THE EFFECT OF FLUID ACCUMULATION IN STOMACH ON ELECTRICAL IMPEDANCE TOMOGRAPHY IMAGE OF LUNGS
Electrical impedance tomography (EIT) is a non-invasive, side effect free, bedside monitoring alternative to conventional imaging methods. One of the most frequent EIT system used for lung monitoring is PulmoVista 500 (Dräger Medical, Germany). The manufacturer of the system recommends placing the electrode belt at the level of 4th to 6th intercostal space. Since the fundus or cardia of the stomach is located in a position that contributes to the creation of EIT lung image, there is a question whether the EIT image is not influenced by the content of the stomach. The aim of this study is to investigate whether significantly different EIT images of the lungs can be obtained, if the monitoring is performed in subjects with different liquid content in the stomach. Eleven healthy subjects were monitored in this study at three phases: with empty stomach, after drinking 0.5 L and 1.0 L of water. Significant changes in the distribution of ventilation were found for regions of interest set as quadrants.
Keywords:
electrical impedance tomography, distribution of ventilation, stomach
Authors:
Kristyna Buzkova; Martin Skopek
Authors‘ workplace:
Czech Technical University in Prague, Kladno, Czech Republic
; Dep. of Biomedical Technology, Faculty of Biomedical Engineering
Published in:
Lékař a technika - Clinician and Technology No. 1, 2017, 47, 11-14
Category:
Original research
Overview
Electrical impedance tomography (EIT) is a non-invasive, side effect free, bedside monitoring alternative to conventional imaging methods. One of the most frequent EIT system used for lung monitoring is PulmoVista 500 (Dräger Medical, Germany). The manufacturer of the system recommends placing the electrode belt at the level of 4th to 6th intercostal space. Since the fundus or cardia of the stomach is located in a position that contributes to the creation of EIT lung image, there is a question whether the EIT image is not influenced by the content of the stomach. The aim of this study is to investigate whether significantly different EIT images of the lungs can be obtained, if the monitoring is performed in subjects with different liquid content in the stomach. Eleven healthy subjects were monitored in this study at three phases: with empty stomach, after drinking 0.5 L and 1.0 L of water. Significant changes in the distribution of ventilation were found for regions of interest set as quadrants.
Keywords:
electrical impedance tomography, distribution of ventilation, stomach
Introduction
Electrical impedance tomography (EIT) offers a noninvasive, side effect free, bedside alternative monitoring method to conventional imaging systems. EIT provides information about the distribution of tissue impedance within selected tomographic cross-section of the body. The principle of EIT is well known for more than 30 years [1] and its application has been found in several medical areas, especially in monitoring of lung ventilation where commercial systems are now available [2,3].
One of the most frequently used devices in clinical practice is EIT system PulmoVista 500 (Dräger Medical, Germany). For lung monitoring it uses an electrode belt with 16 integrated electrodes. It is recommended by the manufacturer to place the electrode belt at the level of 4th–6th intercostal space. This is also a localization of the fundus of stomach (Fig. 1 right). Since the human body is not a homogenous conductor, EIT lung image is affected by ambient tissue. The contribution of the impedance of tissue to total impedance of the thorax is given by the distance from the cross-section that is defined by the position of the electrode belt (as illustrated in Fig. 1). Therefore, the content of the stomach could affect the EIT image of the lungs, especially in patients that are monitored in horizontal position.
![Fig. 1: Left: Contribution of impedance with increasing distance from the cross-section defined by the position of the electrode belt. [4] Right: The illustration of the stomach position and the level of the fifth intercostal space. Modified from [5].](https://pl-master.mdcdn.cz/media/image/f30d9916587aa70773bc8d9c17fe0668.png?version=1537797620)
The aim of this study is to evaluate, whether there is a significant impact of a liquid content in the stomach on EIT image of the lungs. Another aim of this study is to contribute to the standardization of methodology of EIT monitoring of the lungs in a clinical practice.
