Factors influencing recurrence of the pressureulcers after plastic surgery – retrospective analysis
Faktory ovlivňující recidivu dekubitální léze po plastickém chirurgickém výkonu – retrospektivní analýza
Cíl:
Cílem studie bylo zhodnotit proces péče u pacientů s dekubitem, kteří byli indikováni k plastické operační intervenci a faktorů ovlivňujících recidivu dekubitu.
Metodika:
Retrospektivní analýza uzavřené dokumentace pacientů indikovaných k plastické operaci realizované na klinice plastické chirurgie.
Výsledky:
Statisticky významnými faktory, které souvisely s výskytem recidivy dekubity, byly index tělesné hmotnosti (body mass index; BMI) a tělesná lokalizace dekubitů u sledované populace 46 pacientů s 55 dekubity.
Závěr:
Ve sledované populaci byly BMI a tělesná lokalizace dekubitu identifikovány jako statisticky významné faktory související s recidivou dekubitů. Vyšší BMI bylo spojeno s častějším výskytem recidivy. Dekubitus v ischiadické oblasti byl spojen s častější recidivou, bez ohledu na průměrnou velikost dekubitu.
Klíčová slova:
dekubitální léze – dekubitus – terapie – hospitalizace – chirurgický rekonstrukční výkon – laloková plastika – retrospektivní analýza
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů
Authors:
N. Antalová 1; A. Pokorná 1; A. Hokynková 2; L. Cetlová 3; Jakub Turek 4
Authors‘ workplace:
Department of Nursing, Faculty of Medicine, Masaryk University, Brno, Czech Republic
1; Department of Burns and Plastic Surgery, University Hospital Brno, Czech Republic
2; Department of Healthcare Studies, College of Polytechnics, Jihlava, Czech Republic
3; Department of Pediatric Surgery, Orthopedics and Traumatology, University Hospital Brno, Czech Republic
4
Published in:
Cesk Slov Neurol N 2018; 81(Suplementum 1): 23-28
Category:
Original Paper
doi:
https://doi.org/10.14735/amcsnn2018S23
Overview
Aim:
The aim of the study was to evaluate the therapy process in patients with pressure ulcers indicated for plastic surgery intervention and to determine the factors influencing recurrence of pressure ulcers.
Methods:
Retrospective analysis of patients’ documentation indicated for plastic surgery performed in a plastic surgery unit.
Results:
Body mass index (BMI) and body site of the pressure ulcers were identified as the significant factors influencing the rate of the recurrence of the lesion in the analyses of 46 patients with 55 pressure ulcers.
Conclusion:
In the monitored patients’ population, BMI and the site of pressure ulcers were identified as statistically significant parameters responsible for the recurrence of the lesions. The higher the BMI, the more frequent recurrence had occurred. The presence of pressure ulcers in the ischiatic area was related to the increased recurrence rate, regardless of the average size of the lesion.
Introduction
Pressure ulcers (PUs) and their occurrence, especially in patients with neurological disease and with permanently limited mobility (para - or tetraplegic), are challenging issues for health care systems. The lesions occur more frequently in patients with spinal cord injury [1]. These patients suffer from the PUs predominantly localized at the ischiatic, sacral and trochanteric areas which do not allow appropriate conservative treatment typical for the I. and II. category PUs, and therefore patients are indicated for mostly two-stage surgical intervention [2]. With respect to the overall condition of patients, there is a high risk of recurrence of PUs that we tried to identify.
Aim
The aim of this study was to analyse the process of the treatment in patients with PUs indicated for the plastic surgery intervention and to determine the factors influencing recurrence of PUs.
Methods
Data collection was performed by retrospective record analysis of patients hospitalized at the Clinic of Burns and Plastic Surgery of one of the university hospitals in the Czech Republic, in one-year time interval (from January 2016 to January 2017).
Patients enrolled in the study were hospitalized with the main diagnosis of L89 according to the International Classification of Diseases (ICD)-10 and were also indicated for plastic surgical treatment.
The following parameters were observed: patient‘s demographic data (age, gender, and occupation), general patient status (mobility, Norton Scale Pressure Ulcers RiskAssessment), local finding, PUs characteristics (localization, categorization based on EPUAP/NPUAP), type, time and number of surgical interventions and the PUs recurrence. Statistical analysis of the data was performed with the software for analysis and statistics SPSS version 20.0 (IBM Corp., Armonk, NY, USA) using the Kruskal Wallis test and multilinear regression analysis at a significance level of 0.05.
