-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Specific aspects of the treatment of patients with multiple mechanical and burn injuries
Autoři: L. Klein 1; P. Douša 2; R. Zajíček 1; I. Pafčuga 1; M. Tokarik 1
Působiště autorů: Dept. of Burns Medicine, 2 Dept. of Orthopedics and Traumatology, 3rd Faculty of Medicine and Teaching Hospital Královské Vinohrady, Charles University, Prague, Czech Republic 1
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 50, 1, 2008, pp. 17-22
Introduction
Polytrauma presents a serious medical and social problem, due to the morbidity, mortality and possible consequences in terms of a long-term disablement or permanent invalidity. There are many various definitions of these statuses whereas all with the common basic characteristics of polytrauma: simultaneous injury to several (at least two) body systems, one of which threatens the patient’s life. In some cases, polytrauma can be considered also combined or associated thermal injuries (burns) and mechanical injuries (for example fractures of the locomotor system). Combinations of these injuries are among the most severe ones. The overall condition of the patient depends on how severe are the particular injuries. The initial burn shock deepens and course of the acute burn treatment period worsens, complications often occur, treatment time of particular injuries extends. If there is a fracture of pelvis or femur hemorrhagic shock develops among the burn shock and the blood loss must be replaced even in the initial stages (in contrast to when there is burn injury only). A complex approach to the treatment of such patients is possible only within the scope of an interdisciplinary cooperation of particular specializations that are organized into trauma centers.
Case report
On August 1st, 2006 at one o’clock in the morning a car accident occurred. A car crashed into a tree and caught fire. There were two passengers in the car, one died in the fire and the other, 23-year-old male was rescued with severe thermal and mechanical injuries. The patient was urgently treated on the spot, including endotracheal intubation and he was transported by an air ambulance directly to the Burn Centre, where he was admitted at 02.30 AM. Later, we have found from the anamnesis that the injured man was previously healthy and he did not suffer any internal illnesses. In his early childhood he underwent a surgery for pes equinovarus on the right and at the age of 4 he underwent bilateral prolongation of his Achilles tendons. The initial treatment revealed that the patient sustained deep burns of upper limbs, trunk, buttocks, genitals and lower limbs in the total extent of 62% of the total body surface area (TBSA) (Fig. 1, 2). An inhalation trauma of the airways was suspected. In the area of the right orbit there was a hematoma and there was laceration of the patient’s lower lip. Since there was disfiguration, mechanical damage to the skin on the ventrolateral side of the thigh and the whole lower extremity was positioned in an external rotation, we suspected a compound fracture in the area of right femur. Venous and arterial cannulations were completed, aggressive liquid resuscitation was continued with the use of crystalloid and colloid solutions, and frozen plasma was also given. A nasogastric tube was placed as well as insertion of a permanent Foley catheter was performed, mechanical lung ventilation was continued, and the patient was put on antibiotics Tazocin. We have completed releasing escharotomy on the right hand and forearm, suture of the lip wound and tetanus prophylaxis by application of intramuscular TAT 0.5ml. Next, it was necessary to complete diagnostics of possible skeletal injuries and exclude possible injuries to the thoracic and abdominal cavities. The appropriate X-ray and CT scans were completed. X-ray of the right femur revealed ipsilateral fracture of the proximal end without a significant dislocation and transversal dislocated fracture of the diaphysis. Other bones were without any trauma. Head, chest and abdominal injuries were excluded; on the contrary, bronchoscopy confirmed inhalation injury of the airways. CT scan of the chest revealed aĘpartial atelectasis of the lower lobe on the right side and subsegmental atelectasis in the left lower lobe. Consequently, the orthopedic team completes the first surgery - fixation of the right femur diaphysis fracture with the use of external fixator (ZF Mefisto) which allowed correcting the fracture into a satisfactory position (Fig. 3). Due to the overall condition of the patient and due to the type of multiple traumas we have decided to treat the pertrochanteric fracture conservatively. Next, the treatment continued on the Intensive Care Unit and was focused on mechanical ventilation, liquid resuscitation, metabolic support and surgical treatment of the burned areas. Surgical interventions then followed, usually in 48-hour-intervals, consisting of releasing incisions (Fig. 4) or necrectomies. On the upper extremities and on trunk the avulsion method was used. It concerns the so called epifascial necrectomy, where we remove skin and subcutis down to fascia (Fig. 5). The advantage of this method is significantly lesser blood loss than in the tangential (laminar) necrectomy by excisions when using Humby - or Watson - knife. Overview of the main surgical interventions is listed in Table 1.
