Hybrid short-wire ERCP technique, five years of experience
Pětiletá zkušenost s hybridní ERCP technikou s krátkým vodičem
Úvod: Cílem této práce je představit novou hybridní techniku endoskopické retrográdní cholangiopankreatikografie (ERCP) využívající krátké vodiče v kombinaci s akcesorii navrženými jak pro dlouhý, tak pro krátký systém. Technika je založena na vnitřním uzamčení krátkého vodiče, kanylaci prováděné asistentem a možnosti cílit polohu vodiče lékařem. Materiál a metody: ERCP byly prováděny duodenoskopy firmy Olympus s použitím krátkých vodičů (260–270 cm) a akcesorií určenými pro krátký i dlouhý systém. Byla srovnávána rychlost zavádění akcesorií po vodiči a incidence post-ERCP pankreatitidy (PEP) v případě použití hybridní techniky a dlouhé metody. Dále byla sledována úspěšnost kanylací, procento krvácivých komplikací a cholangoitidy. Výsledky: Od roku 2016 do roku 2020 bylo provedeno celkem 1 506 ERCP. Hybridní technika byla použita u 58,2 % (2017), 88,5 % (2018), 91,3 % (2019) a 98,5 % (2020) výkonů. Úspěšnost kanylací byla 94,73 %. Průměrná doba zavádění akcesorií po vodiči pracovním kanálem byla 15 s (cv = 0,12; σ = 1,91) při použití krátkého vodiče s V-systémem, 31 s (cv = 0,08; σ = 2,67) při použití dlouhého vodiče s V-systémem a 55 s (cv = 0,06; σ = 3.34) při použití dlouhého vodiče a endoskopu bez možnosti fixace vodiče. Komplikace výkonů se vyskytly v 5,26 % a všechny byly nezávažné. Byl prokázán nižší výskyt PEP s použitím krátkého vodiče oproti dlouhému vodiči (1 % vs. 4 %, P = 0.033). Závěr: Naše retrospektivní analýza hybridní ERCP techniky prokazuje rychlejší zavedení akcesorií a nižší míru PEP ve srovnání s dlouhou metodou. Zaznamenali jsme nízký výskyt krvácení a infekčních komplikací, zřejmě díky snadné a rychlé manipulaci s krátkým vodičem.
Klíčová slova:
endoskopická retrográdní cholangiopankreatikografie – vodiče – krátký systém – dlouhý systém – hybridní ERCP technika
Authors:
Maceček J.; Staňka B.; Konvička P.
Authors‘ workplace:
Gastroenterology Department, AGEL Středomoravská nemocniční a. s. – AGEL Prostějov Hospital
Published in:
Gastroent Hepatol 2021; 75(3): 200-206
Category:
doi:
https://doi.org/10.48095/ccgh2021200
Overview
Backgrounds: The aim of this work is to present the novel hybrid endoscopic retrograde cholangiopancreatography (ERCP) technique using short guidewires and accessories designed for long and short systems. The technique is based on the internal locking capability of the short guidewire, assistant wire control and the possibility of targeting the wire by a physician. Material and methods: ERCPs were performed with Olympus duodenoscopes, using a short guidewire (260–270 cm) and accessories designed for short - and long-wire systems. The speed of deployment of the accessories and incidence of post-ERCP pancreatitis (PEP) when using the short-wire hybrid technique were compared with the same parameters when using a long-wire system. The success of cannulations, the percentage of bleeding and cholangitis were monitored. Results: From 2016 to 2020, a total number of 1,506 ERCPs were done. Hybrid technique was used in 58.2% (2017), 88.5% (2018), 91.3% (2019) and 98.5% (2020) of the procedures. The cannulation success rate was 94.73%. The average accessory insertion times through the working channel were 15 s (cv = 0.12, σ = 1.91) when using a short guidewire and a V-system, 31 s (cv = 0.08, σ = 2.67) when using a long guidewire and a V-system and 55 s (cv = 0.06, σ = 3.34) when using a long guidewire and an endoscope without a locking device. The rate of complications was 5.26% and none of them was severe. A lower incidence of PEP with a short guidewire than with a long one (1% vs. 4%, P = 0.033) was demonstrated. Conclusion: Our retrospective analysis of the ERCP hybrid technique highlights faster deployment of accessories and a lower PEP rate compared to the long-wire method. We noticed low bleeding and infectious complications apparently due to easy and quick handling of the short guidewire.
Keywords:
endoscopic retrograde cholangiopancreatography – guidewires – short-wire system – long-wire system – hybrid ERCP technique
Introduction
A guidewire for ERCP is an accessory for bile or pancreatic cannulation and traversal strictures to achieve accessory placement [1]. A proper guidewire increases the success rate of selective cannulation. The wire-guided cannulation technique is superior to the contrast-guided cannulation technique and reduces the incidence of PEP [2].