Characteristics of the monitored population
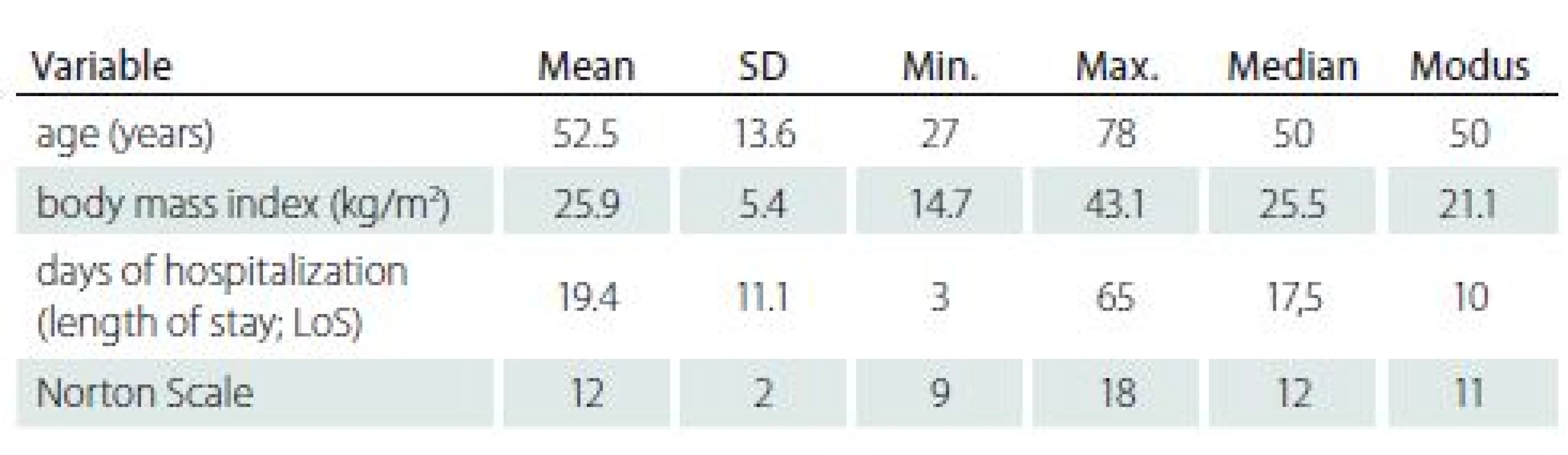
In period of 12 months, 48 patients were surgically treated. The total number of patients enrolled in this analysis was 43. Five patients were admitted to different department so they were excluded due to lack of follow up data. Three patients underwent an independent follow-up on another site that was not considered as a recurrence and therefore the total number of cases under review was 46, i.e. 100% with a total of 55 PUs. For a more detailed description of the examined population, see Tab. 1.
Results and discussion
Of the total number of 46 cases, 41 (89.1%) males and 5 (10.9%) females were included. Using the descriptive statistics, general population characteristics (age, body mass index [BMI], number of days in hospital, Norton Scale) were also evaluated (Tab. 1).
