-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
MutilATing electrotrauma – case REPORT
Autoři: Y. Kaloudová; H. Řihová; P. Brychta; I. Suchánek; J. Kučera; I. Menšík; H. Krupicová; B. Lipový
Působiště autorů: Department of Burns and Reconstruction Surgery, University Hospital, Brno, Czech Republic
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 50, 1, 2008, pp. 11-15
INTRODUCTION
The passage of aĘhigh-voltage electrical current through aĘhuman body causes depolarization of the cell membranes with aĘwide variety of possible consequences that can even lead to the destruction of these cells. At the same time electric energy is transformed to thermal energy in the tissues involved, mainly in high resistance tissues (1). Progression of the necrosis is characteristic of electrotrauma (1). To maintain vitality of the peripheral parts of extremities it is very important to prevent compartment syndrome. This can be achieved by repeated very careful examination, evaluation of the status and earliest possible completion of releasing cuts of the skin and into subcutis after aĘcircular deep burn; however, first of all come fasciotomies of all muscle groups in the impaired extremity. After electric current passes through the extremities, subescharotic and subfascial oedema develops (1). The most important task is to release deep paraosseal muscle groups. Fasciotomy must be completed within 6Đ8 hours after the injury at the latest (1, 2). When high-voltage electrical current passes through the extremity, often skin and subcutis appear intact; however, muscle structures are damaged. Electrotrauma leads to pathological changes due to the thermal effect and also to the developing oedema of tissues. The oedema quickly increases during the first eight hours after the injury and then gradually increases until 24 hours after the injury (1). Fasciotomy allows the release of overpressure in particular muscle groups, and blood supply in the extremity improves (1, 2).
In the Czech Republic the main electric grid has a voltage of 230 V, 22 kV, 110 kV, 220 kV, 400 kV.
On the electrified railway lines the voltage between the trolley and the rail is 3000 VĘ(direct current in the northern part of the Czech Republic) or 25 kV (alternating current in southern Czech Republic).
Between the trolley of a Prague tram and the rail the voltage is 600 V, the same as between the wires for trolleybus. Between the rail and current collecting rail (“third rail”) in the metro the voltage is 750 V(4).
CASE REPORT
May 5th, 2005, Lipnice nad Sázavou. Assembling work on the high-voltage overhead line tower (22 kV). The current in the wires is turned off, and a fitter works tied to the line tower with safety belts.
At 01 : 30 PM the current in the line is revived and the 22-year-old man is hit by an electrical discharge. Unconsciousness, tonic clonic convulsions. After the electrical current is turned off the stricken man is untied from the belts and transported to the ground by the elevating platform. On arrival of an ambulance the man ventilates spontaneously, is conscious, has retrograde amnesia, heart beat is regular, pulse is 110 beats per minute, blood pressure is 150/70.
Primary, adequate transfer by Air Ambulance to our Department of Burns and Reconstruction Surgery in Brno, admission at 02.50 PM.
- Petechiae in face and in the lumbar area, small injuries to the tongue.
- Flexion contracture of the left upper extremity in the elbow joint, full fixated extension in the left radiocarpal joint.
- Deep burns in the left axilla, deep circular burns on arm and forearm left, noncircular burns of fingers and palm of the left hand.
- Flexion position in the radiocarpal joint of the right upper extremity, fingers in full flexion, deep burns of the right palm and fingers, oedema of the right wrist and distal part of the forearm.
- Right foot in equinovarus position, circular deep burns of distal half of the right shank and foot.
- Total extent of the deep burned areas was 10% of the body surface. Clear clinical and laboratory signs of passage of the electrical current through the patient are present.
Preliminary examination at the surgery in general anesthesia – immediately after admission
Left upper extremity:
- Escharotomy axilla Đ arm Đ forearm Đ hand.
- Fasciotomy on arm, forearm and flexor retinaculotomy (already apparent necroses of biceps brachii muscle, brachioradialis, triceps brachii tenton, necrosis of olecranon and head of radius, necrosis of the proximal portions of extensors at the forearm).