Guidewires differ in material composition, flexibility, diameter, shape of the terminal part and length. It is the length of the guidewire that is one of the basic parameters that determines the resulting diagnostic and therapeutic effect of the entire procedure. The long-wire ERCP system with the respective accessories is still traditionally used in the Czech Republic. The basis is cannulation performed by an assistant (nurse) .
Due to the technical progress, a short--wire system, using a significantly shorter guidewire, was created. The physician can thus perform the cannulation without assistance. The accessories also had to adapt to this technique. The choice of the optimal technique is important to achieve successful cannulation, to minimise the procedure duration with a low complication rate. The aim of this work is to present the novel ERCP hybrid technique using Olympus endoscopes with a V-locking system and demonstrating the combination of a short guidewire with accessories designed for both long and short systems and demonstrate basic statistical data. This concept combines the advantages of the long-wire and short-wire systems.
Material and methods
An analysis of basic data from all ERCPs from 2016 to 2020 and a more detailed analysis of the previous year (2020) was done. ERCPs were performed by two endoscopists, both with five years of experience in this technique, using Olympus TJF-Q180V endoscopes (V-locking system) and in the minority of cases with Olympus TJF 145 endoscopes (without a locking system). Various accessories (Olympus, Boston Scientific, COOK, Endoflex, Medwork) were used, such as sphincterotomes, Dormia baskets, extraction and dilation balloons, brushes, plastic and metal stents, inserted along the guidewires. For almost all ERCPs, 260 cm long Dreamwire (10 cm hydrophilic tip, Boston scientific), Jagwire (5 cm hydrophilic tip, Boston Scientific) or VisiGlide 2 (270 cm long, 7 cm hydrophilic tip, Olympus), 0.025 - and 0.035-inch wide, were used. When using an older type of endoscope without a V-system, long wires (450–480 cm, Boston Scientific, Olympus, or COOK) are necessary.
The total number of procedures, percentage of procedures using a short wire, indications, technical feasibility, bleeding and infectious complications were monitored. The speeds of accessory deployment and incidence of PEP when using the short-wire hybrid technique were compared with the same parameters when using a long-wire system. The speeds of accessory deployment were measured in three groups, each with 50 randomly selected patients (short-wire and V-system/ long-wire and V-system/ long-wire and endoscope without V-system). The incidences of PEP were measured in two groups, each with 285 patients (hybrid ERCP technique group/ long-wire method group).
Results
From 2016 to 2020, a total of 1,506 ERCPs were done (Graph 1). The decline in the number of procedures in 2020 was caused by the COVID-19 infection. The average age of the patients was 69 years, the age range was 25 to 95 years and the median was 71 years.
Graf 1. Počet provedených ERCP v letech 2016–2020; osa x – roky, osa y – počet
ERCP.

Due to the acquisition of Olympus endoscopes with a V-system in 2016, the ERCP procedures were gradually switched to the short guidewire technique. The V-system and RX (rapid exchange) system were tested in 2016, first with long wires. In 2016, all ERCPs were performed using the long guidewires.
It has been found that short guidewires can be used for the accessory designed for both the short - and the long--wire systems due to the fixation of the guidewire at the distal end of the endoscope and a sufficient length of commonly used accessories. The sum of the lengths of the bile or pancreatic ducts (approximately 15–20 cm), the working channel (approximately 140 cm), handling length with inserted guidewire alone (100–120 cm) and handling length of the wire with inserted accessory (approximately 50–60 cm) shows that the short guidewire length (260–270 cm) is sufficient due to internal and external locking devices.
Since 2017, the switch to ERCPs with a short wire has been gradually implemented and a ‘hybrid technique’ using a short guidewire and accessories suitable for both short and long systems have been implemented in our practice. The following histogram shows the percentage distribution of short-wire (hybrid technique) and long-wire ERCP over the years. We use long wires in clinical practice only when an endoscope with a locking system is unavailable (Graph 2).
Graf 2. Procentuální zastoupení ERCP s krátkým (hybridní technika)
a dlouhým vodičem v letech 2016 až 2020; osa x – roky, osa y – procentuální
zastoupení.

The wire itself, in the case of the hybrid technique, is controlled by a nurse during cannulation. The advantages of this technique are shorter accessory exchange and the lower rate of certain complications. The average time of insertion of the accessory from the moment it is threaded on the wire until the moment it appears at the distal end of the endoscope is much shorter when a short wire is used. When using a short wire and V-system it is 15 s (cv = 0.12, σ = 1.91), when using a long wire and V-system it is 31 s (cv = 0.08, σ = 2.67) and when using a long wire and endoscope without locking the wire it is 55 s (cv = 0.06, σ = 3.34). The total number of complications amounted to 5.26% and all were then treated conservatively without surgery. No perforation was done. There was a lower incidence of PEP with the short-wire hybrid technique than with the long-wire system (1% [2020] vs. 4% [2016, 2017], P = 0.033), however this parameter may be skewed by greater endoscopic experience in 2020.