Obr. 1. General view of the patient on admission 
Obr. 2. General view of the patient on admission 
Obr. 3. Status after the femoral fracture reposition by an external fixator in the burned area 
Obr. 4. Releasing incision on chest 
Obr. 5. Epifascial necrectomy – avulsion on right lower extremity 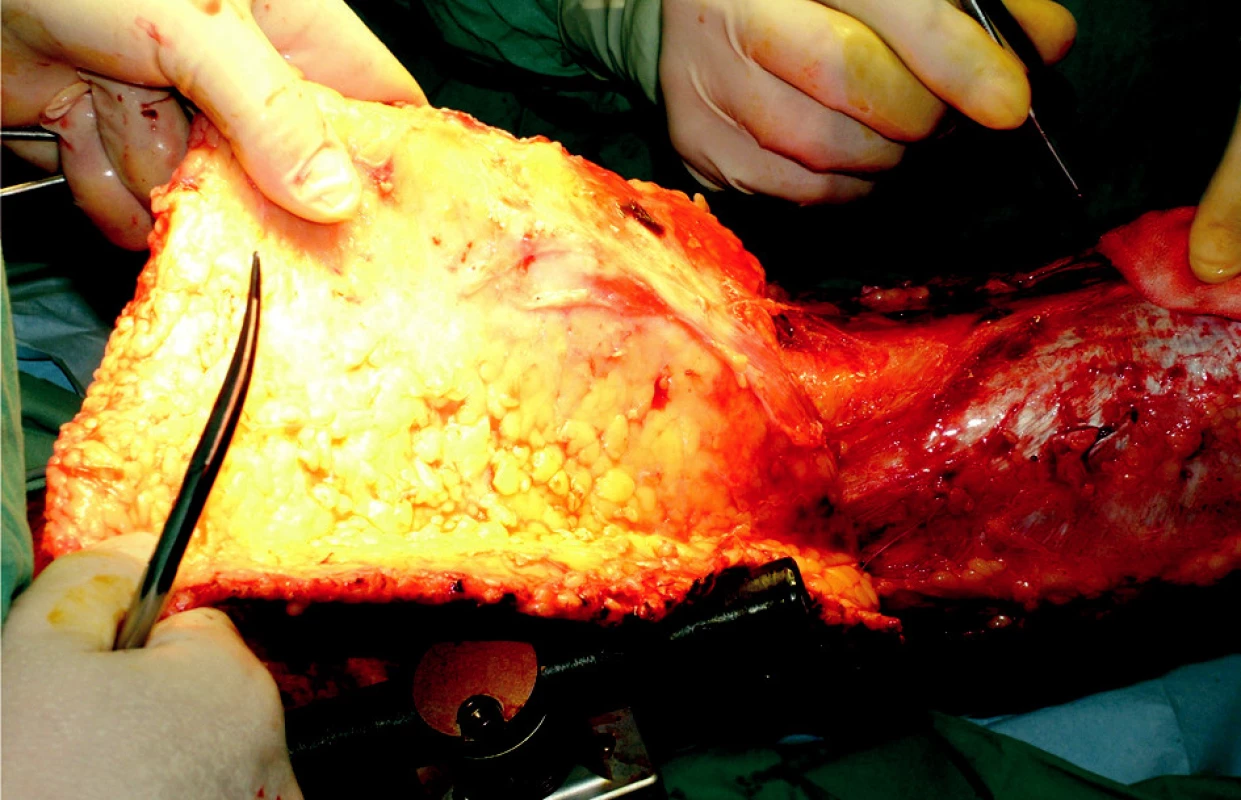
Tab. 1. Treatment options of fractures in combination with burns 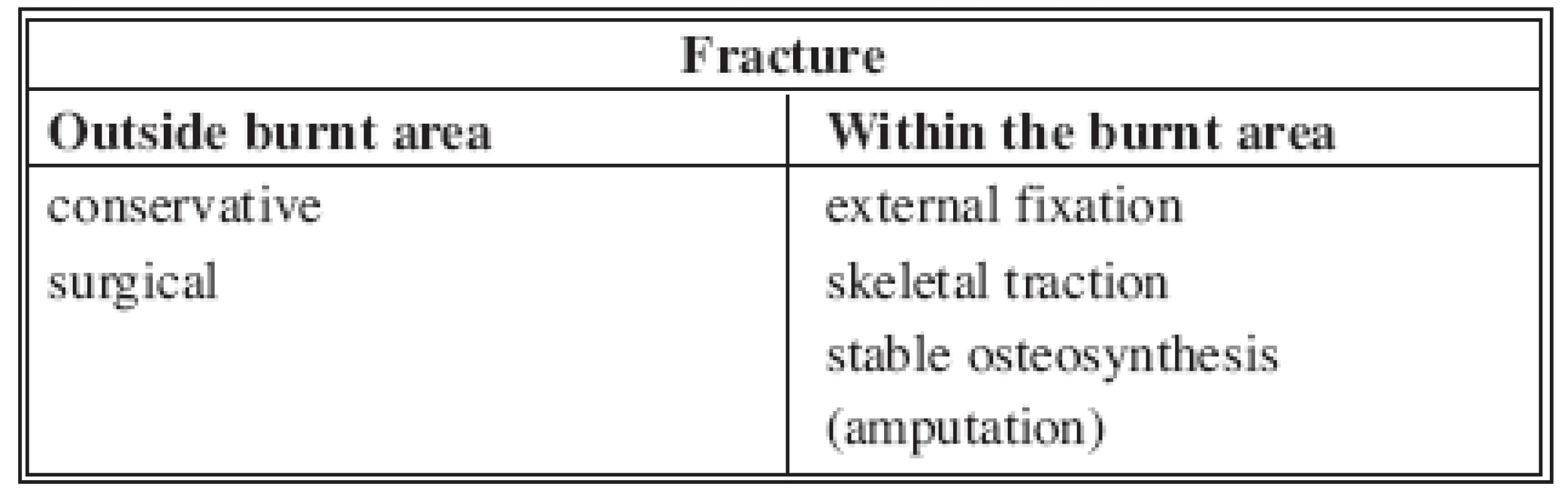
Despite the maximum effort to be gentle during manipulation with the patient (transfers to and from the operating table, surgery on limb with the external fixator in situ, bed changes etc.) the eighth day after the osteosynthesis, there was loosening of the fixator and it was necessary to reposition and fixate the femoral bone fragments again (Fig. 6). The fracture was healing with a massive callus particularly at the medial side of femur, however, the pertrochanteric fracture gradually led to a varosity of the proximal femoral fragment.Due to angulated fragments of the diaphysis it was necessary on November 16th, 2006 (14 weeks after the injury) to complete an adjustment of the external fixation. We have increased rigidity of the external fixator by adding more screws. We have achieved satisfactory position; the pertrochanteric fracture was at that time already healed. During the course of the treatment the patient underwent intensive physiotherapy, initially passive and later active with the goal to prevent contractures of the small and large joints and to limit muscle atrophy as much as possible and simultaneously maintain muscle strength. Later rebandaging including showering was performed at the