- Elbow contracture release as well as the radiocarpal joint.
- Excision of the necrotic skin and subcutis in the left cubita and at the dorsal part of forearm.
Right upper extremity:
- Escharotomy of the forearm, wrist and hand.
- Fasciotomy of the anterior muscle group and deep muscle groups of the forearm.
- Flexor retinaculotomy (right median nerve necrotic).
Right lower extremity:
- Escharotomy shank - foot.
- Fasciotomy on shank (apparent are necroses of anterior and deep muscle groups of the shank).
Course of treatment
(Fig. 1-12)
Obr. 1. Documentation of burn wounds care of the patient 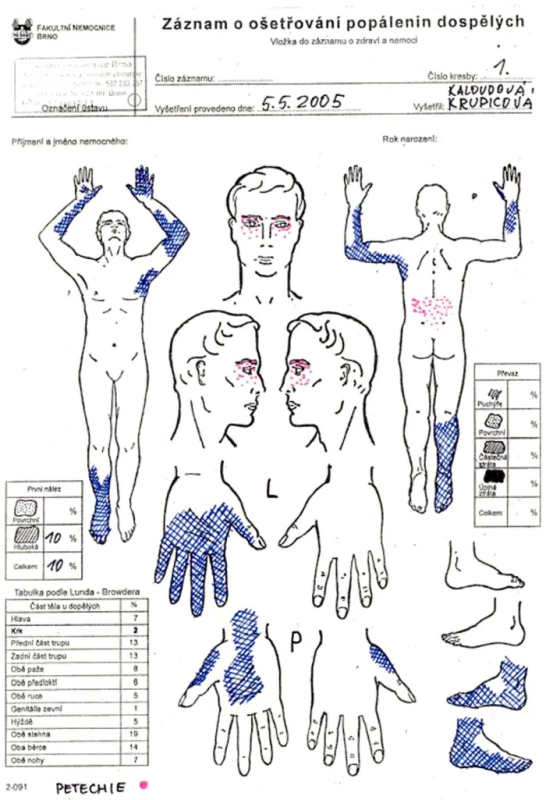
Obr. 2. Right upper extremity second day after the injury 
Obr. 3. Right shank sixth day after the injury 
Obr. 4. Left upper extremity eighth day after the injury 
Obr. 5. Left upper extremity eighth day after the injury 
Obr. 6. Left arm stump 12th day after the injury – revision in general anesthesia 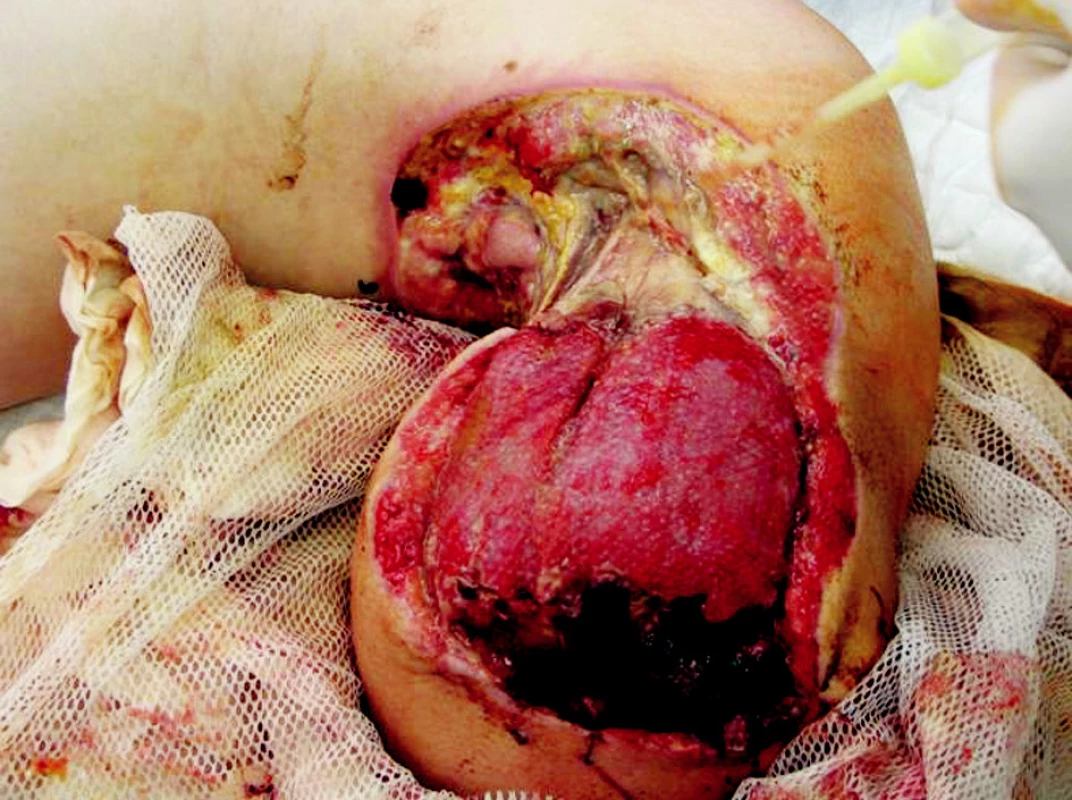
Obr. 7. Exarticulation of the left upper extremity in shoulder 
Obr. 8. Stump of the right shank 18th day after the injury 
Obr. 9. Right upper extremity 22nd day after the injury 
Obr. 10. Right upper extremity 30th day after the injury 
Obr. 11. Microsurgically transferred parascapular fasciocutaneous flap to the soft tissues defect of right upper extremity 
Obr. 12. The patient 3 months after the high-voltage electric current injury 
Second day after the injury – revision in general anesthesia
- Massive oedema in subcutis and subfascia on upper extremities and on the right lower extremity.
- Excision of clearly bordered necrosis of the skin and subcutis in right forearm and right hand completed.
- Fasciotomy extended to thorax - release of pectoralis major muscle.
Sixth day after the injury
- Amputation of the right lower extremity in shank (ischemic necrosis of the distal third of shank and foot). Stumps of fibula and tibia covered by a dorsal muscle flap from the intact calf muscles.
