A systematic review of the clinical efficacy of sacroiliac joint stabilization in the treatment of lower back pain
Systematická analýza klinické efektivity stabilizace sakroiliakálního skloubení v rámci terapie bolestí zad
Cíl: Dysfunkce sakroiliakálního skloubení (sacroiliac joint; SIJ) je chronické onemocnění zodpovídající za významné množství případů bolestí zad. Následující práce prezentuje systematickou analýzu odborných článků založených na důkazech týkajících se chirurgického managementu dysfunkce SIJ publikovaných v průběhu posledních 10 let. Jejím hlavním cílem je prezentovat výsledky stran klinické efektivity chirurgické artrodézy SIJ srovnáním předoperačního a pooperačního hodnocení bolesti, a také incidencí chirurgických komplikací.
Metodika: Stratifikace datového souboru byla provedena pomocí algoritmu PRISMA, jehož výsledkem byla skupina 27 studií. Sledovanými parametry byly design studií, počet zařazených pacientů, výskyt chirurgických komplikací, předoperační a pooperační hodnocení Visuální analogové škály bolesti (VAS) a hodnoty Oswestry Disability Index (ODI). Metaanalýza byla provedena na základě modelu s náhodnými efekty, statistická heterogenita byla analyzována pomocí I2 indexu, publikační bias byl analyzován pomocí Eggerova testu a funnel plotu.
Výsledky: Průměrné (95% CI) předoperační hodnoty VAS a ODI dosahovaly 7,86 (7,65–8,07) a 55,1 (49,8–60,5). Pooperačně došlo k poklesu VAS na průměrnou hodnotu 3,23 (2,89–3,58) a poklesu ODI na průměrnou hodnotu 30,7 (25,9–35,5). Celková incidence chirurgických komplikací byla 7,04 %, přičemž průměrná incidence ranných komplikací byla 3,87 % (2,44–6,09) a průměrný výskyt dislokace či malpozice šroubů byl 4,32 % (3,18–5,81). Celkem 5,19 % (3,93–6,83) pacientů vyžadovalo reoperaci.
Závěr: Naše práce demonstrovala významné zlepšení předoperačních hodnot VAS (o 4,6 bodů) a ODI (o 25 bodů) u pacientů, kteří podstoupili chirurgickou stabilizaci SIJ. Tyto výsledky naznačují, že stabilizace SIJ může být u těchto pacientů využitelná a efektivní metoda. Navíc celková morbidita tohoto výkonu se jeví jako nižší, nežli popisovaly předchozí práce. Můžeme očekávat, že v důsledku zlepšujících se chirurgických technik a navigačních metod se bude chirurgická morbidita tohoto výkonu nadále snižovat.
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Článek je podporován interním grantem Krajské zdravotní a.s.
Klíčová slova:
sakroiliakální skloubení – fúze – artrodéza – analýza
Authors:
J. Lodin 1; J. Procházka 2; M. Jelínek 3; P. Waldauf 4
; M. Sameš 1; P. Vachata 1
Authors‘ workplace:
Neurosurgical Department, University of J. E. Purkyne and Masaryk Hospital Krajská Zdravotní a. s., Ústí nad Labem, Czech Republic
1; Chronic Pain Therapy Centre, Ústí nad Labem
2; University of J. E. Purkyne, Ústí nad Labem, Czech Republic
3; Anesthesiology and Intensive Care Department, Královské Vinohrady Faculty Hospital, Prague, Czech Republic
4
Published in:
Cesk Slov Neurol N 2019; 82(6): 655-663
Category:
Original Paper
doi:
https://doi.org/10.14735/amcsnn2019655
Overview
Aim: Sacroiliac joint (SIJ) dysfunction is a chronic disorder, representing a significant cause of lower back pain. This study aims to present an evidence-based systematic analysis of published literature concerning the surgical management of SIJ dysfunction within the last 10 years. Its main goal is to demonstrate the clinical efficacy of SIJ arthrodesis via preoperative and postoperative analysis of patient pain and disability scores, as well as presenting the incidence of surgery-related complications.
Methods: The PRISMA algorithm was used to stratify online search results into 27 studies, which made up our dataset. The parameters collected included study design, number of follow-up patients, surgical complications and preoperative and postoperative Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI) scores. A random effects meta-analysis model was used to analyze the selected data, statistical heterogeneity was assessed using the inconsistency I test, publication bias was analyzed using the funnel plot and Egger’s test.
Results: The mean (95% CI) values of the preoperative VAS and ODI scores were 7.86 (7.65–8.07) and 55.1 (49.8–60.5), resp. These values improved postoperatively to a mean (95% CI) score of 3.23 (2.89–3.58) for VAS and 30.7 (25.9–35.5) for ODI. The total number of recorded surgical complications was 7.04%. The mean (95% CI) incidence of wound complications was 3.87% (2.44–6.09) and the mean (95% CI) proportion of screw dislocation or malposition was 4.32% (3.18–5.81). The proportion (95% CI) of patients requiring a second operation was 5.19% (3.93–6.83).
Conclusion: This study demonstrated that patients indicated for sacroiliac stabilization showed significant improvement in VAS (by 4.6 points) and ODI (by 25 points) scores. These findings suggest that SIJ stabilization is a feasible and effective treatment option for this group of patients. Furthermore, overall morbidity of the procedure was lower than in previously reported studies and is expected to decrease with improvement in surgical technique and navigational imaging.