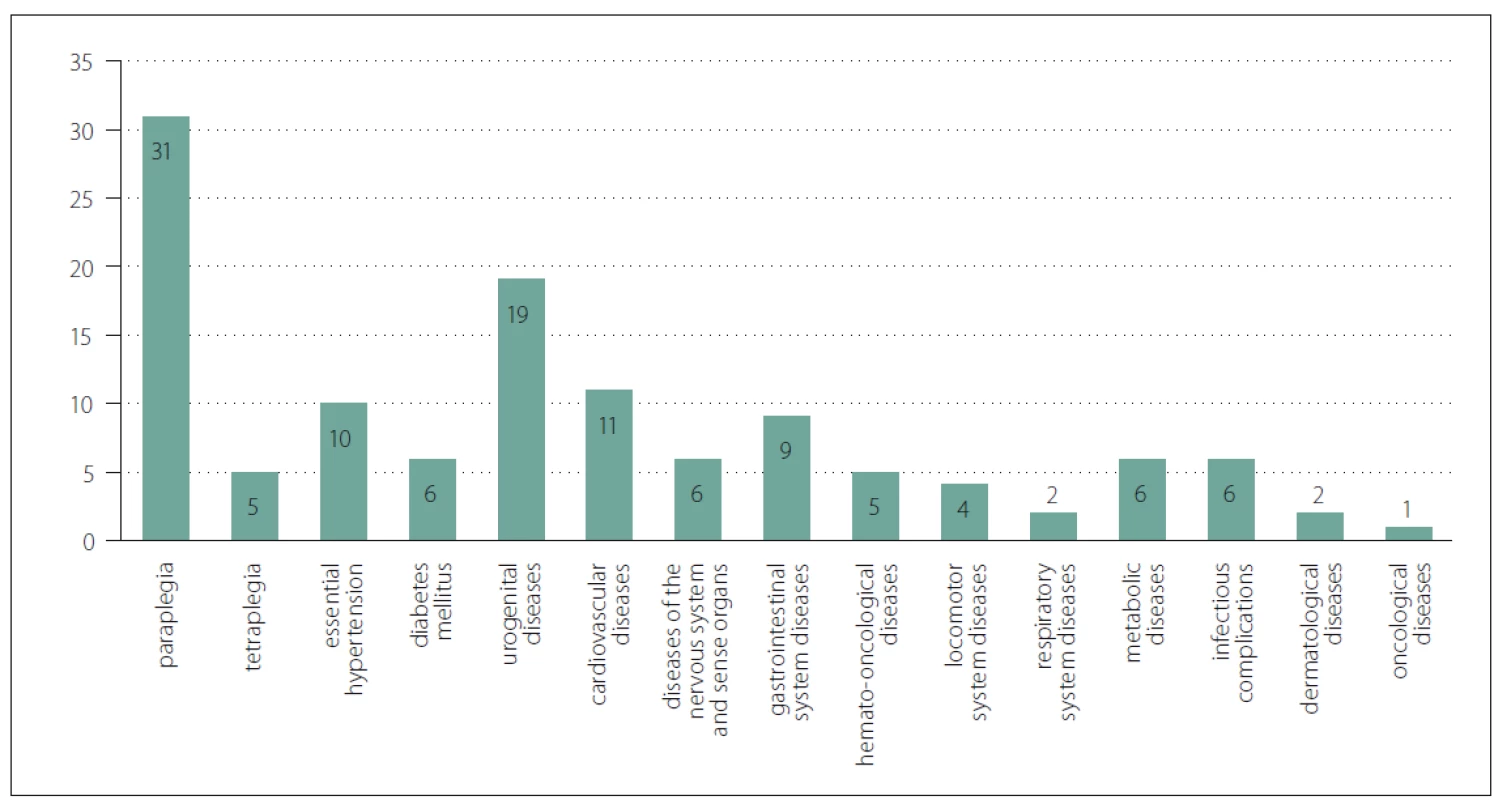
The mean age in our population seems to be not as high as expected; on the other hand, the most common comorbidity of paraplegia (N = 31; 72%) was the most frequent risk factor for the formation of PU, but the aetiology of paraplegia was not documented, or it was impossible to determine the time of its onset. Spinal cord lesions also occur in patients of younger age, most often due to traumatic etiology [3,4].
With a higher age, the risk of PUs as well as the mobility limitation and length of hospitalization are increasing [1]. Most of the patients had significantly limited mobility - wheelchair mobility (23; 50%); total immobility on the bed (6; 13%) and a minimum of patients were able to use crutches or walking sticks (2; 4.4%). In 15 (32.6%) patients, mobility was not recorded nor rated by any scale (e. g. Activity of Daily Living Scale [ADL]). Similarly, the study presented by Hoff et al., shows that patients with reduced activity/ immobility due to spinal cord injury are more at risk with the occurrence of PUs [5].
Another important observed parameter was body weight and nutritional status. In our population, mean BMI was 25.9 kg/ m2 (min. 14.7 kg/ m2; max. 43.1 kg/ m2). Greater weight of the patient is associated with a higher risk of PU lesions and complicates the positioning of the patient by healthcare staff [6]. Equally important is the fact that obesity is directly associated with numerous health problems such as stroke, heart disease or diabetes, and these comorbidities can also indirectly influence the development and course of treatment of PUs [7]. This was also verified in our retrospective study.