Bleeding and cholangitis after hybrid ERCP technique occurred in 1.75% and 2.1% of patients, respectively, which is consistent with the results of some studies (see discussion).
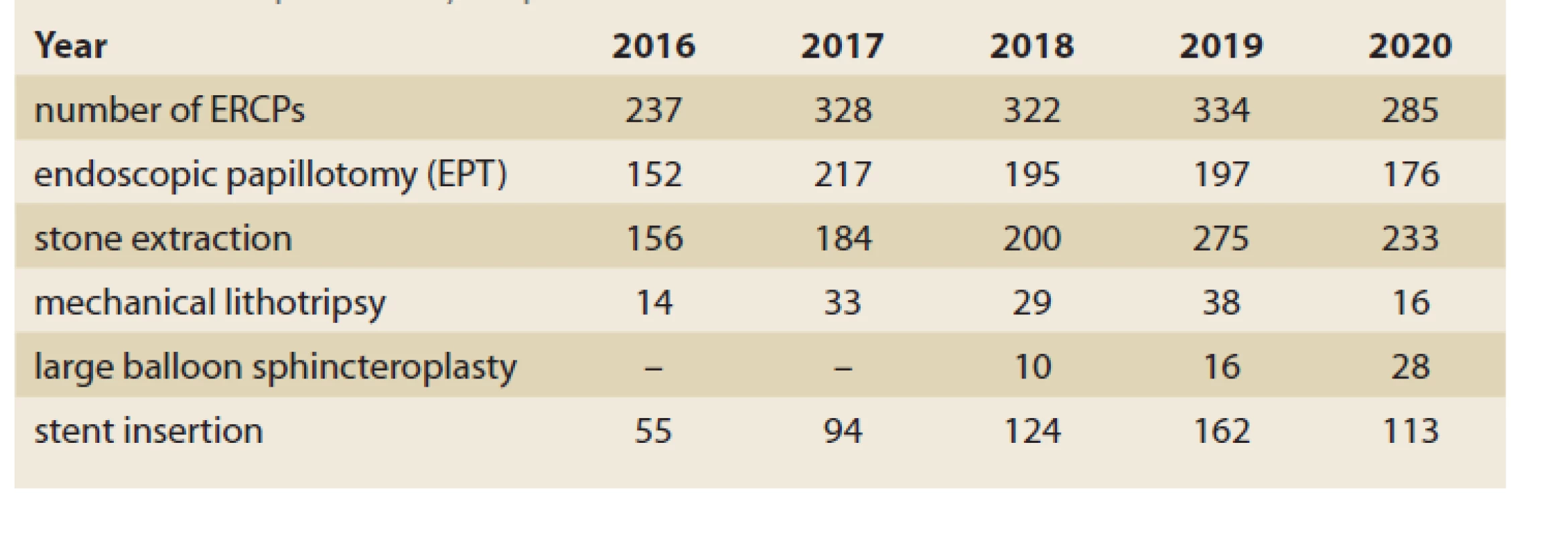
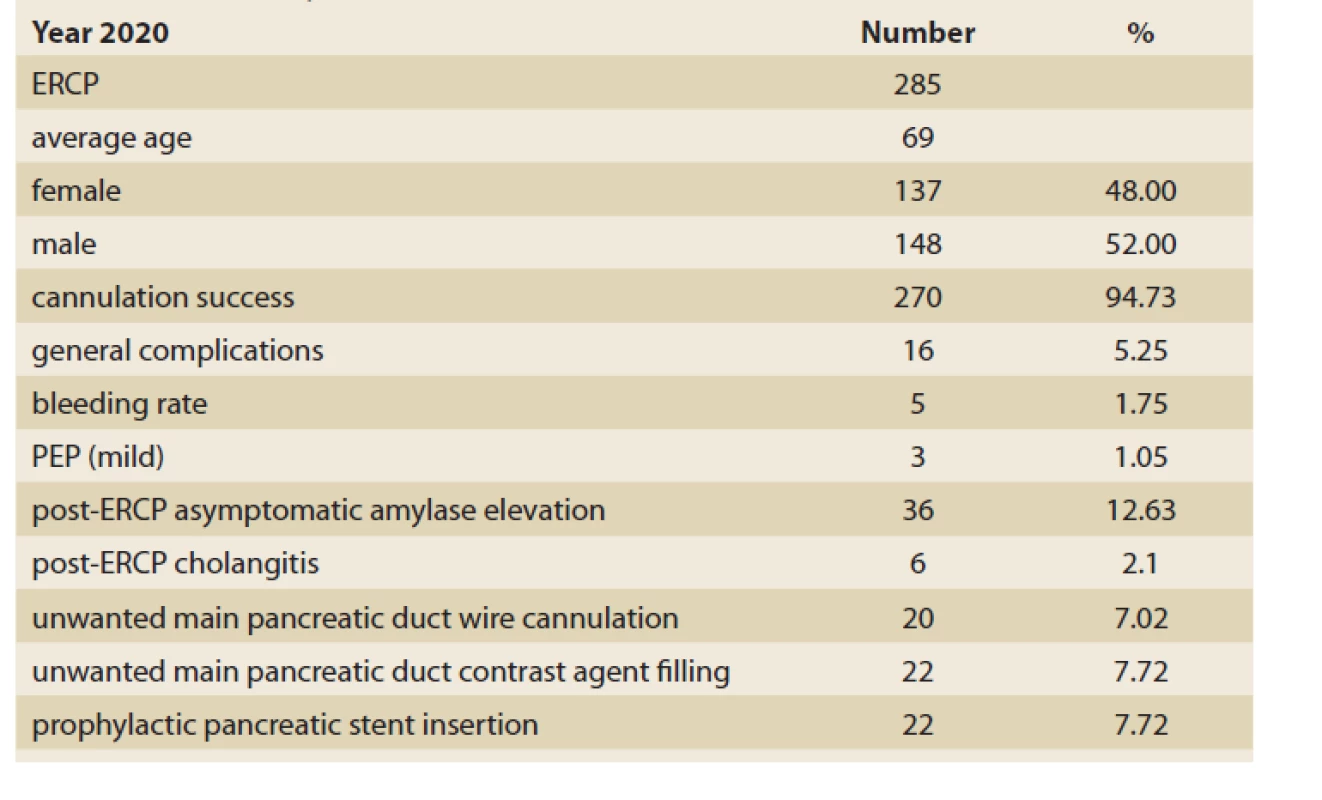
In addition to the speed of faster accessory exchange, easy handling of the guidewire is an advantage for the assistant due to its length and simple adjustment of the position of the wire, or targeted cannulation by a physician at the time of accessory exchange. If accessories dedicated to the short system are used, a smooth transition to physician--controlled cannulation is possible. The cannulation success rate at our workplace was 94.73 with the use of a hybrid technique. Tab. 1 shows some ERCP parameters for the last 5 years and demonstrates the possibility of performing all basic therapeutic modalities with a short wire. Tab. 2 presents some data for the last year.
Tab. 1. ERCP parametry za posledních 5 let.
Tab. 2. ERCP data pro rok 2020.
Discussion
Guidewires are used in nearly every ERCP to gain access to the biliary or pancreatic duct and help to insert various devices. The wire-guided cannulation technique is the basis of the success of any ERCP. Guidewires consist of a stiff shaft for guiding the passage of various accessories and a hydrophilic flexible tip area for tracking and entering desired routes. Most of the modern guidewires have a monofilament core made of stainless steel, nitinol, or a shape-memory alloy, and an outer sheath coated with Teflon, polyurethane, or other polymers to reduce surface friction. The length of a guidewire ranges from 150 to 650 cm. The thickness of a guidewire ranges from 0.46 to 0.97 mm (0.018 - to 0.038-inch). In clinical practice, the most commonly used guidewires are 0.025 - and 0.035-inch in diameter [3], which were also used in our analysis. Despite the various attributes of the guidewires, the important parameter is its length. Based on this parameter, two ERCP approaches exist: the long-wire system and short-wire system.
The limitations of the traditional long--wire system gradually led to the introduction of different short-wire systems. A common principle of the short-wire system is locking a short wire in position to allow the advancement or removal of various devices without displacement of the wire. In clinical practice the RX, Fusion and V-system are used preferentially. The use of the short-wire system leads to reduction of the procedure time, decreased sedation requirements and improved guidewire stability, and it allows the endoscopist to control the guidewire, which can reduce the side effects of ERCP [4]. In other countries, the short system is used more often than the long system (data on file – Boston Scientific). In the Czech Republic it is used only rarely.