骶髂关节稳定治疗腰背痛的临床疗效的系统评价
目的:关节(SIJ)功能障碍是一种慢性疾病,代表下腰痛的重要原因。这项研究旨在提供有关过去10年内SIJ功能障碍的外科手术治疗的已发表文献的循证系统分析。其主要目标是通过术前和术后对患者疼痛和残疾评分的分析来证明SIJ关节固定术的临床疗效,并提出与手术相关的并发症的发生率。
方法:使用PRISMA算法将在线搜索结果分层为27个研究,构成了我们的数据集。收集的参数包括研究设计,随访患者数量,手术并发症以及术前和术后视觉模拟量表(VAS)和Oswestry残疾指数(ODI)评分。使用随机效应荟萃分析模型分析选择的数据,使用不一致检验评估统计异质性,使用漏斗图和Egger检验分析产生的偏倚。
结果:术前VAS和ODI评分的平均值(95%CI)分别为7.86(7.65-8.07)和55.1(49.8-60.5)。这些值在术后改善了,VAS的平均评分(95%CI)为3.23(2.89–3.58),ODI的平均评分为30.7(25.9–35.5)。记录的手术并发症总数为7.04%。伤口并发症的平均发生率(95%CI)为3.87%(2.44–6.09),螺丝脱位或错位的平均比率(95%CI)为4.32%(3.18–5.81)。需要再次手术的患者比例(95%CI)为5.19%(3.93-6.83)。
结论:这项研究表明,已指示稳定的患者在VAS评分(由4.6分)和ODI评分(由25分)显着改善。这些发现表明SIJ稳定对于该组患者是可行和有效的治疗选择。此外,该手术的总体发病率低于先前报道的研究,并且随着外科手术技术和导航成像技术的改善,有望降低。
关键词:关节–融合–关节固定–分析
Keywords:
fusion – analysis – sacroiliac joint – arthrodesis
Introduction
Sacroiliac joint (SIJ) dysfunction is defined as a chronically painful SIJ, which is essentially stable and has become disabling to the patient [1]. This clinical condition is increasingly recognized as a significant cause of lower back pain, for which it is responsible in 15–30% of cases [2–4]. This percentage is most likely higher in patients with a history of surgical procedures of the lumbar spine [5–7]. Although the incidence of SIJ dysfunction is relatively high, it commonly remains an unrecognized source of lower back pain, consequently resulting in significant patient disability. Diagnosis of SIJ dysfunction is mostly made per exclusionem, after ruling out more common causes of lower back pain such as lumbar disc disease or spinal stenosis. The diagnosis is confirmed by a combination of clinical manoeuvres and diagnostic intra-articular joint injections [8]. Therapeutic management of this condition is initially conservative, consisting of anti-inflammatory medication, physical therapy and therapeutic injections. In cases where conservative management fails, a surgical therapeutic strategy may be considered. Although several surgical approaches and implant systems are described in the literature, surgical immobilization of the affected joint remains a controversial topic within the neurosurgical and orthopaedic medical communities. A number of review papers attempting to demonstrate the efficacy of these procedures have been published within the last five years [9–11]. This review aims to present an evidence-based systematic analysis of published literature concerning surgical management of SIJ dysfunction within the last 10 years. Its main goal is to demonstrate the clinical efficacy of SIJ arthrodesis via preoperative and postoperative analysis of patient pain and disability scores. The secondary goal is to present the incidence of surgery-related complications in order to quantify morbidity of the procedure.
Methods
We conducted a systematic review of literature concerning surgical management of SIJ dysfunction, following the PRISMA protocol (Fig. 1). The PubMed electronic database was searched using the terms “sacroiliac fusion” and synonyms (sacroiliac joint fusion, sacroiliac joint arthrodesis, sacroiliac fixation, sacroiliac joint stabilization). In addition, datasets of previous meta-analyses were screened for potentially missed papers. Inclusion criteria included original prospective or retrospective studies with cohorts of 2 or more patients, published in the English language, throughout the period from January 1, 2008 to December 31, 2018, with a minimal follow-up period of 6 months. In several cases, patient cohorts of two or more papers were identical or overlapped. In these cases, only the most recent papers with the largest cohort sizes were included in our dataset.
Obr. 1. PRISMA schéma stratifikace dat.
N – počet

Analyzed parameters
The extracted data included study design, original number and number of patients followed up, patients with previous lumbar spine surgical procedures, SIJ dysfunction diagnosis, surgical technique, length of surgery, blood loss, surgical complications, length of follow-up, patient pain and disability scores. For analytic purposes, surgical complications were grouped into three categories: wound complications (infection, haematoma, poor healing, etc.), screw malposition or dislocation and miscellaneous. Furthermore, patients requiring an additional surgical procedure due to a surgical complication formed an additional group. Patient pain scores were analyzed using the Visual Analogue pain Scale (VAS), as this was the most common scale utilized in the analyzed papers. The VAS was recorded on a scale of 0–10, the data from the studies which used the 0–100 scale were divided by a 10 constant, in order to group the data effectively. Various methods for documentation of disability were utilized within the study groups, such as the European Quality of Life-5 Dimensions questionnaire, the Short Form Health Survey and the Oswestry Disability Index (ODI). The ODI was the most frequently used out of these, and as such was the parameter we chose to focus on in our paper. In several cases, pain and disability scores were reported at several follow-up points. In these cases, scores recorded at the longest follow-up period were used in our study.
Statistical assessment
Statistical analysis was performed using R and R markdown software (R Development Core Team, Vienna, Austria). A random-effects meta-analysis (RMA) model was used to calculate the mean preoperative and postoperative values of VAS and ODI, on the basis of VAS and ODI values presented by each individual study. Not all the studies presented standard deviation (SD) intervals along with their VAS and ODI values, the missing data were calculated using multiple imputation in R. Statistical heterogeneity was assessed using the inconsistency I test, with values from 25–50% indicating moderate heterogeneity and values above 50% suggesting high heterogeneity. Publication bias was analyzed using the funnel plot and Egger’s test.