The shortest period of hospitalization was 3 days, the longest hospital stay of one patient was 65 days (average hospital stay was 19.4 days). Several authors report that the average time of the hospitalized patients increases the risk of complications, including colonization by hospital-acquired pathogens (hospital acquired infections) [8]. Therefore, in addition to practical and economic considerations, the goal is to reduce the number of days of stay at the hospital to the shortest possible time. An interesting study was presented by Milchelski et al., in which, due to the careful and intensive patients’ preparation at the outpatient clinic, hospitalization alone during reconstructive surgery lasted in average of 3.6 days. During a relatively short postoperative follow-up, only 11.1% of patients experienced a mild wound dehiscence, and no patient underwent reoperation or necrosis of the transmitted lobe [9]. However, this procedure assumes an excellent level of care after the patient had been dismissed from the hospital.
The Norton Scale, used by the clinic‘s nurses to assess the risk of PUs at the reported institution, was at least 9 in the observed patients and the highest value was 18 points (12 points mean).
Comorbidities of patients in our population are involved, in a greater or lesser extent, in the formation and treatment of PUs. In accordance with the international literature, patients with neurological disorders, especially with spinal cord affection, are the most at risk, where according to the literature there may be up to 80% risk of recurrence of PUs [10]. Eslami et al. evaluated that between tetraplegic and paraplegic patients, the prevalence of PUs was 20 – 60%, and about 85% of patients with spinal cord injury may experience PUs during treatment [11]. In our population, as already mentioned, 31 (72%) patients were diagnosed with neurological disease – paraplegia. Other comorbidities are summarized in Fig. 1. In majority of the patients, multiple surgeries were performed (Tab. 2, 3).
Obr. 1. Komorbidity (N = 46 případů).
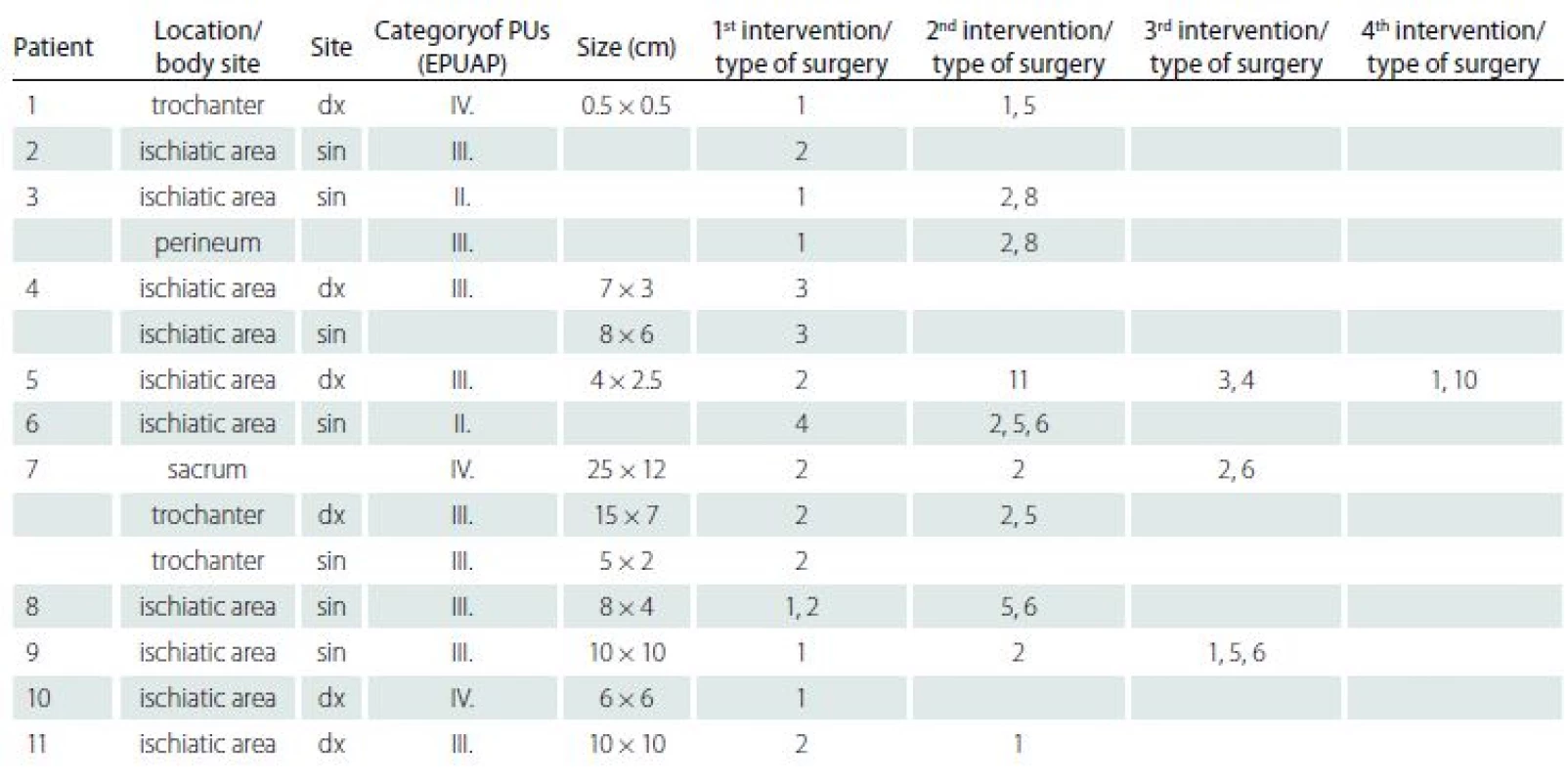

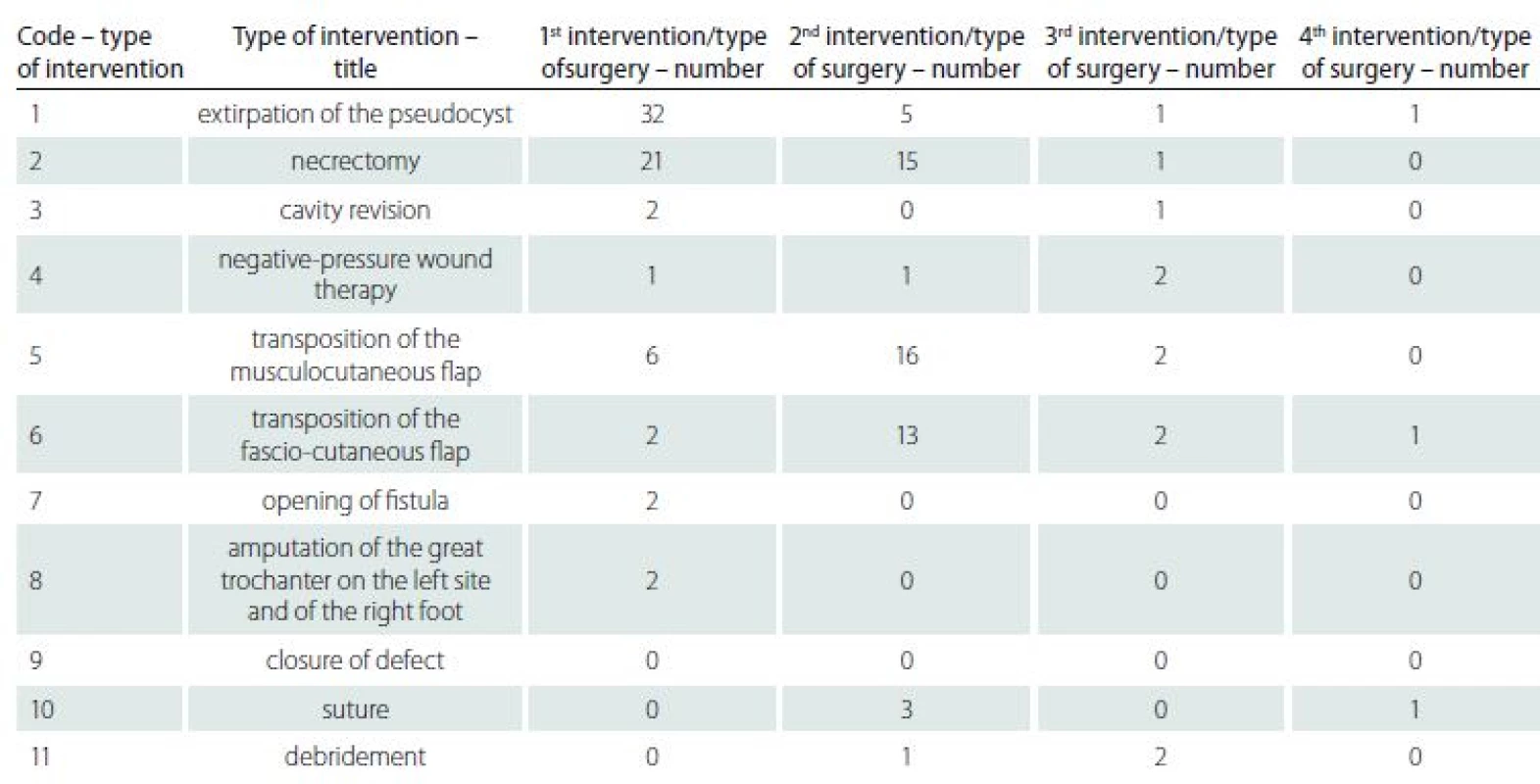
The recurrence of PUs was documented in 28 cases (60,9%). Based on the literature research, following parameters: age, gender, BMI, mobility according to compensatory aid for locomotion and locality of PUs, were identifies as potential factors of recurrence of PUs after plastic surgery intervention. The statistical analysis is summarized in Tab. 4.
