43-year-old woman. Her first symptoms started 3 days before as fever and headaches leading to meningeal signs. Her DID entry exam showed fever, hypohydration, positivity of upper meningeal signs, but she was fully conscious and neurogically showing only transient problems with dystaxia of her left upper limb. The blood laboratory tests showed high CRP (272.7 mmol/ L) and fibrinogen (6.1 mmol/ L) values as well as leucocytosis (16.33 × 109/ L). CSF examination supported a diagnosis of bacterial meningitis (Tab. 1), but microscopy and agglutination tests were negative. MRI showed no focal infection of the brain. PCR for the panel of bacteria was negative. The patient was rehydrated, therapy with ceftriaxon (4 g/ day) was started and, after negative results for Listeria spp, ampicilin and corticosteroids were added. Simultaneously, a thorough exam failed to identify a potential focus of the infection. On day 3 after admission, Streptococcus intermedius was identified by both cultivation and sequencing from CSF with a good sensitivity to penicillin (MIC = 0.018 mg/ L). Antibiotic therapy was thus adjusted to a high dose of crystalline penicillin potassium salt (48 MIU/ day), which led to the normalization of the levels of inflammatory markers. The complete normalization of the CSF was, however, achieved after 18 days post-admission. The patient was released 21 days after the beginning of hospitalization showing no residual symptoms.
Both cases showed invasive infections caused by Streptococcus intermedius, which are relatively rare, but pose a relatively high pathogenic potential. Previous studies showed patients with diseases caused by this bacteria indicating a propensity of this bacteria to the formation of abscesses [1 – 4]. Our case report 2, however, showed a patient with an invasive infection without abscess formation, which is very rare. In both presented cases, no primary focus was found elsewhere, despite of the extensive searching [5]. This suggests a hematogenous spread of Streptococcus intermedius. The diagnosis of Streptococcus intermedius is critical since the growth conditions are anaerobic. When examining CSF, tests may not always include bacteria from this group. For the molecular analysis, the next step then is a panbacterial DNA test with subsequent sequencing (16s rRNA) [1,2,6,7].
Antibiotic therapy before the identification of the pathogen needs to cover a broader spectrum and is achieved by a combination therapy, which includes third generation cephalosporins with metronidazol and, potentially, vancomycin [8]. A targeted therapy shall then be introduced after the causative agent has been identified and sensitivity has been tested. Penicillin is the antibiotic of choice in infections caused by Streptococcus intermedius [6 – 9]. In the case of Streptococcus intermedius resistance to penicillin, cefotaxim, teicoplanin or vancomycin are available [9,10].
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 6. 9. 2017
Accepted for print: 1. 3. 2018
prof. MUDr. Pavel Boštík, Ph.D.
Department of Infectious Diseases
Charles University Faculty of Medicine and University Hospital
Šimkova 870
500 03 Hradec Králové, Czech Republic
e-mail: bostikp@lfhk.cuni.cz
Sources
1. Noguchi S, Yatera K, Kawanami T et al. The clinical features of respiratory infections caused by the Streptococcus anginosus group. BMC Pulm Med 2015; 15 : 133. doi: 10.1186/ s12890-015-0128-6.
2. Tran MP, Caldwell-McMillan M, Khalife W et al. Streptococcus intermedius causing infective endocarditis and abscesses: a report of three cases and review of the literature. BMC Infect Dis 2008; 8 : 154. doi: 10.1186/ 1471-2334-8-154.
3. Jouhadi Z, Sadiki H, Hafid I et al. [Streptococcus intermedius: a rare cause of brain abscess in children]. Arch Pediatr 2013; 20(3): 282 – 285. doi: 10.1016/ j.arcped.2013.01.002.
4. Saijo M, Murono K, Hirano Y et al. [A patient with Streptococcus intermedius brain abscess treated with high dose penicillin G--susceptibility of the isolate to penicillin G and the concentration of penicillin G in cerebrospinal fluid]. Kansenshogaku Zasshi 1998; 72(4): 414 – 417.
5. Moazzam AA, Rajagopal SM, Sedghizadeh PP et al. Intracranial bacterial infections of oral origin. J Clin Neurosci 2015; 22(5): 800 – 806. doi: 10.1016/ j.jocn.2014.11.015.
6. Ohara N, Asai K, Ohkusu K et al. [A case of culture-negative brain abscess caused by Streptococcus intermedius infection diagnosed by broad-range PCR of 16S ribosomal RNA]. Brain Nerve 2013; 65(10): 1199 – 1203.
7. Saito N, Hida A, Koide Y et al. Culture-negative brain abscess with Streptococcus intermedius infection with diagnosis established by direct nucleotide sequence analysis of the 16s ribosomal RNA gene. Internal med 2012; 51(2): 211 – 216.
8. Gilbert DN, Moellering RC, Eliopoulos GM et al. Brain abscess. In: The Sanford guide to antimicrobial therapy. 41st ed. Sanford: Antimicrobial Therapy, Inc. 2011.
9. Rozkiewicz D, Daniluk T, Sciepuk M et al. Prevalence rate and antibiotic susceptibility of oral viridans group streptococci (VGS) in healthy children population. Adv Med Sci 2006; 51 (Suppl 1): 191 – 195.
10. Jacobs JA, Stobberingh EE. In-vitro antimicrobial susceptibility of the „Streptococcus milleri‘ group (Streptococcus anginosus, Streptococcus constellatus and Streptococcus intermedius). J Antimicrob Chemother 1996; 37(2): 371 – 375.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2018 Issue 2
- Memantine Eases Daily Life for Patients and Caregivers
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
- Advances in the Treatment of Myasthenia Gravis on the Horizon
-
All articles in this issue
- Glucose transporter-1 deficiency syndrome – expanding the clinical spectrum of a treatable disorder
- Carpal tunnel syndrome within the context of functional disorders of the musculoskeletal system
- Identification of pediatric patients with pharmacoresistant epilepsy and selection of candidates of non-pharmacological therapy
- Neurofilament light chains in serum and cerebrospinal fluid and status of blood-CSF barrier in the selected neurological diseases
- Physiotherapy in Parkinson’s disease in the Czech Republic – a demographic study
- Patients with idiopathic REM sleep behavior disorder follow-up – phenoconversion into parkinsonian syndrome and dementia
- Czech version of the Edinburgh Cognitive and Behavioral Amyotrophic Lateral Sclerosis Screen – a pilot study
- Acute pediatric myelitis – cohort of 20 patients
- Granular cell tumor in the pituitary stalk
- Brain biopsy in 10 key points – what can a neurologist expect from the neurosurgeon and the neuropathologist?
- Ataxia
- Anticoagulation therapy in patients with atrial fibrillation and cerebral amyloid angiopathy - NO
- Anticoagulation therapy in patients with atrial fibrillation and cerebral amyloid angiopathy
- Anticoagulation therapy in patients with atrial fibrillation and cerebral amyloid angiopathy - YES
- Fabry disease, an overview and the most common neurological manifestations
- Is the role of amyloid in senile dementia substantial?
- Serum anti-Müllerian hormone levels in multiple sclerosis – a multicenter case-control study
- Invasive primary intracerebral infections in women caused by Streptococcus intermedius manifesting as purulent meningitis and intracerebral abscess
- Malignant melanotic schwannoma of the vertebral body in a patient with Carney complex
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Ataxia
- Brain biopsy in 10 key points – what can a neurologist expect from the neurosurgeon and the neuropathologist?
- Fabry disease, an overview and the most common neurological manifestations
- Glucose transporter-1 deficiency syndrome – expanding the clinical spectrum of a treatable disorder