The use of long guidewires was necessary due to the design imperfections of endoscopes and accessories. The length of a typical long wire used for ERCP ranges from 420 to 480 cm. The length of the guidewire is approximately twice the length of the accessory inserted along the wire. This is necessary due to the absence of a device for locking the wire in the optimal position. This excessive length creates several problems. Since the assistant is in control of the wire and the physician is in control of the ERCP device, excellent communication between the physician and assistant is required. Disorder of mutual coordination leads to loss of access, difficult cannulation and problems with advancing the wire to the desired target. The main problem is that the assistant must coordinate many activities at one time and avoid contamination of the wire with the floor surface [5]. Repositioning or loss of access to either the bile or pancreatic duct and the length of the wire in general may lead to increases in procedure duration, radiation exposure, failure of the procedure and even the probability of side effects [6].
The short system is able to be put into practice primarily thanks to the structural improvement of endoscopes and accessories. Endoscopic assistants have been and are essential to the successful ERCP, but the ability of the endoscopists to manage the guidewire and the scope independently was considered an advantage during these procedures. All short-wire systems are based on locking the wire in position to allow device exchange over short guidewires (185–270 cm) while maintaining access. Device exchanges are possible by either fixation of the wire externally at the biopsy port or internally at the elevator. A locking system and accessory design allow the physician to control the guidewire [7].
There are three short-wire ERCP proprietary systems available. These systems integrate cannulation, sphincterotomy, balloon extraction, balloon dilation and biliary stenting devices. The same short-wire devices can be used with traditional long wires if needed.
The RX system (Boston Scientific Corporation, Natick, MA, USA) was the first short-wire system, introduced in 1999. This system incorporates three components. The RX locking device has an external lock that may fix one or two guidewires. A biopsy port cap minimises air or bile leakage during the procedure. RX-compatible biliary devices include both open ‘tear away’ channel monorail designs used with sphincterotomes and catheters, as well as short-track designs used with cytology catheters, stone extraction balloons, dilating balloons and stents. The last component includes the 260 cm long 0.035-inch or 0.025-inch wide Jagwire with a coated firm shaft, flexible hydrophilic leading tip, and two--coloured markings [7].
The Fusion system (Cook Endoscopy; Winston-Salem, NC, USA) was introduced in 2004. This system incorporates both short-track and tear-away capabilities. The external wire lock fits on the biopsy port, which enables the locking of one or two guidewires. A key feature of this system includes a side port that has been placed 6 cm from the distal tip of any catheter and a closed tear-away channel running the length of the catheter (as opposed to the open tear-away channel of the RX). The Fusion guidewire, although not extendable, is 0.035-inch in diameter and 185 cm in length with similar features to the Jagwire [7].
The V-system (Olympus, Tokyo, Japan) was introduced in 2005. This is the first modification of a duodenoscope for the facilitation of guidewire exchanges. The V-system scope elevator lever includes a V-shaped groove and an increased angle of articulation. This design promotes securing and locking of the short guidewire at the elevator level to reduce repositioning of the guidewire during accessory exchanges [8]. The V-system devices are like the traditional long-wire devices at the leading end but have a different design component at the external end [8]. Device manipulation may be simplified by the 270 cm long wire (Visiglide 1 or 2) with a hydrophilic coating over the leading end. The C-hook allows the device handle to be attached to the V-scope. This enables the endoscopist to control multiple accessories. The main advantage of the C-hook is that it is very easy for the endoscopist to relinquish control of the guidewire back to the assistant if needed.
Our experience shows the advantage of using internal locking (V-system) in most procedures, external locking (RX) is more advantageous when using the double-wire technique. At our workplace, we introduced a hybrid technique using a short wire and other accessories suitable for both short and long systems.
One of the main benefits of the short system is clearly associated with the ability to permit physician-controlled guidewire cannulation of the desired duct. The median time to successful cannulation was shown to be shorter in wire-assisted cannulation compared to cannulation achieved after the first contrast injection (120 s vs.150 s, P = 0.73) [9]. In another study where 71 patients were enrolled, the short-wire system provided a faster device exchange time (125 vs. 177 s, P = 0.05) and stent insertion time (135 vs. 254 s, P = 0.001) as compared to the long-wire system. A shorter total procedure time, fluoroscopy time and cannulation time was noted, but without statistical significance. PEP occurred in one patient in the short-wire and two patients in the long-wire group [10].
The changes in guidewire design and physician control of the wire can be expected to reduce ampullary trauma and lead to decreased complication rates, especially PEP. PEP is still the most frequent and severe complication encountered subsequent to ERCP with an incidence of 3.5%. PEP is mild, moderate and severe in 45%, 44% and 11% of cases, respectively. Death occurs in 3% of cases of PEP (95% CI 1.65–4.51%) [11,12].