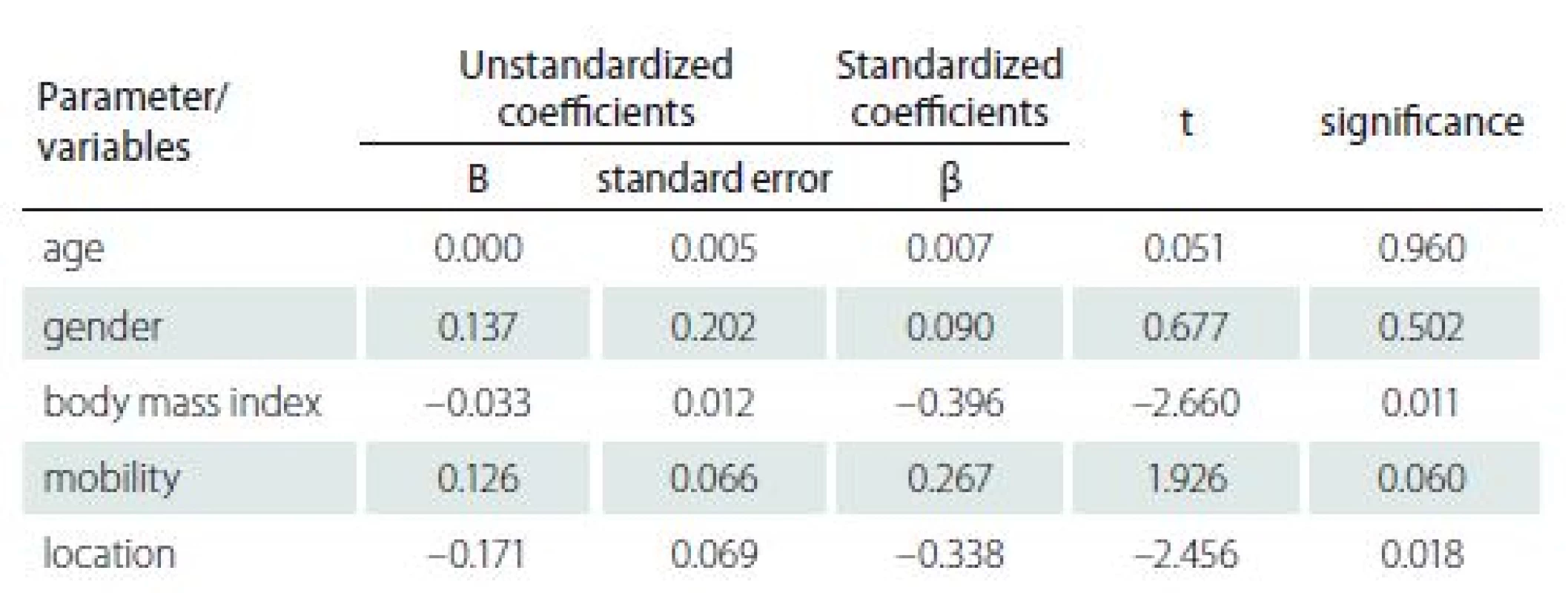
Based on the results, we can state that the age, gender, and patient mobility do not have a significant effect on the prediction of recurrence of PUs (p > 0.05) in monitored population. On the other hand, BMI and localization (body site) of PU had shown to significantly predict the occurrence of recurrence. Thus, we can say that in patients with higher BMI there is a significantly higher risk of recurrence of PUs. The location of the PU is also a significant factor for the formation of PUs and their recurrences. Most of the total number of 55 PUs was documented in the ischiatic area, and the average size of the PUs varied at different locations (see Tab. 5 for details).