Results
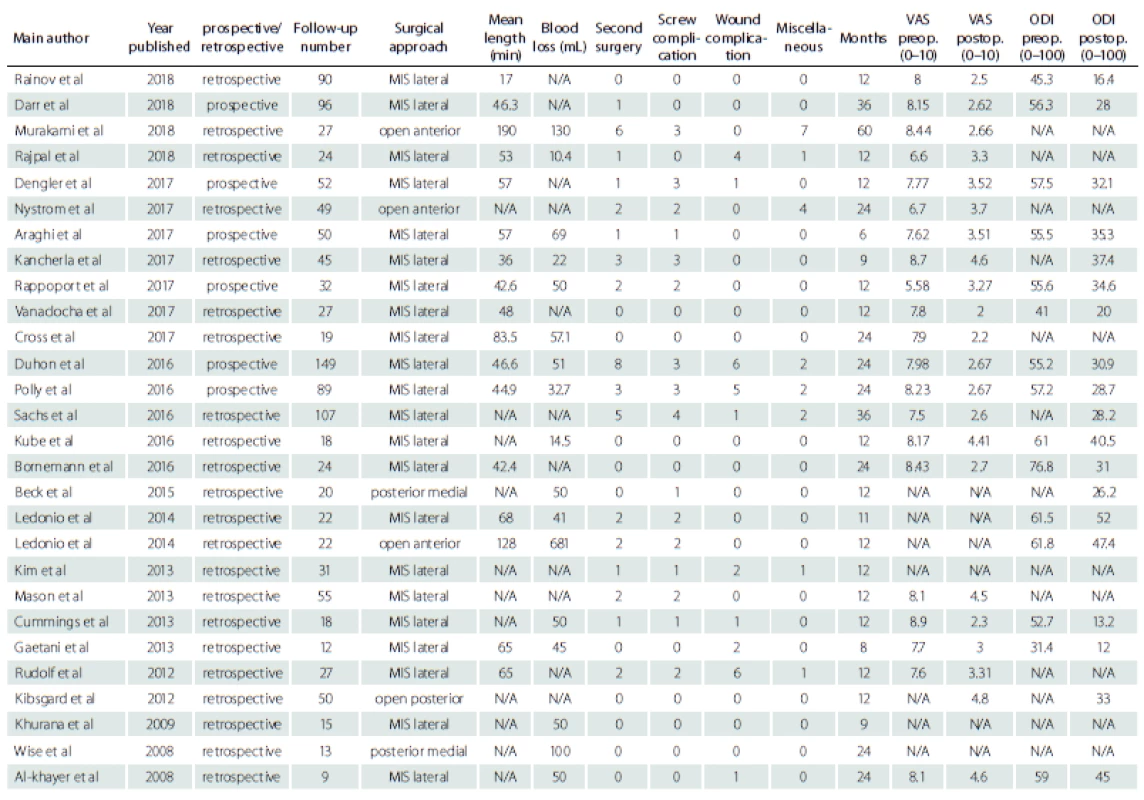
The electronic database search yielded a total of 1,069 papers, which were reduced to 574 available for analysis after filtering out non-English papers and papers published beyond the set time frame. Furthermore, 527 studies were excluded due to their irrelevance, 13 had overlapping cohorts, 4 were systematic reviews and 3 were duplicates. This left 27 papers as our final dataset, which represented 1,192 surgically treated patients (Tab. 1) [12–38]. One study included two patient cohorts treated using different approaches, and as such each patient group was presented separately, forming a total of 28 patient groups for analysis [29]. Of these final papers, 6 had a prospective design and 21 were retrospective. Diagnostic criteria for SIJ dysfunction consisted of clinical signs of SIJ dysfunction including typical pain characteristics and positive provocation tests, as well as a minimum 50% pain reduction following fluoroscopically guided SIJ injections of local anaesthetics and/ or steroids. Conservative treatment was attempted in all surgically treated patients, with insufficient effect on patient pain. Various surgical approaches were used within individual studies, with a minimally invasive lateral approach (MIS) being the most common (21 studies; 77.8%), followed by open approaches (3 studies; 11.1%) and posterior medial oblique approaches (2 studies; 7.4%). One study consisted of two patient cohorts, one operated on using an MIS and the second using an open approach [29]. The length of the follow-up varied amongst individual studies, ranging from 6 to 60 months.