Methods
This prospective interventional crossover study was approved by the Institutional Review Board of the Faculty of Biomedical Engineering, Czech Technical University in Prague in May, 2016. The study was conducted in a laboratory of CTU FBMI. Every participant signed an informed consent before enrolment in the study.
Inclusion and Exclusion Criteria
The subjects had to be minimally 2 hours after any meal or drinks. The subjects had to be overall healthy, without any active implanted devices and wounded skin in the electrode belt location. Also, according to the manufacturer, it is not possible to use EIT system in subjects that suffer from diseases that cause uncontrollable body movements or subjects with Body Mass Index (BMI) greater than 50 kg/m2. Another exclusion criterion for our study was Tiffeneau index lower than 70%, which is defined as a ratio of forced expired volume in one second and forced vital capacity. Healthy subjects, without any obstructive diseases of respiratory system, are supposed to have Tiffaneau index above 70%. It was possible for both smokers and non-smokers to be enrolled in the study.
Monitored Subjects
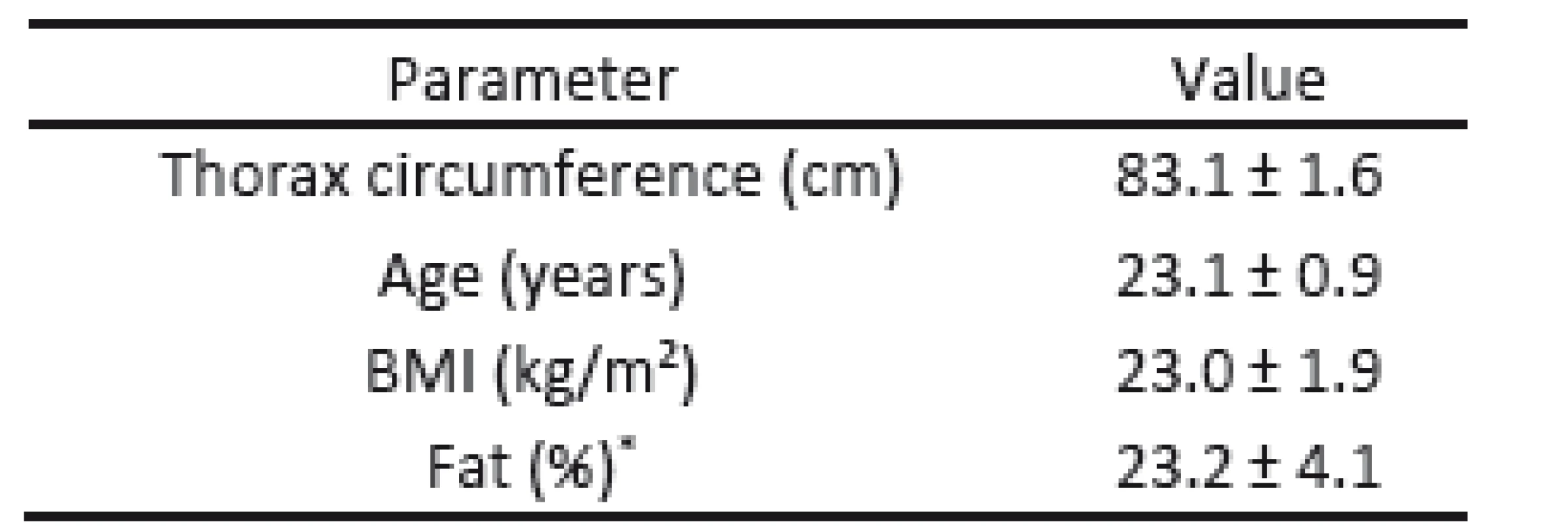
In total, 11 healthy volunteers (6 males, 5 females) were involved in the study. All subjects completed the study. Main characteristics of the subjects are presented in the Table 1.
Experiment Protocol
First, every subject was placed to supine position and the localization of the fifth intercostal space in the level of the medioclavicular line was performed. The respective place was labeled on the subject’s skin with a marker. Circumference was then measured in vertical body position with arms relaxed using a tailor’s measuring tape. The subject was asked to breathe normally, so the measuring did not occur during a deep inspiration or expiration. Based on the measured circumference of the thorax, proper size of the electrode belt was selected.