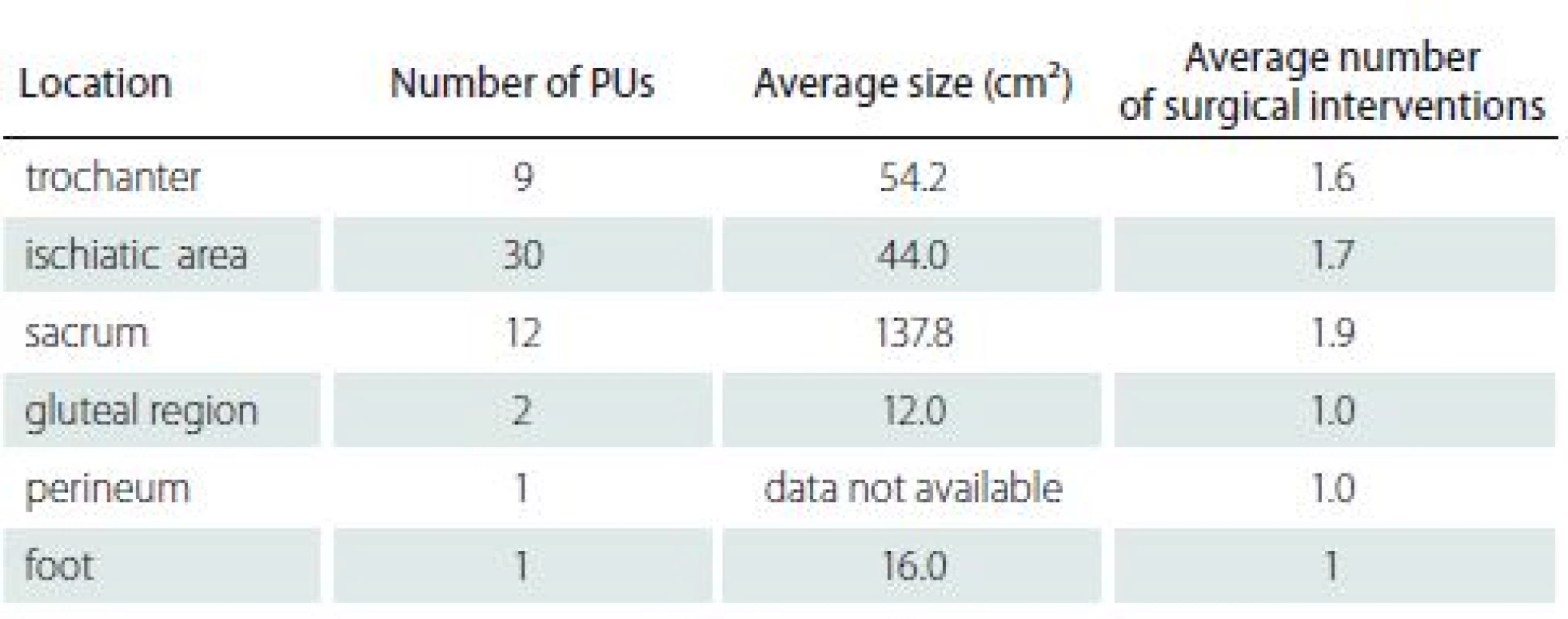
Considering the location/ body site of the PU as a factor of the recurrence, the higher risk is in PU localized at the ischiatic area, in which 45.5% of all PUs had documented the recurrence. This finding is clinically related to the documented size of the decubitus, although this assumption has not been confirmed in our statistical analysis.
Conclusion
Pressure ulcers in patients with neurological diagnosis and diseases and impaired mobility indicated for surgical performance is typical for a relatively high risk of recurrence. From a retrospective analysis of 46 cases of patients with PU lesions, BMI and the localization of the PUs were validated as statistically significant risk factors of PUs recurrence. Higher BMI and the PUs at the ischiatic region were identified with the higher risk of the recurrence of PUs.
Limitations of the study
The main limitation was the retrospective nature of the study. Some of the information reviewed were not available in the medical records at all or in the different parts of documentations. Thus, there have been identified shortcomings in the management of documentations. By elimination of this limitation in the future, it could result in greater clarity and consequently effectiveness in further processing of data that can be used to improve the care of patients with reduced mobility indicated for plastic surgery. The second main limitation is relatively small number of cases enrolled in the study (N = 46), which is affected by the total number of patients with neurological disease indicated for the plastic surgical treatment of PUs at the given unit. Nonetheless, the study‘s advantage is that follow-up of 46 cases was complete and all the patients met the inclusion criteria in the one-year period of data collection.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
doc. PhDr. Andrea Pokorná, Ph.D.