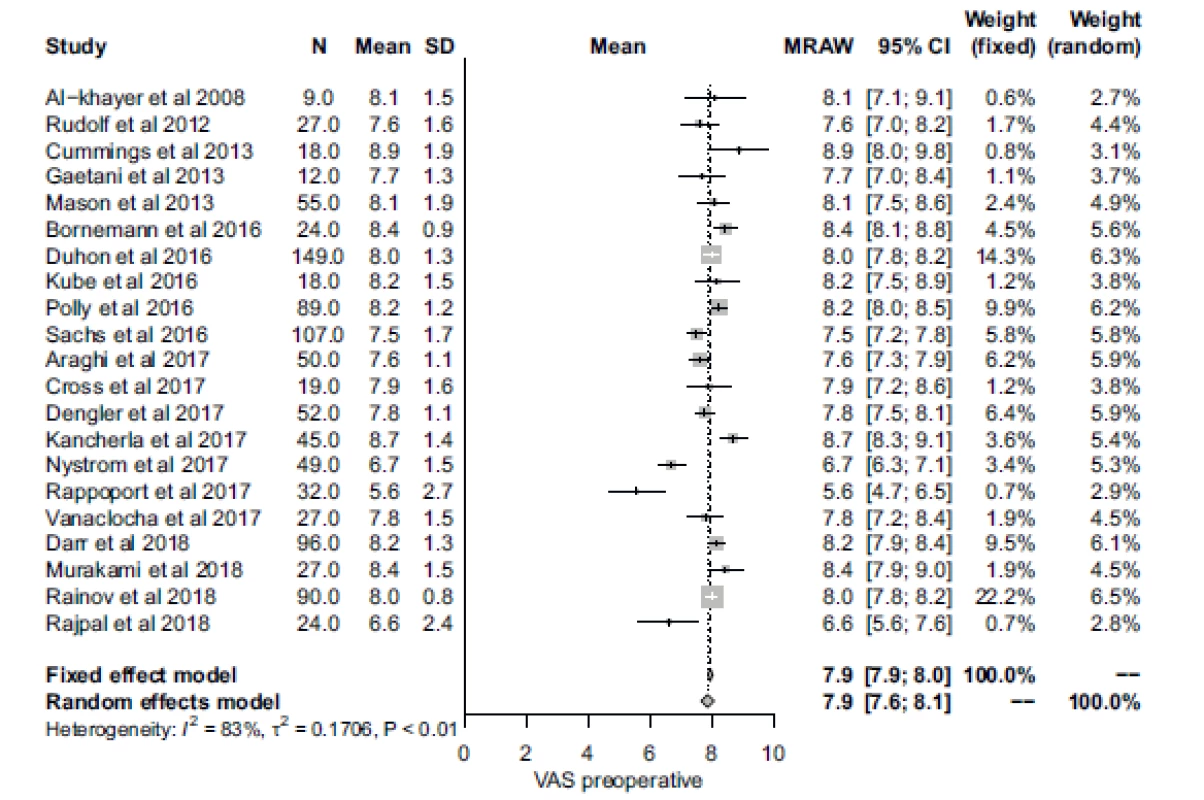
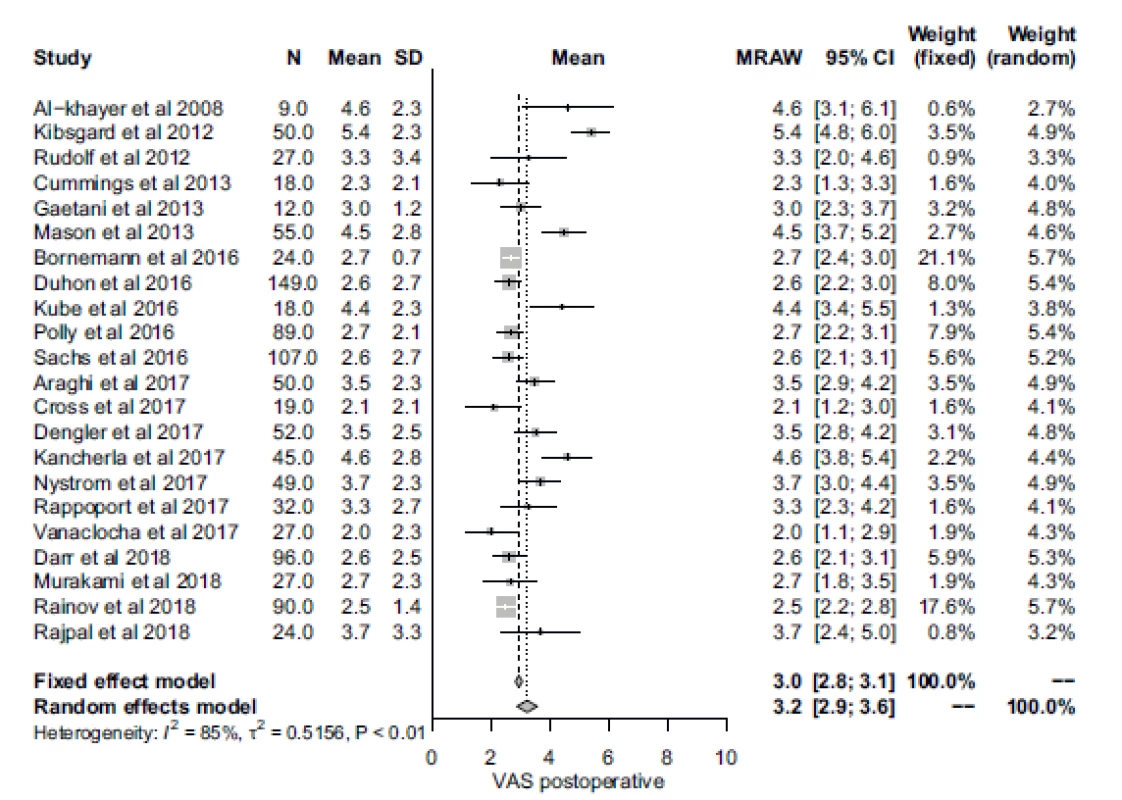
Pain
A total of 21 studies recorded preoperative pain severity using the VAS rating. The RMA mean (95% CI) preoperative VAS score was 7.86 (7.65–8.07) with significant heterogeneity across studies (Fig. 2). Postoperative VAS was reported in 22 studies, with an RMA mean (95% CI) value of 3.23 (2.89–3.58), also with significant heterogeneity (Fig. 3). These values suggest an improvement in pain severity of approximately 4.63 following SIJ surgery.
Obr. 2. Forrestův plot předoperačního skóre Vizuální analogové škály bolesti.
CI – interval spolehlivosti, MRAW – netransformovaný průměr; N – počet; SD – standardní odchylka; VAS – Vizuální analogová škála
Obr. 3. Forrestův plot pooperačního skóre Vizuální analogové škály bolesti.
CI – interval spolehlivosti, MRAW – netransformovaný průměr; N – počet; SD – standardní odchylka; VAS – Vizuální analogová škála
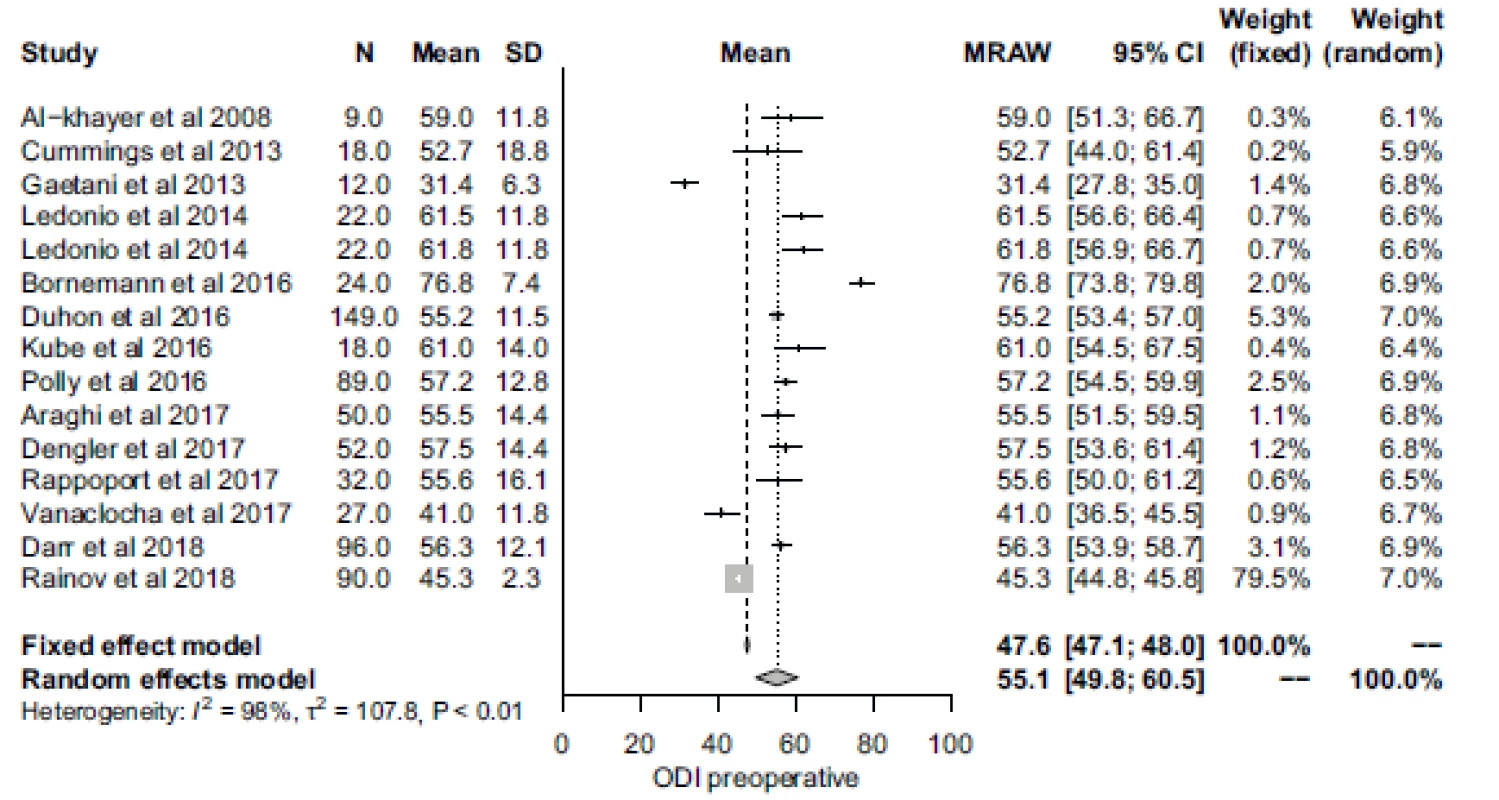
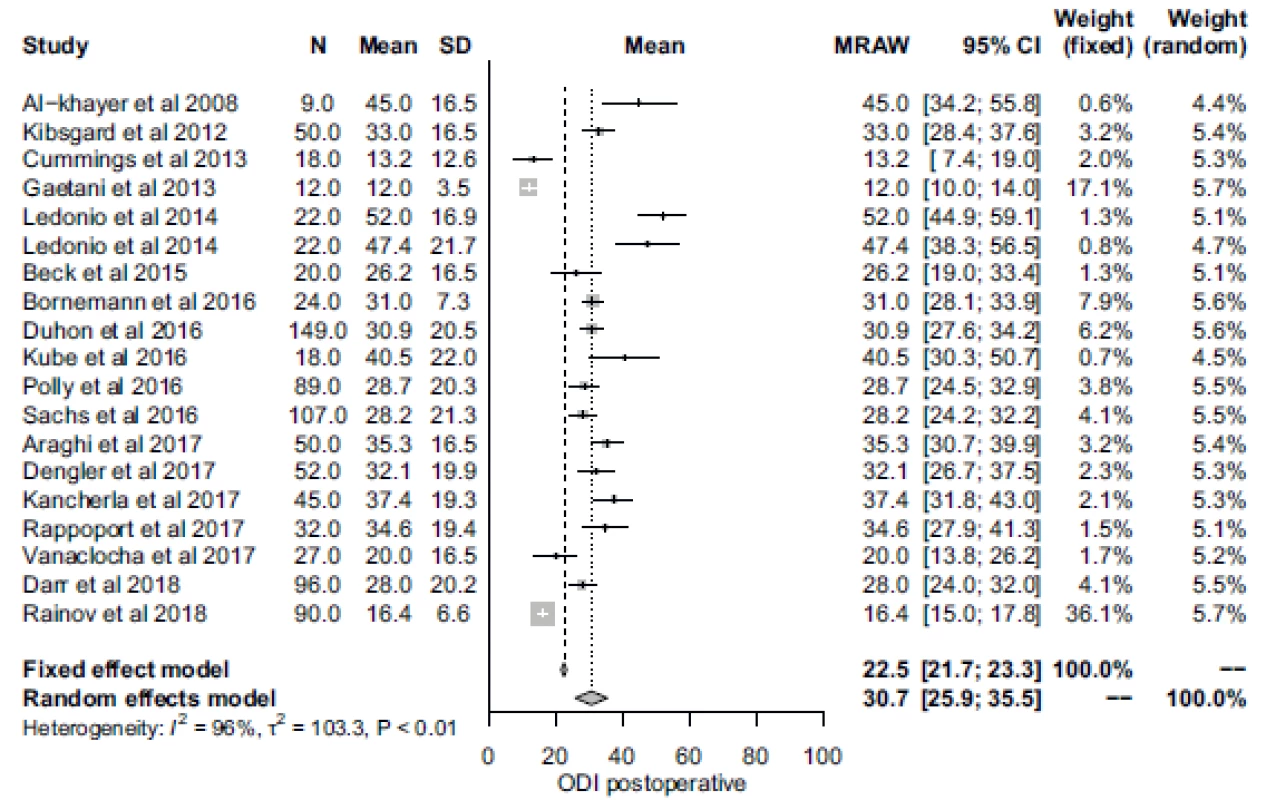
Disability
Preoperative disability described by the ODI was reported in 15 studies. The RMA demonstrated a mean (95% CI) preoperative ODI of 55.1 (49.8–60.5), with significant heterogeneity across studies (Fig. 4). Postoperative ODI scores were recorded in 19 papers, with an RMA mean (95% CI) value of 30.7 (25.9–35.5) with significant heterogeneity amongst studies (Fig. 5).