standard unit. Owing to the then epidemiological situation at the workplace bacteriological assessment of wounds several times revealed a positive Methycilin-Resistant Staphylococcus aureus (MRSA). Despite that, through thorough local care and the overall treatment we managed to prevent infection in the areas of pin sites (Fig. 7-10). Since the patient had a significant psychological support from the staff, clinical psychologist, and a good family support, healing course of both types of injuries (thermal and mechanical) was positive. After five months from completion of the osteosynthesis we have dynamized the external fixator and the patient was allowed partial weight bearing on the limb. The patient started verticalization and gait training and gradually progressed to a full weight bearing. The patient’s overall condition at the end of the sixth month allowed for transfer to a surgical unit in the area of the patient’s residence so he could continue with rehabilitation. Transplanted and harvested areas as well as both fractures continued to heal well and on March 8th, 2007, eight months after the injury, during an out-patient visit it was possible to remove the external fixator (Fig. 11). The pertrochanteric femoral fracture healed in varus angulation, however, in this case we consider the position satisfactory. Fracture of diaphysis healed with a massive callus with a slight angulation. The result was shortening of the limb by 2 cm which proved to be positive due to the plantar flexion in the ankle joint. The patient thrives physically and mentally and is motivated to continue with gait training and overall self care training (Fig. 12).