No difference in the rates of PEP after cannulation was shown when using standard catheter 7.8% vs. hydrophilic Jagwire 0.035-inch guidewire 5.4% [13]. A major advantage of the short-wire system is the potential for shorter procedure and fluoroscopy time. Using the V-system endoscope and accessories with a short hydrophilic wire (Glidewire; Boston Scientific Corporation) can lead to rapid and reliable device exchanges with only a 5% chance of wire loss [14]. Use of the endoscopist-controlled rather than assistant-controlled wire guidance for bile duct cannulation reduces the complications of ERCP such as pancreatitis [14].
A prospective multicentre, randomised and controlled trial was conducted comparing the V-system to the traditional duodenoscope and accessories. The V-system was found to have both reduced rates of guidewire adjustments and time needed to complete accessory exchanges over a guidewire when compared to the traditional system [8]. The reduction in exchange time between the V-system and the conventional system was 19.4 s vs. 31.7 s (P < 0.001), whereas the need to reposition the guidewire was required less often with the V-system, 9.4% vs. 35.7% (P = 0.0005) [8]. By contrast, the reduced procedure and fluoroscopy times were not found to be statistically significant. Failure to secure the guidewire leading to loss of access occurred in 11% of cases. The reasons for loss of access varied from unfamiliarity with the system to nuances with the use of the guidewire and the elevator [8].
Preliminary data from a prospective randomised single-blind trial with 46 patients that compared the performance characteristics of the short-wire system (Fusion) and a standard long-wire system showed a trend towards shorter procedure times and shorter time to perform various ERCP manoeuvres with the short-wire system [15]. A statistically significant reduction in stent insertion times was also observed during this study (P = 0.001).
There are not many recent randomised studies comparing the long and short systems. One took place in 2016 in the USA [16]. The patients were randomised using a 2 × 2 factorial design to the initial cannulation attempt with endoscopist--controlled vs. assistant-controlled wire systems (1 : 1 ratio) and small (3.9 Fr tip) vs. standard (4.4 Fr tip) sphincterotomes (1 : 1 ratio). The primary efficacy outcome was successful deep bile duct cannulation within 8 attempts. A sample size of 498 was planned to demonstrate a significant increase in cannulation of 10%. Interim analysis was planned after 200 patients – with a stopping rule pre-defined for a significant difference in the composite safety end point (pancreatitis, cholangitis, bleeding and perforation).
The study was stopped after the interim analysis, with 216 patients randomised, due to a significant difference in the safety end point with endoscopist-controlled vs. assistant-controlled wire guidance [3/ 109 (2.8%) vs. 12/ 107 (11.2%), P = 0.016)], due primarily to a lower rate of PEP [3/ 109 (2.8%) vs. 10/ 107 (9.3%), P = 0.049)]. The difference in successful biliary cannulation for endoscopist-controlled vs. assistant-controlled wire guidance was − 0.5% (95% CI−12.0 to 11.1%) and for small vs. standard sphincterotome − 0.9% (95% CI–12.5 to 10.6%).
In addition to PEP, the most common complications are bleeding and cholangitis. In this field, comparative studies are needed to compare the short - and long--wire ERCPs. In general, postsphincterotomy bleeding has been reported in up to 2% of ERCP cases [17]. Transient bacteraemia has been reported in up to 27% of therapeutic procedures, cholangitis has been reported in 1% of the procedures [18]. In a large retrospective study of 16,855 patients undergoing ERCP, infection was reported in only 1.4% [19].
Single-used endoscopes are gradually entering clinical practice as a result of endoscope associated infections [20]. When using, for example a single-use duodenoscope EXALTTM Model D (Boston Scientific), it is also possible to use short-wire techniques due to the locking capabilities [21].
Although there are many benefits to the short-wire systems, there have been some inefficiencies associated with them. These include decreased pushability due to the open channel design (RX), inability to flush the channel to facilitate use with a hydrophilic wire (RX), occasional inability to use smaller than 0.035-inch or angled wires after the channel is torn with the first device exchange (unless the device is preloaded) (RX), deterioration of the device after multiple exchanges (RX, Fusion), not being able to insert pancreatic stents easily (all), occasionally no reliable locking of the wire (V), looping of the guidewire between the biopsy port and the external locking device (RX, Fusion), air and bile leakages [12].
Considering the advantages and disadvantages of both ERCP systems a hybrid technique was introduced at our workplace .
Conclusion
In clinical practice, two ERCP techniques are used, the long - and the short-wire systems. Both have their advantages and disadvantages. The short-wire system is used more often in other countries than in the Czech Republic. The short-wire system reduces the side effects of ERCP by reducing the cannulation and procedure times, fluoroscopy time and sedation requirements, as well as improving the wire stability and the physician’s control of the wire. The disadvantage of a different short-wire system include decreased pushability due to the open channel design, inability to flush the channel to facilitate use with a hydrophilic wire, inability in some cases to use smaller than 0.035-inch or angled guidewires repeatedly, deterioration of the device after multiple exchanges, no reliable locking of the wire, looping of the wire and air and bile leakages.