Obr. 4. Forrestův plot předoperačního skóre Oswestry Disability Index.
CI – interval spolehlivosti, MRAW – netransformovaný průměr; N – počet; ODI – Oswestry Disability Index; SD – standardní odchylka
Obr. 5. Forrestův plot pooperačního skóre Oswestry Disability Index.
CI – interval spolehlivosti, MRAW – netransformovaný průměr; N – počet; ODI – Oswestry Disability Index; SD – standardní odchylka
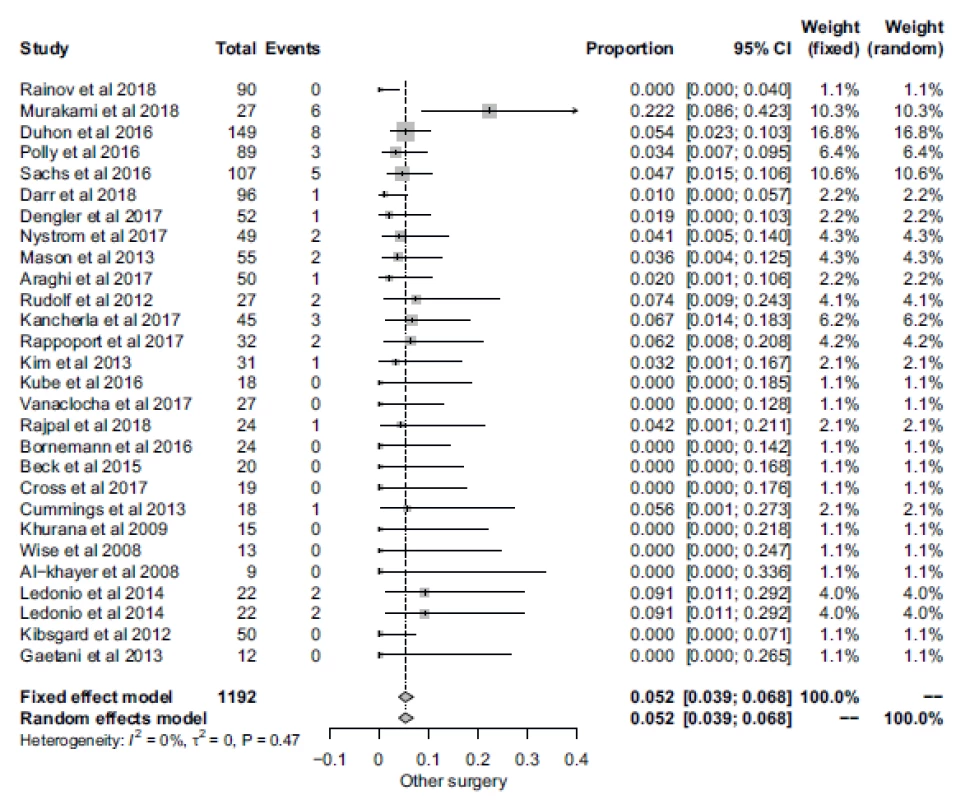
Complications
All the studies reported their individual incidence surgery-related complications. The total incidence of preoperative or postoperative complications was 7.04% (84 cases). The RMA demonstrated the proportion (95% CI) of wound complications at 3.87% (2.44–6.09), with moderate heterogeneity amongst studies. The RMA model showed a mean (95% CI) proportion of screw dislocation or malposition of 4.32% (3.18–5.81), with low heterogeneity. Miscellaneous complications occurred only in isolated cases and as such were not analysed separately. They included cases of vascular injury, urinary retention, postoperative ileus, iliac bone fracture or meralgia paresthetica. Furthermore, RMA was used to analyze the proportion of patients requiring an additional surgical procedure following SIJ stabilization. The proportion (95% CI) of patients requiring a second operation was 5.19% (3.93–6.83), with low heterogeneity across studies (Fig. 6).