Subject’s height and weight was then measured and BMI was calculated. Subject’s body fat was measured using two different methods: impedance and caliper. The impedance method for body fat measuring was performed using Omron BF 511 (Kyoto, Japan). The second method is in fact a measurement of a skinfold and was performed using a Harpenden Skinfold caliper (Baty International, Great Britain). In our case four different places were measured with the caliper: biceps, triceps, abdomen and beneath scapula. The body fat measurements were fully in accordance with the procedures described in the manufacturer’s manual. These characteristics were measured for later use for evaluation of possible anatomy correlation with the EIT results.
Every subject then underwent a spirometric examination. Regular examination was performed using spirometer Ergostik (Geratherm Medical, Germany). Forced expired volume in one second, forced vital lung capacity and Tiffaneau index were measured.
Finally, an electrode belt of a proper size was placed on the subject’s chest at the level of the fifth intercostal space. The subject was set into a horizontal position. A reference electrode was placed on the abdomen and connected to the electrode belt. For this purpose, a single-use ECG electrode was used.
When the subject was placed to the monitoring position, the belt was connected to the EIT system and the electrode signal quality was checked and displayed on the screen. When the signal was not sufficient, ECG gel was applied between the affected electrode and skin until a proper contact resistance was assured. Then, the subject started to breathe through the spirometric sensor. When the delay of the tube was found and the subject remained calm with a breathing pattern stabilized, a four-minute period of EIT recording started. The subject was supposed not to move, since an extra movement could cause artifacts in the recorded data. After the four-minute period of the calm breathing, the subject was asked to perform deep breaths for approximately one minute. The subjects were covered with blanket in order to ensure the subject’s comfort and to minimalize muscle tremors.
When the first measuring was finished, the subject removed the spirometric probe and sit up. With the belt remaining on, the subject drank 0.5 L of water within the time limit of two minutes. Then the signal quality was checked and another set of measurement was performed. This process was repeated once more, so the third measurement was performed after drinking another 0.5 L of water, increasing the total intake of liquids to 1 L.
Data Evaluation
A cross-section image of the thorax that was acquired from the PulmoVista 500 EIT system was divided into four regions of interest (ROI). Divisions into four horizontal layers and quadrants, as shown in Fig. 2, are the most common and represent the standard definition of ROIs in the PulmoVista 500 software. Percentage of regional ventilation in each ROI for each breath was evaluated. For every record of spontaneous and forced breathing, one mean value representing the percentage of ventilation in each ROI was calculated.
![Fig. 2: Regions of interest (ROI) used for the evaluation of distribution of ventilation. Upper image: Layers; Lower image: Quadrants. [6]](https://pl-master.mdcdn.cz/media/image/dd7fe565b15911dc9e3b8d2f55d09d46.png?version=1537797235)
Then, distribution of ventilation for all three records acquired in every subject was compared for each ROI.
As a post-hoc analysis, student’s t-test for paired samples was used for comparison of the statistical significance of the differences between the evaluated regional ventilations in the ROIs. Since there are three groups being compared, Bonferroni correction was calculated. For the level of significance α = 0.05, obtained p values were adjusted by number of groups, i.e. 3.
Changes in distribution of ventilation for records with different liquid volumes in the stomach were evaluated. A value of p < 0.05 was considered to be statistically significant in this study.