Department of Nursing
Faculty of Medicine
Masaryk University
Kamenice 3, 625 00 Brno
Czech Republic
e-mail: apokorna@med.muni.cz
Accepted for review: 13. 6. 2018
Accepted for print: 10. 8. 2018
Sources
1. Pokorná A, Benešová K, Mužík J et al. Sledování dekubitálních lézí u pacientů s neurologickým onemocněním – analýza Národního registru hospitalizovaných. Cesk Slov Neurol N 2016; 79/ 112 (Suppl 1): S8 – S14. doi: 10.14735/ amcsnn2016S14.
2. Hokynková A, Šín P, Černoch F et al. Využití lalokových plastik v operační léčbě dekubitů. Cesk Slov Neurol N 2017; 80/ 115 (Suppl 1): S41 – S44. doi: 10.14735/ amcsnn2017S41.
3. Vašíčková L, Sieglová J, Mašek M. Význam tlakové mapy (pressure mapping system) pro pacienty s mobilitou na vozíku. Cesk Slov Neurol N 2016; 79/ 112 (Suppl 1): S15 – S19. doi: 10.14735/ amcsnn2016S15.
4. Taghipoor KD, Arejan RH, Rasouli MR et al. Factors associated with pressure ulcers in patients with complete or sensory-only preserved spinal cord injury: is there any difference between traumatic and nontraumatic causes? J Neurosurg Spine 2009; 11(4): 438 – 444. doi: 10.3171/ 2009.5.SPINE08896.
5. Hoff JM, Bjerke LW, Gravem PE et al. Pressure ulcers after spinal cord injury. Tidsskr Nor Laegeforen 2012; 132(7): 838 – 839. doi: 10.4045/ tidsskr.10.0878.
6. Walden CM, Bankard SB, Cayer B et al. Mobilization of the obese patient and prevention of injury. Ann Surg 2013; 258(4): 646 – 650. doi: 10.1097/ SLA.0b013e3182a5039f.
7. Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg 2009; 250(1): 166 – 172. doi: 10.1097/ SLA.0b013e3181ad8935.
8. Glance LG, Stone PW, Mukamel DB et al. Increases in mortality, length of stay, and cost associated with hospital-acquired infections in trauma patients. Arch Surg 2011; 146(7): 794 – 801. doi: 10.1001/ archsurg.2011.41.
9. Milcheski DA, Mendes RRDS, Freitas FR et al. Brief hospitalization protocol for pressure ulcer surgical treatment: outpatient care and one-stage reconstruction. Rev Col Bras Cir 2017; 44(6): 574 – 581. doi: 10.1590/ 0100-69912017006005.
10. Bansal C, Scott R, Stewart D et al. Decubitus ulcers: a review of the literature. Int J Dermatol 2005; 44(10): 805 – 810. doi: 10.1111/ j.1365-4632.2005.02636.x.
11. Eslami V, Saadat S, Habibi Arejan R et al. Factors associated with the development of pressure ulcers after spinal cord injury. Spinal Cord 2012; 50(12): 899 – 903. doi: 10.1038/ sc.2012.75.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2018 Issue Suplementum 1
- Memantine Eases Daily Life for Patients and Caregivers
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
- Advances in the Treatment of Myasthenia Gravis on the Horizon
-
All articles in this issue
- Pressure lesion monitoring – data set validation after second pilot data collection
- Wound healing effects after application of polyunsaturated fatty acids in rat
- Pressure ulcers in outpatients of the Spinal Unit of University Hospital Brno 2013– 2016
- Supraclavicular flap in reconstruction of intraoral defects
- The pressure ulcers in patients with comorbid neurological disorders
- The factors of pressure ulcer’s healing in critically ill patients
- Factors influencing recurrence of the pressureulcers after plastic surgery – retrospective analysis
- Pressure injuries prevention is better than solving of their complications
- Chondroblastic osteosarcoma of maxilla, a patient with Li- Fraumeni syndrome
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- The pressure ulcers in patients with comorbid neurological disorders
- Chondroblastic osteosarcoma of maxilla, a patient with Li- Fraumeni syndrome
- Supraclavicular flap in reconstruction of intraoral defects
- Pressure lesion monitoring – data set validation after second pilot data collection