Obr. 6. Forrestův plot pacientů vyžadující následný chirurgický výkon.
CI – interval spolehlivosti
Discussion
The main goal of surgical management of SIJ dysfunction is mechanical immobilization of the SIJ via arthrodesis, because pathological intra-articular movements may trigger sensory nerve endings within the joint, which then acts as a pain generator [39]. Various surgical techniques have been described in the literature in order to achieve this goal, however, the efficacy of these procedures remains controversial within the neurosurgical and orthopaedic communities. This is demonstrated by a recent paper by Bina et al, who have questioned the credibility of SIJ dysfunction diagnosis, limited follow-up, as well as the efficacy of SIJ stabilization in achieving arthrodesis, thus limiting SIJ movement [40]. Our study aimed to analyze the current clinical efficacy of SIJ stabilization by comparing mean preoperative VAS and ODI scores of patient cohorts published within the last 10 years. Furthermore, surgery-related complications presented in these studies were collected in order to quantify the relative morbidity of these procedures.
Pain severity
All patient cohorts within our study reporting VAS scores demonstrated an improvement in pain severity. Mean preoperative and postoperative VAS values were 7.86 and 3.23, resp., which shows an improvement of approximately 4.6 on the VAS scale. The VAS is the most common tool for recording patient pain. The advantages include its simple nature and widespread use. The main disadvantage is that the numerical values lack a direct clinical meaning. This has resulted in the implementation of the minimum clinically important difference (MCID), as a means of determining the threshold of achieving effective treatment. MCID of VAS for lower back pain vary within individual studies; mostly they range around a decrease of 2.0 [41–45]. Therefore, an improvement of 4.6 in VAS scores shows a significant decrease in the pain levels of the patients in our study.
Disability
The most common means of documenting disability was the ODI, which was preoperatively recorded in 15 studies and postoperatively in 19 studies. The ODI is a validated questionnaire targeted towards patients with lower back pain and remains the most common tool for documenting disability in these patients. A recent paper by Copay et al demonstrated that ODI could serve as a valid measure of SIJ dysfunction in addition to degenerative spinal disorders [46]. The preoperative and postoperative values of ODI were 55.1 and 30.7, resp., which demonstrates postoperative improvement by approximately 25 points. The MCID for ODI varies between 8–15 points between individual papers [41,42,46]. Nonetheless, a decrease by 25 points represents a significant improvement in disability.
Surgical complications
The extent of surgical morbidity of SIJ stabilization procedures is dependent on several factors including surgical technique, imaging and guidance tools and the surgeon’s experience. In our dataset, the total incidence of complications reported was 7.04%, which falls into the range of 3.5–21.0% reported by previous studies [47–49]. The most common surgical complications were screw malposition or dislocation (4.32%). The rate of these complications is expected to decrease in future with improvement in imaging and navigation techniques. Wound complications occurred in 3.87% of cases and included wound infections or significant postoperative haematomas. In a real world, this number is most likely higher, due to underreporting of these complications, as they are often managed in an out-patient manner. Overall, 5.19% of the patients required a second procedure due to a surgical complication. This statistics is mostly related to the number of malpositioned implants, which was the most common indication for a second surgery. A decrease in the number of malpositioned/ dislocated implants will most likely result in a decrease of the number of patients requiring additional surgery.
Strengths and weaknesses of the study
The strengths of our study include a high number of analyzed studies compared to similar reviews [9–11]. Furthermore, six of the studies analyzed are prospective in design, thus strengthening the validity of our results. All the studies utilized a similar algorithm in diagnosing SIJ dysfunction and mostly recorded VAS and ODI as measurements of pain and disability. Each study addressed the incidence of individual surgical complication as well as the number of patients requiring additional surgery.
The weaknesses of our study include a high heterogeneity of individual studies in various fields, the most important represented by different strategies in recording pain and disability scores. A small number of studies did not use the VAS and ODI as means of describing pain and disability and some studies recorded only the postoperative values of these scales. Furthermore, pain and disability were assessed in a wide range of follow-up visits (6–60 months), which may affect the final value of these scores. Another weakness is combining studies utilizing an open as well as a MIS surgical approach. Due to the fact that both approaches are in essence different, varying surgical and clinical results may be present. Finally, only three of the analyzed papers had a follow-up of more than 24 months, thus limiting our interpretation of truly long-term results of SIJ stabilization.
Conclusion
In conclusion, our study collected data from 27 published studies, which represents 1,192 surgically treated patients with SIJ dysfunction. We demonstrated that patients diagnosed with SIJ dysfunction, who did not benefit from conservative therapy, showed significant improvement in VAS (by 4.6 points) and ODI (by 25 points) scores, following surgical arthrodesis of the SIJ. These findings suggest that SIJ stabilization is a feasible and effective treatment option for this group of patients and that it complements similar reviews performed in the past. Furthermore, the total complication rate in our study is 7.04%, which is lower than in the majority of previously published studies. A further decrease in surgical complications can be expected, especially with the improvement of minimally invasive surgical techniques and navigation imaging. Further prospective randomized studies with long-term follow-up are necessary in order to support surgical management of this group of patients.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Jan Lodin, MD
Neurosurgical Department
J. E. Purkyne of Masaryk Hospital
Krajska Zdravotní a.s.,
Sociální Péče 3316/12A
400 11 Ústí nad Labem
Czech Republic
e-mail: jan_lodin@hotmail.com
Accepted for review: 10. 5. 2019
Accepted for print: 3. 10. 2019
Sources
1. Zelle BA, Gruen GS, Brown S et al. Sacroiliac joint dysfunction: evaluation and management. Clin J Pain 2005; 21(5): 446–455.