At our workplace, a hybrid technique combining the advantages of both systems was introduced and eliminated their disadvantages. It uses a short guidewire and any accessory designed for both short and long systems. The basis of the technique is internal locking of the wire by the V-system. Unlike some studies, we did not observe dislocation of the wire due to insufficient fixation on the Albarran bridge, even when using wires of different thicknesses. The advantage of this technique is traditional assistant cannulation, targeting the wire by an endoscopist and in the case of suitable accessories, a smooth transition to physician-assisted cannulation, confirmation of better control of the short wire by an assistant, faster deployment of accessories and an assumed lower complication rate. Our study aimed to describe practical experience with this technique and try to introduce it into routine clinical practice. Randomised control trials are of course necessary in future. Last year we organised a workshop on this topic (short-wire system and hybrid technique). The hybrid ERCP technique is very promising due to its combination of the advantages of both traditionally used systems, therefore we do not use long wires at all in our department.
Submitted/ Doručeno: 3. 5. 2021
Accepted/ Přijato: 2. 6. 2021
MUDr. Mgr. Jaroslav Maceček, Ph.D., MBA
Gastroenterology Department
AGEL Středomoravská nemocniční a.s. – AGEL Prostějov Hospital
Mathonova 291/ 1
796 04 Prostějov
Conflict of Interest: The authors declare that the article/ manuscript complies with ethical standards, patient anonymity has been respected, and they state that they have no financial, advisory or other commercial interests in relation to the subject matter.
Publication Ethics: This article/ manuscript has not been published or is currently being submitted for another review. The authors agree to publish their names and e-mails in the published article/ manuscript.
Dedication: The article/ manuscript is not supported by a grant nor has it been created with the support of any company.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Konflikt zájmů: Autoři deklarují, že text článku odpovídá etickým standardům, byla dodržena anonymita pacientů a prohlašuji, že v souvislosti s předmětem článku nemají finanční, poradenské ani jiné komerční zájmy.
Publikační etika: Příspěvek nebyl dosud publikován ani není v současnosti zaslán do jiného časopisu pro posouzení. Autoři souhlasí s uveřejněním svého jména a e-mailového kontaktu v publikovaném textu.
Dedikace: Článek není podpořen grantem ani nevznikl za podpory žádné společnosti.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Sources
1. Lee TH, Jung YK, Park SH. Preparation of high-risk patients and the choice of guidewire for a suc-cessful endoscopic retrograde cholangiopancreatography procedure. Clin Endosc 2014; 47(4): 334–340. doi: 10.5946/ ce.2014.47.4.334.
2. Kawakami H, Maguchi H, Mukai T et al. A multicenter, prospective, randomized study of selective bile duct cannulation performed by multiple endoscopists: the BIDMEN study. Gastrointest Endosc 2012; 75(2): 362–372. doi: 10.1016/ j.gie.2011.10.012.
3. Kwon C, Koh DH, Song TJ et al. Technical reports of endoscopic retrograde cholangiopancreatography guidewires on the basis of physical properties. Clin Endosc 2020; 53(1): 65–72. doi: 10.5946/ ce.2019.114.
4. Reddy SC, Draganov PV. ERCP wire systems: the long and the short of it. World J Gastroenterol 2009; 15(1): 55–60. doi: 10.3748/ wjg.15.55.
5. Somogyi L, Chuttani R, Croffie J et al. Guidewires for use in GI endoscopy. Gastrointest Endosc 2007; 65(4): 571–576. doi: 10.1016/ j.gie.2006.10.003.
6. Beilstein MC, Ahmad NA, Kochman ML et al. Initial evaluation of a duodenoscope modified to allow guidewire fixation during ERCP. Gastrointest Endosc 2004; 60(2): 284–287. doi: 10.1016/ s0016-5107(04)01686-4.
7. Shah RJ, Somogyi L, Petersen BT et al. Short-wire ERCP systems. Gastrointest Endosc 2007; 66(4): 650–657. doi: 10.1016/ j.gie.2007.05.030.
8. Joyce AM, Ahmad NA, Beilstein MC et al. Multicenter comparative trial of the V-scope system for therapeutic ERCP. Endoscopy 2006; 38(7): 713–716. doi: 10.1055/ s-2006-925446.
9. Bailey AA, Bourke MJ, Williams SJ et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy 2008; 40(4): 296–301. doi: 10.1055/ s-2007-995566.
10. Draganov PV, Kowalczyk L, Fazel A et al. Prospective randomized blinded comparison of a short-wire endoscopic retrograde cholangiopancreatography system with traditional long-wire devices. Dig Dis Sci 2010; 55(2): 510–515. doi: 10.1007/ s10620-009-1052-5.