Results
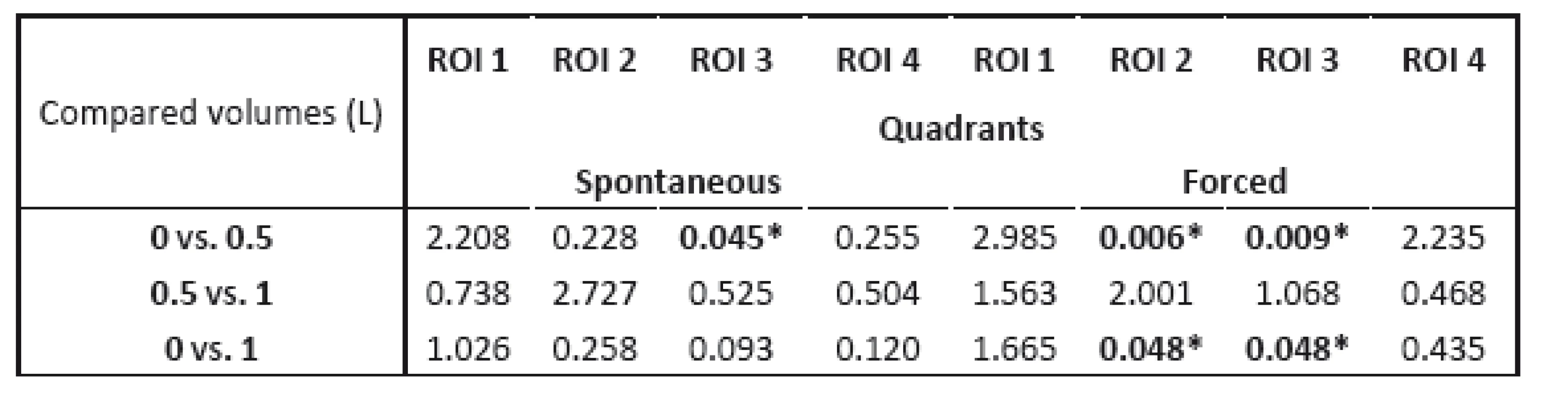
All p-values presenting statistical significance of changes of distribution of ventilation are shown in Table 2. There were no statistically significant changes for the layers layout. The most significant changes were found in quadrants layout for the change of liquid in stomach from 0 to 0.5 L at ROI 2 and ROI 3 for the phase of forced breathing. Figure 3 shows changes in distribution of ventilation in ROI 3 for quadrants layout for both spontaneous and forced breathing.

No significant changes in tidal volumes were detected during the measurements for spontaneous breathing, nor for the forced breathing.
No anatomy correlations with changes in distribution of ventilation were found.
Discussion
Detected changes in distribution of ventilation suggest that when monitoring the patient in a horizontal position by EIT, obtained images of lungs can be affected by the amount of liquid in the stomach.
For layers, no significant changes were detected after Bonferroni correction of evaluated p values.
The most significant changes were detected for the quadrants layout. This can be explained by the position of the stomach, which is situated underneath the basal part of left lung and is projected mainly into 2nd and 4th quadrant.
No changes were detected when comparing the images of 0.5 L and 1 L volumes. We can speculate that the change of the volume from 0.5 L to 1 L was not crucial enough to cause significant changes in the impedance of the thorax. Also, as the subject was measured with an empty stomach, the liquid was being absorbed during the measurement. We tried to minimize the absorption of the liquid from the stomach by very small pauses between the measurements; there was only a two-minute pause for the subject to drink a halfliter of water and these pauses were strictly kept.
It is hard to analyze whether the found changes in distribution of ventilation directly correspond with the liquid changes in stomach, since there was no localization of stomach performed for each subject. The assumed localization of the stomach was based on general human anatomy [Fig. 1 right], so the exact position of stomach can vary between individuals. Therefore, changes in the liquid volume in stomach can cause different changes in EIT image of the thorax from subject to subject. Also, the stomach does not need to be exactly in the chosen tomographic cross-section, since the EIT image is influenced by more distant tissues, as shown in Fig. 1 left.
Another factor that needs to be taken into account in this study is the position of the subjects during EIT monitoring. The subjects were in horizontal position, when stomach is placed more dorsally then in vertical position, which is caused by the gravitation. The horizontal position was chosen since EIT monitoring is usually performed in laying patients.
It was allowed to enroll the subject in the study only if he/she was at least two hours after last meal or drink, what al of them confirmed at the beginning. The stomach content of 300 mL should be absorbed in approx. an hour [7]. By the two-hour pause, we assured that previous content in the stomach should not play a substantial role in our study. However, there was no possibility to check the initial condition of the subject, thus we had to rely on the subject’s honesty.