2. Sembrano JN, Polly DW Jr. How often is low back pain not coming from the back? Spine (Phila Pa 1976) 2009; 34(1): E27–E32.
3. Irwin RW, Watson T, Minick RP et al. Age, body mass index, and gender differences in sacroiliac joint pathology. Am J Phys Med Rehabil 2007; 86(1): 37–44. doi: 10.1097/ phm.0b013e31802b8554.
4. Bernard TN Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res 1987; (217): 266–280.
5. Unoki E, Abe E, Murai H et al. Fusion of multiple segments can increase the incidence of sacroiliac joint pain after lumbar or lumbosacral fusion. Spine (Phila Pa 1976) 2016; 41(12): 999–1005. doi: 10.1097/ BRS.0000000000001409.
6. Schomacher M, Kunhardt O, Koeppen D et al. Transient sacroiliac joint-related pain is a common problem following lumbar decompressive surgery without instrumentation. Clin Neurol Neurosurg 2015; 139 : 81–85. doi: 10.1016/ j.clineuro.2015.09.007.
7. Liliang PC, Lu K, Liang CL et al. Sacroiliac joint pain after lumbar and lumbosacral fusion: findings using dual sacroiliac joint blocks. Pain Med 2011; 12(4): 565–570. doi: 10.1111/ j.1526-4637.2011.01087.x.
8. Schmidt GL, Bhandutia AK, Altman DT. Management of sacroiliac joint pain. J Am Acad Orthop Surg 2018; 26(17): 610–616. doi: 10.5435/ JAAOS-D-15-00063.
9. Zaidi HA, Montoure AJ, Dickman CA. Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. J Neurosurg Spine 2015; 23(1): 59–66. doi: 10.3171/ 2014.10.SPINE14516.
10. Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg 2015; 9 : 40. doi: 10.14444/ 2040.
11. Lingutla KK, Pollock R, Ahuja S. Sacroiliac joint fusion for low back pain: a systematic review and meta-analysis. Eur Spine J 2016; 25(6): 1924–1931. doi: 10.1007/ s00586-016-4490-8.
12. Rainov NG, Schneiderhan R, Heidecke V. Triangular titanium implants for sacroiliac joint fusion. Eur Spine J 2019; 28(4): 727–734. doi: 10.1007/ s00586-018-5860-1.
13. Rajpal S, Burneikiene S. Minimally Invasive sacroiliac joint fusion with cylindrical threaded implants using intraoperative stereotactic navigation. World Neurosurg 2019; 122: e1588–e1591. doi: 10.1016/ j.wneu.2018.11.116.
14. Darr E, Cher D. Four-year outcomes after minimally invasive transiliac sacroiliac joint fusion with triangular titanium implants. Med Devices (Auckl) 2018; 11 : 287–289. doi: 10.2147/ MDER.S179003.
15. Murakami E, Kurosawa D, Aizawa T. Sacroiliac joint arthrodesis for chronic sacroiliac joint pain: an anterior approach and clinical outcomes with a minimum 5-year follow-up. J Neurosurg Spine 2018; 29(3): 279–285. doi: 10.3171/ 2018.1.SPINE17115.
16. Vanaclocha V, Herrera JM, Saiz-Sapena N et al. Minimally invasive sacroiliac joint fusion, radiofrequency denervation, and conservative management for sacroiliac joint pain: 6-year comparative case series. Neurosurgery 2018; 82(1): 48–55. doi: 10.1093/ neuros/ nyx185.
17. Cross WW, Delbridge A, Hales D et al. Minimally invasive sacroiliac joint fusion: 2-year radiographic and clinical outcomes with a principles-based SIJ fusion system. Open Orthop J 2018; 12 : 7–16. doi: 10.2174/ 1874325001812010007.
18. Rappoport LH, Luna IY, Joshua G. Minimally invasive sacroiliac joint fusion using a novel hydroxyapatite-coated screw: preliminary 1-year clinical and radiographic results of a 2-year prospective study. World Neurosurg 2017; 101 : 493–497. doi: 10.1016/ j.wneu.2017.02.046.
19. Araghi A, Woodruff R, Colle K et al. Pain and opioid use outcomes following minimally invasive sacroiliac joint fusion with decortication and bone grafting: the evolusion clinical trial. Open Orthop J 2017; 11 : 1440–1448. doi: 10.2174/ 1874325001711011440.
20. Nystrom B, Gregebo B, Taube A et al. Clinical outcome following anterior arthrodesis in patients with presumed sacroiliac joint pain. Scand J Pain 2017; 17 : 22–29. doi: 10.1016/ j.sjpain.2017.06.005.
21. Bornemann R, Roessler PP, Strauss AC et al. Two--year clinical results of patients with sacroiliac joint syndrome treated by arthrodesis using a triangular implant system. Technol Health Care 2017; 25(2): 319–325. doi: 10.3233/ THC-161272.
22. Dengler JD, Kools D, Pflugmacher R et al. 1-year results of a randomized controlled trial of conservative management vs. minimally invasive surgical treatment for sacroiliac joint pain. Pain Physician 2017; 20(6): 537–550.
23. Kancherla VK, McGowan SM, Audley BN et al. Patient reported outcomes from sacroiliac joint fusion. Asian Spine J 2017; 11(1): 120–126. doi: 10.4184/ asj.2017.11 .1.120.
24. Sachs D, Kovalsky D, Redmond A et al. Durable intermediate-to long-term outcomes after minimally invasive transiliac sacroiliac joint fusion using triangular titanium implants. Med Devices (Auckl) 2016; 9 : 213–222. doi: 10.2147/ MDER.S109276.
25. Kube RA, Muir JM. sacroiliac joint fusion: one year clinical and radiographic results following minimally invasive sacroiliac joint fusion surgery. Open Orthop J 2016; 10 : 679–689. doi: 10.2174/ 1874325001610010679.
26. Polly DW, Swofford J, Whang PG et al. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg 2016; 10 : 28. doi: 10.14444/ 3028.
27. Duhon BS, Bitan F, Lockstadt H et al. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int J Spine Surg 2016; 10 : 13.
28. Beck CE, Jacobson S, Thomasson E. A Retrospective outcomes study of 20 sacroiliac joint fusion patients. Cureus 2015; 7(4): e260. doi: 10.7759/ cureus.260.