Eighth day after the injury
- Amputationof the left upper extremity below the shoulder (necrotic colliquating muscle groups distally on arm and forearm, necrotic ulna and radius in proximal two thirds and necrosis of the humerus in distal one third). The humeral stump covered by vital muscle remainders of arm and the adaptation suture for rotation of laterodorsal skin and subcutaneous flaps.
Fourteenth day after the injury
- Exarticulation of left upper extremity in the shoulder (humerus completely necrotic, progression of necrosis to the humeral stump muscles). Vital part of deltoid muscle was rotated into the defect after exarticulation, adaptation suture of deltoid muscle fascia and latissimus dorsi, defect covered by rotation of the dorsolateral fasciocutaneous flap from the arm.
Eighteenth day after the injury
- Autografting of the stump apex of the right shank with split-thickness grafts.
Twenty-eighth to thirty-eighth day after the injury
- Repeated dressing changes at the intensive care unit (analgesia and deep sedation), gentle debridement.
Forty-fifth day after the injury
- Excision of the bordered necrosis of the right median nerve.
- Microsurgery transfer of the right parascapular fasciocutaneous flap to the distal part of the right forearm, wrist and thenar for the soft tissues defect closure.
- Surgery was completed by microsurgery team of our workplace.
Two and half months after the injury
- Patient discharged home.
- Outpatient care, physical and psychological rehabilitation followed.
Four months after the injury
- Reconstruction of the right median nerve in the area of distal forearm and wrist Đ nerve graft from the left suralis nerve, length 12 cm.
One and a half years after the injury
- Reconstruction of the right thumb long flexor tendon with aĘtendon graft from the left foot.
Two years after the injury
- Function of the right hand in terms of grip is satisfactory (he was able to complete pinch grip and sign). Gait on the right prosthesis was very good.