Conclusion
The study proves that different stomach content can have an impact on the evaluated lung image, when repeatedly using the electrical impedance tomography system PulmoVista 500 for monitoring of distribution of ventilation. It shows that it is necessary to perform the monitoring at exact same conditions and patient’s fluid intake must be registered. Otherwise, inaccurate conclusions regarding the patient’s long-term development of a lung disease or conditions might be derived.
Acknowledgement
The work has been supported by research grant No. SGS16/258/OHK4/3T/17.
Ing. Kristýna Buzková
Department of Biomedical Technology
Faculty of Biomedical Engineering
Czech Technical University in Prague
nám. Sítná 3105,
CZ-272 01 Kladno
E-mail: buzkokri@fbmi.cvut.cz
Phone: +420 728 848 785
Sources
[1] Brown, B. H.: Electrical impedance tomography (EIT): a review. Journal of Medical Engineering & Technology, vol. 27/ 3, pp. 97–108, 2003.
[2] Holder, D.: Electrical impedance tomography: methods, history, and applications. Philadelphia: Institute of Physics Pub., 2005.
[3] Leonhardt, S., Lachmann, B.: Electrical impedance tomography: the holy grail of ventilation and perfusion monitoring? Intensive Care Medicine, vol. 38, issue 12, pp. 1917–1929, 2012.
[4] Teschner, E., Imhoff, M.: Electrical impedance tomography: The realization of regional lung monitoring. Dräger Medical GmbH EIT Booklet, Germany, 2011.
[5] Dylevsky, I.: Funkční anatomie, Grada Publishing a.s., 2009, I. vydání.
[6] Masopustova, M.: Effect of tomographic plane on results of electrical impedance tomography (Vliv tomografické roviny na výsledky vyšetření EIT u mužů a žen). Diploma thesis, Faculty of Biomedical Engineering, Czech Technical University in Prague. 2014.
[7] Peronnet, F., Mignault, D., Du Souich, P., Vergne, S., Le Bellego, L., Jimenez, L. and Rebasa-Lhoret, R.: Pharmacokinetic analysis of absorption, distribution and disappearance of ingested water labeled with D2O in humans. European Journal of Applied Physiology, 112(6), 2213–2222, 2012.
Labels
BiomedicineArticle was published in
The Clinician and Technology Journal

2017 Issue 1
-
All articles in this issue
- THE EFFECT OF FLUID ACCUMULATION IN STOMACH ON ELECTRICAL IMPEDANCE TOMOGRAPHY IMAGE OF LUNGS
- EFFECT OF STERILIZATION ON MECHANICAL PROPERTIES OF COLLAGEN-BASED COMPOSITE TUBES
- BIOFEEDBACK AS A NEUROBIOMECHANICAL ASPECT OF POSTURAL FUNCTION
- THE USE OF NONINVASIVE DIAGNOSTIC METHODS IN THE ASSESSMENT OF POSTURAL CHANGES IN UNIVERSITY STUDENTS
- USING PVDF FILMS AS FLEXIBLE PIEZOELECTRIC GENERATORS FOR BIOMECHANICAL ENERGY HARVESTING
- The Clinician and Technology Journal
- Journal archive
- Current issue
- About the journal
Most read in this issue
- THE USE OF NONINVASIVE DIAGNOSTIC METHODS IN THE ASSESSMENT OF POSTURAL CHANGES IN UNIVERSITY STUDENTS
- BIOFEEDBACK AS A NEUROBIOMECHANICAL ASPECT OF POSTURAL FUNCTION
- USING PVDF FILMS AS FLEXIBLE PIEZOELECTRIC GENERATORS FOR BIOMECHANICAL ENERGY HARVESTING
- THE EFFECT OF FLUID ACCUMULATION IN STOMACH ON ELECTRICAL IMPEDANCE TOMOGRAPHY IMAGE OF LUNGS