29. Ledonio CG, Polly DW Jr, Swiontkowski MF. Mini-mally invasive versus open sacroiliac joint fusion:are they similarly safe and effective? Clin Orthop Relat Res 2014; 472(6): 1831–1838. doi: 10.1007/ s11999-014-3499-8.
30. Kim JT, Rudolf LM, Glaser JA. Outcome of percutaneous sacroiliac joint fixation with porous plasma-coated triangular titanium implants: an independent review. Open Orthop J 2013; 7 : 51–56. doi: 10.2174/ 18743 25001307010051.
31. Mason LW, Chopra I, Mohanty K. The percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: a prospective outcome study. Eur Spine J 2013; 22(10): 2325–2331. doi: 10.1007/ s00586-013-2825-2.
32. Cummings J Jr, Capobianco RA. Minimally invasive sacroiliac joint fusion: one-year outcomes in 18 patients. Ann Surg Innov Res 2013; 7(1): 12. doi: 10.1186/ 1750-1164-7-12.
33. Kibsgard TJ, Roise O, Sudmann E et al. Pelvic joint fusions in patients with chronic pelvic girdle pain: a 23--year follow-up. Eur Spine J 2013; 22(4): 871–877. doi: 10.1007/ s00586-012-2512-8.
34. Gaetani P, Miotti D, Risso A et al. Percutaneous arthrodesis of sacro-iliac joint: a pilot study. J Neurosurg Sci 2013; 57(4): 297–301.
35. Rudolf L. Sacroiliac joint arthrodesis – MIS technique with titanium implants: report of the first 50 patients and outcomes. Open Orthop J 2012; 6 : 495–502. doi: 10.2174/ 1874325001206010495.
36. Khurana A, Guha AR, Mohanty K et al. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br 2009; 91(5): 627–631. doi: 10.1302/ 0301-620X.91B5.21519.
37. Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 2008; 21(8): 579–584. doi: 10.1097/ BSD.0b013e31815ecc4b.
38. Al-Khayer A, Hegarty J, Hahn D et al. Percutaneous sacroiliac joint arthrodesis: a novel technique. J Spinal Disord Tech 2008; 21(5): 359–363. doi: 10.1097/ BSD. 0b013e318145ab96.
39. Rashbaum RF, Ohnmeiss DD, Lindley EM et al. Sacroiliac joint pain and its treatment. Clin Spine Surg 2016; 29(2): 42–48. doi: 10.1097/ BSD.0000000000000359.
40. Bina RW, Hurlbert RJ. Sacroiliac fusion: another „magic bullet“ destined for disrepute. Neurosurg Clin N Am 2017; 28(3): 313–320. doi: 10.1016/ j.nec.2017.02.001.
41. Parker SL, Mendenhall SK, Shau DN et al. Minimum clinically important difference in pain, disability, and quality of life after neural decompression and fusion for same-level recurrent lumbar stenosis: understanding clinical versus statistical significance. J Neurosurg Spine 2012; 16(5): 471–478. doi: 10.3171/ 2012.1.SPINE11842.
42. Copay AG, Glassman SD, Subach BR et al. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study Questionnaire Short Form 36, and pain scales. Spine J 2008; 8(6): 968–974. doi: 10.1016/ j.spinee.2007.11.006.
43. Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005; 30(11): 1331–1334. doi: 10.1097/ 01.brs.0000164099.92112.29.
44. Ostelo RW, Deyo RA, Stratford P et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 2008; 33(1): 90–94. doi: 10.1097/ BRS.0b013e31815e3a10.
45. Mannion AF, Balague F, Pellise F et al. Pain measurement in patients with low back pain. Nat Clin Pract Rheumatol 2007; 3(11): 610–618. doi: 10.1038/ ncprheum0646.
46. Copay AG, Cher DJ. Is the Oswestry Disability Index a valid measure of response to sacroiliac joint treatment? Qual Life Res 2016; 25(2): 283–292. doi: 10.1007/ s11136-015-1095-3.
47. Smith AG, Capobianco R, Cher D et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 2013; 7(1): 14. doi: 10.1186/ 1750-1164-7-14.
48. Miller LE, Reckling WC, Block JE. Analysis of postmarket complaints database for the iFuse SI Joint Fusion System(R): a minimally invasive treatment for degenerative sacroiliitis and sacroiliac joint disruption. Med Devices (Auckl) 2013; 6 : 77–84. doi: 10.2147/ MDER.S44690.
49. Schoell K, Buser Z, Jakoi A et al. Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J 2016; 16(11): 1324–1332. doi: 10.1016/ j.spinee.2016.06.016.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2019 Issue 6
- Advances in the Treatment of Myasthenia Gravis on the Horizon
- Memantine Eases Daily Life for Patients and Caregivers
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
-
All articles in this issue
- Gunshot injury of the brain
- Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke? YES
- Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke? NO
- Are ticagrelor and prasugrel an alternative in the antiplatelet treatment of ischemic stroke?
- Cervical plexus lesions in clinical practice
- Neurorehabilitation of gait impairment using functional electrical stimulation – current findings from randomized clinical trials
- Difficulty in respecting autonomy in patients with Parkinson’s disease
- Current management of patients with degenerative cervical spine compression
- Surgical treatment of bilateral drug-resistant Menière’s disease
- Mechanical thrombectomy in the treatment of acute ischemic stroke in childhood
- Doporučení pro mechanickou trombektomii akutního mozkového infarktu – verze 2019
- Osmdesátiny doc. MU Dr. Jiřího Bauera, CSc.
- Intraplaque hemorrhage in symptomatic and asymptomatic progressive internal carotid artery stenosis – a pilot study
- Significant fall risk factors in the personal history of in-patients with neurological disease
- Spinal meningiomas – 92 patients operated at our department
- Civilian and military gunshot wounds to the head
- Epidural application of steroids Part 1 – Patient profile before application
- Facial nerve reconstruction with great auricular nerve graft following resection of recurrent basal cell carcinoma in parotidomasseteric region
- A comparison of perioperative pressure measurements in the aneurysm sac and parent artery in ruptured and unruptured aneurysm
- A systematic review of the clinical efficacy of sacroiliac joint stabilization in the treatment of lower back pain
- Does choroidal thickness change in Parkinson’s disease?
- Conservative management of a ruptured Galassi III middle fossa arachnoid cyst
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Cervical plexus lesions in clinical practice
- Doporučení pro mechanickou trombektomii akutního mozkového infarktu – verze 2019
- Mechanical thrombectomy in the treatment of acute ischemic stroke in childhood
- Gunshot injury of the brain