DISCUSSION
Direct measurement of the pressure in the intracompartment space is not possible in extensive burns due to open wounds, either from burns or wounds after fasciotomy. Intrafascial pressure can be validly measured only after removal of dressings which cover extensive wounds - in our case this could have been achieved only in the operating room. Moreover, in the intensive care this practice would in many cases be in conflict with the hygienic/epidemiology regime. Therefore every half an hour for the first eight hours after the injury experienced burn specialists completed a palpation examination of the muscle groups - even over the dressings (1). It is recommended that the examination is performed by one experienced person who palpates the increasing tension of muscle groups. If the finding is positive, immediate revision of the patient’s wounds in the operating room is necessary, and usually further fasciotomies at the impaired extremity must be completed. We have to be aware that often the compartment syndrome develops in deep periosseal muscle groups and deep nerve and blood vessel bundles frequently under intact skin and subcutis. Weakened pulsation of arteries at the periphery of extremities is a late symptom of already irreversible damage to the deep structures.
Releasing escharotomies of the skin and subcutis and fasciotomies at the impaired extremities that show signs of passage of the high voltage electric current (areas of contacts, i.e. exits or entrances of the electric current) must be completed in the full length of the extremity and tied together in the axilla to the fascias of chest muscles (1).
Adequate treatment of the burn shock obviously helps the blood circulation in extremities and helps to maintain as many structures as possible vital.
CONCLUSION
To maximize the vitality of tissues at the extremities the authors stress the importance of earliest fasciotomies of the impaired extremities. After the passage of a high-voltage electrical current through an extremity it is necessary to release all muscle groups, especially the paraosseal, eight hours after the injury at the very latest. Evaluation of the clinical status in the first 24 hours after the injury should be assigned to the most experienced burn specialist available.
Address for correspondence:
Yvona Kaloudová, M.D.
Burn Centre, University Hospital Brno
Jihlavská 20
625 00 Brno
Czech Republic
E-mail: ykaloudova@fnbrno.cz
Zdroje
1. Königová R.,et al. Komplexní léčba popálenin. Praha: Grada, 1999, p.325-356.
2. Klein,L., Ferko A., et al. Principy válečné chirurgie. Praha: Grada, 2005, p.63-65, 97-111.
3. Burke JF., Boyd RJ., Mc Cabe CJ. Trauma Management. Chicago: Year Book Medical Publishers, 1988, p.208-226.
4. Source: ČEZ (searched out 2007. 11. 27,
http://www.cez.cz/edee/content/microsites/elektrina/4-4.htm)
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek ČESKÉ A SLOVENSKÉ SOUHRNYČlánek HOW EAST DISCOVERED WEST
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2008 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
- Metamizol v terapii akutních bolestí hlavy
-
Všetky články tohto čísla
- MutilATing electrotrauma – case REPORT
- Award of the G. Whitaker International Burns Prize for 2007
- Specific aspects of the treatment of patients with multiple mechanical and burn injuries
- Catheter-Related Infections in Burn Patients at the Burn Centre of the University Hospital in Ostrava
- G. WHITAKER INTERNATIONAL BURNS PRIZE – PALERMO (Italy)
- Acinetobacter – serious danger FOR burn patients
- THE 25TH ANNIVERSARY OF BRNO BURN CENTRE: WHAT HAS CHANGED AND WHAT HAS NOT
- THE EFFECT OF NIFEDIPINE ON THE PATENCY OF MICROVASCULAR ANASTOMOSIS IN RATS
- Report of the 12th Congress of European Burns Association (EBA), Budapest, Hungary, September 12–15, 2007
- ČESKÉ A SLOVENSKÉ SOUHRNY
- HOW EAST DISCOVERED WEST
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Specific aspects of the treatment of patients with multiple mechanical and burn injuries
- Acinetobacter – serious danger FOR burn patients
- THE EFFECT OF NIFEDIPINE ON THE PATENCY OF MICROVASCULAR ANASTOMOSIS IN RATS
- MutilATing electrotrauma – case REPORT
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