11. Dumonceau JM, Andriulli A, Elmunzer BJ et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointetinal Endoscopy (ESGE) guideline. Endoscopy 2014; 46(9): 799–815. doi: 10.1055/ s-0034-1377875.
12. Andriulli A, Loperfido S, Napolitano G et al. Incidence rates of post-ERCP complications: a systemic survey of prospective studies. Am J Gaetroenterol 2007; 102(8): 1781–1788. doi: 10.1111/ j.1572-0241.2007.01279.x.
13. Katsinelos P, Paroutoglou G, Kountouras Jet al. A comparative study of standard ERCP catheter and hydrophilic guide wire in the selective cannulation of the common bile duct. Endoscopy 2008; 40(4): 302–307. doi: 10.1055/ s-2007-995483.
14. Papachristou GI, Baron TH, Gleeson F et al. Endoscopic retrograde cholangiopancreatography catheter and accessory exchange using a short hydrophilic guide wire: a prospective study. Endoscopy 2006; 38(11): 1133–1136. doi: 10.1055/ s-2006-944739.
15. Fazel A, Kowalczyk L, Moezardalan K et al. Preliminary results from prospective randomized single blinded trial comparing the performance characteristics of a short-wire (FUSION) and standard long-wire (DASH) ERCP device systems. Gastrointest Endosc 2006; 63(5): AB242. doi: 10.1016/ j.gie.2006.03.628.
16. Buxbaum J, Leonor P, Tung J et al. Randomized trial of endoscopist-controlled vs. assistant-controlled wire-guided dannulation of the bile duct. Am J Gastroenterol 2016; 111(12): 1841–1847. doi: 10.1038/ ajg.2016.268.
17. Szary MN, Al-Kawas FH. Complications of endoscopic retrograde cholangiopancreatography: how to avoid and manage them. Gastroenterol Hepatol (NY) 2013; 9(8): 496–504.
18. Kullman E, Borch K, Lindström E et al. Bacteremia following diagnostic and therapeutic ERCP. Gastrointest Endosc 1992; 38(4): 444–449. doi: 10.1016/ s0016-5107(92)70474-x.
19. Masci E, Toti G, Mariani A et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol 2001; 96(2): 417–423. doi: 10.1111/ j.1572-0241.2001.03594.x.
20. Rahman MR, Perisetti A, Coman E et al. Duodenoscope-associated infections: update on an emerging problem. Dig Dis Sci 2019; 64(6): 1409–1418. doi: 10.1007/ s10620-018-5431-7.
21. Urban O, Falt P. První použití single-use duodenoskopu v České republice. Gastroent Hepatol 2020; 74(5): 428–430. doi: 10.14735/amgh2020428.
Labels
Paediatric gastroenterology Gastroenterology and hepatology SurgeryArticle was published in
Gastroenterology and Hepatology
2021 Issue 3
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- The Importance of Limosilactobacillus reuteri in Administration to Diabetics with Gingivitis
-
All articles in this issue
- Editorial
- Kvíz z klinické praxe
- Current status of endoscopic full-thickness resection for treatment of colorectal neoplastic lesions
- Hybrid short-wire ERCP technique, five years of experience
- Severe bleeding as a complication of endoscopic choledocho-duodenal drainage using LAMS (Hot-Axios) in the treatment of distal stenosis of the common bile duct due to pancreatic head adenocarcinoma
- Endoscopic bariatric therapies
- Endoscopic and medical therapy of gastric antral vascular ectasia: case series and review of available methods
- Anal intraepithelial neoplasia and HD anoscopy
- A rare cause of dysphagia in adult
- Late tension pneumoperitoneum via the abdominal stoma after PEG-J
- Switch from original to biosimilar adalimumab SB-5 in patients with Crohn‘s disease – long-term results
- Teduglutide in the treatment of short bowel syndrome in Crohn’s disease
- Laparoscopic repair of congenital paraesophageal hernia in an 18-month-old child – a clinical case and literature review
- Telemedicine is more than a „doctor on the phone“
- Endoscopy and endotherapy in IBD, ISCARE 26.2.2021
- The selection from international journals
- Správná odpověď na předchozí kvíz Neklasifikovatelný idiopatický střevní zánět postihující tlusté střevo (IBD-unclassified)
- Erratum
- Kreditovaný autodidaktický test: digestivní endoskopie
- Gastroenterology and Hepatology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Anal intraepithelial neoplasia and HD anoscopy
- Endoscopic bariatric therapies
- Teduglutide in the treatment of short bowel syndrome in Crohn’s disease
- A rare cause of dysphagia in adult