Obr. 6. X-rays of the right femur prior to and after insertion of an external fixator 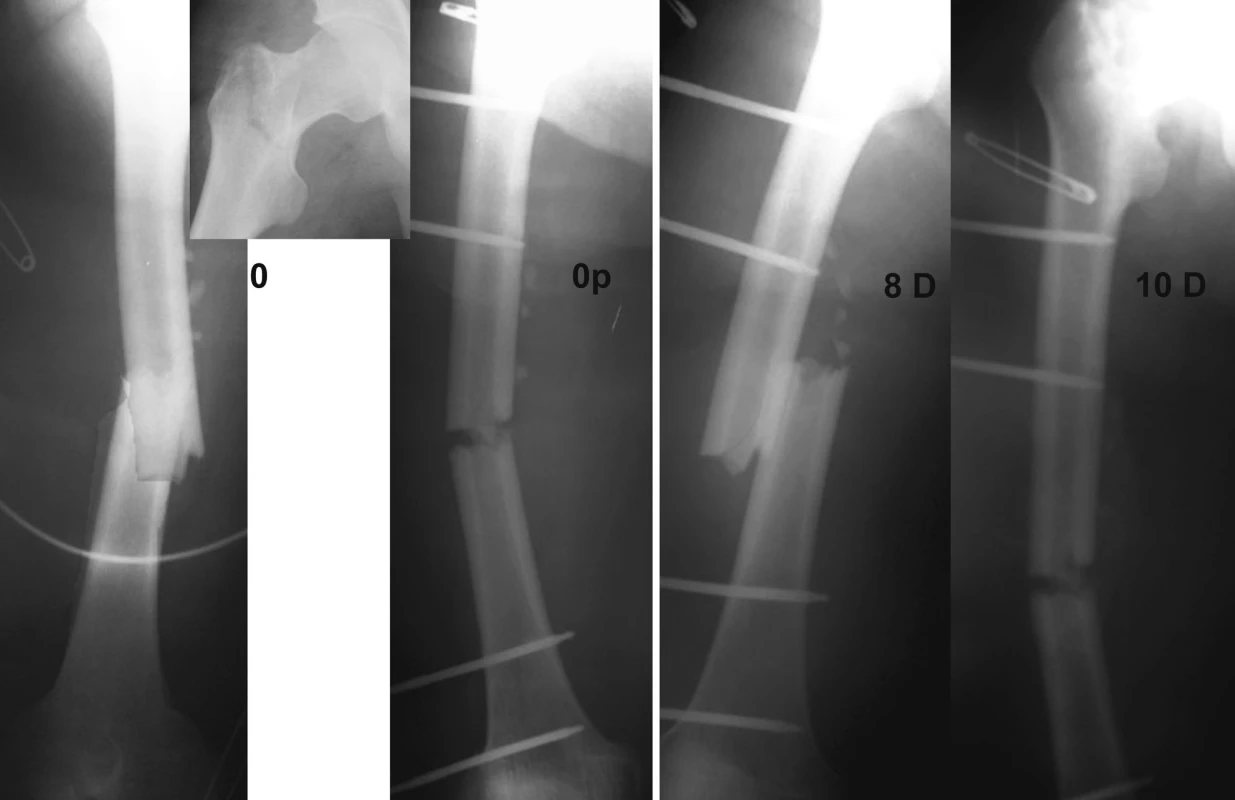
Obr. 7. Area of trunk and right lower extremity prepared for autotransplantation (on the right lower crus the first grafts already healed) 
Obr. 8. Freshly meshed grafts within the rate of 1:3 placed on trunk 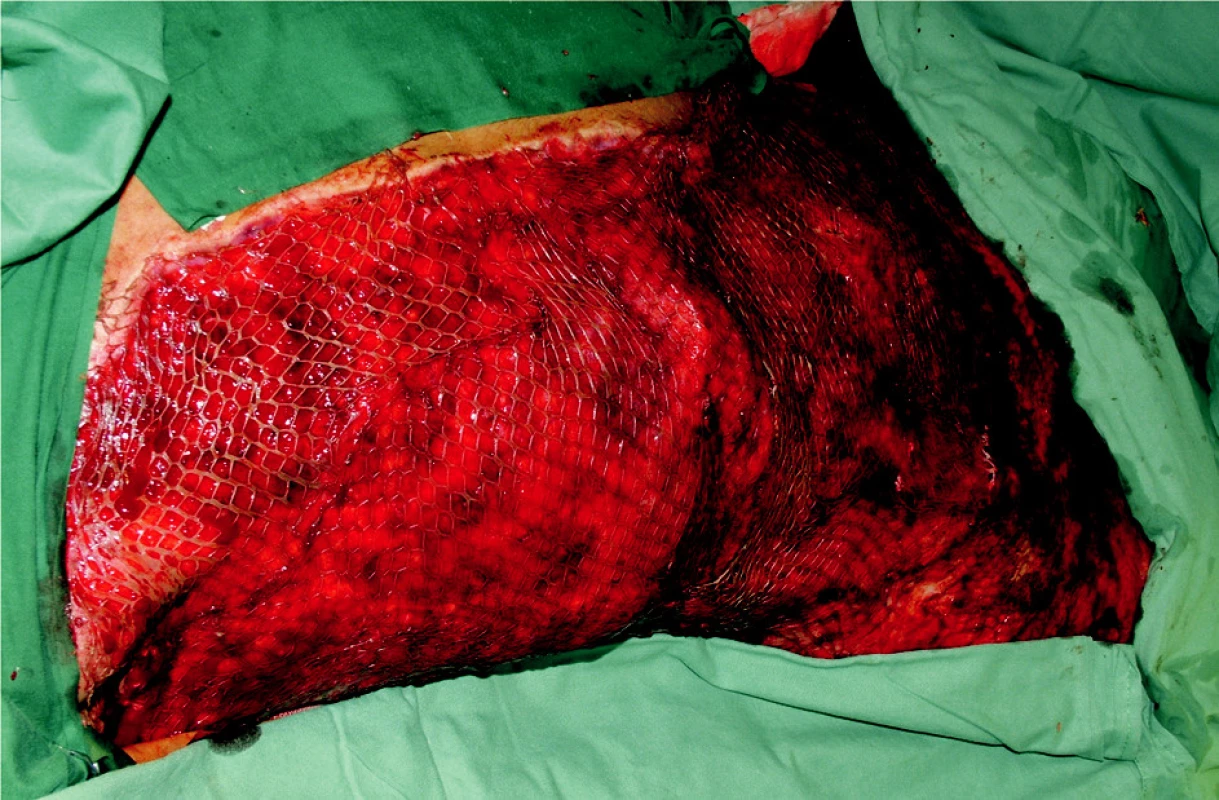
Obr. 9. Healed transplanted areas on trunk and right lower extremity, transplanted and harvest areas on the right upper extremity 
Obr. 10. Healed transplanted areas on trunk and right lower extremity, transplanted and harvest areas on the right upper extremity 
Obr. 11. Control X-ray of right femur 1.5, 3, 6 and 8 months after the injury 
Obr. 12. Status at outpatient check-up in April 2007 
Discussion
The combination of thermal and mechanical injuries can be divided into two types: one when the fracture is localized elsewhere than the burned area or within the burned area. This situation represents a critical factor which must be taken into account during the choice of possible treatment procedures. Basic possibilities of therapeutic algorithms are shown in Table 2.
Tab. 2. Abstract of main surgical interventions 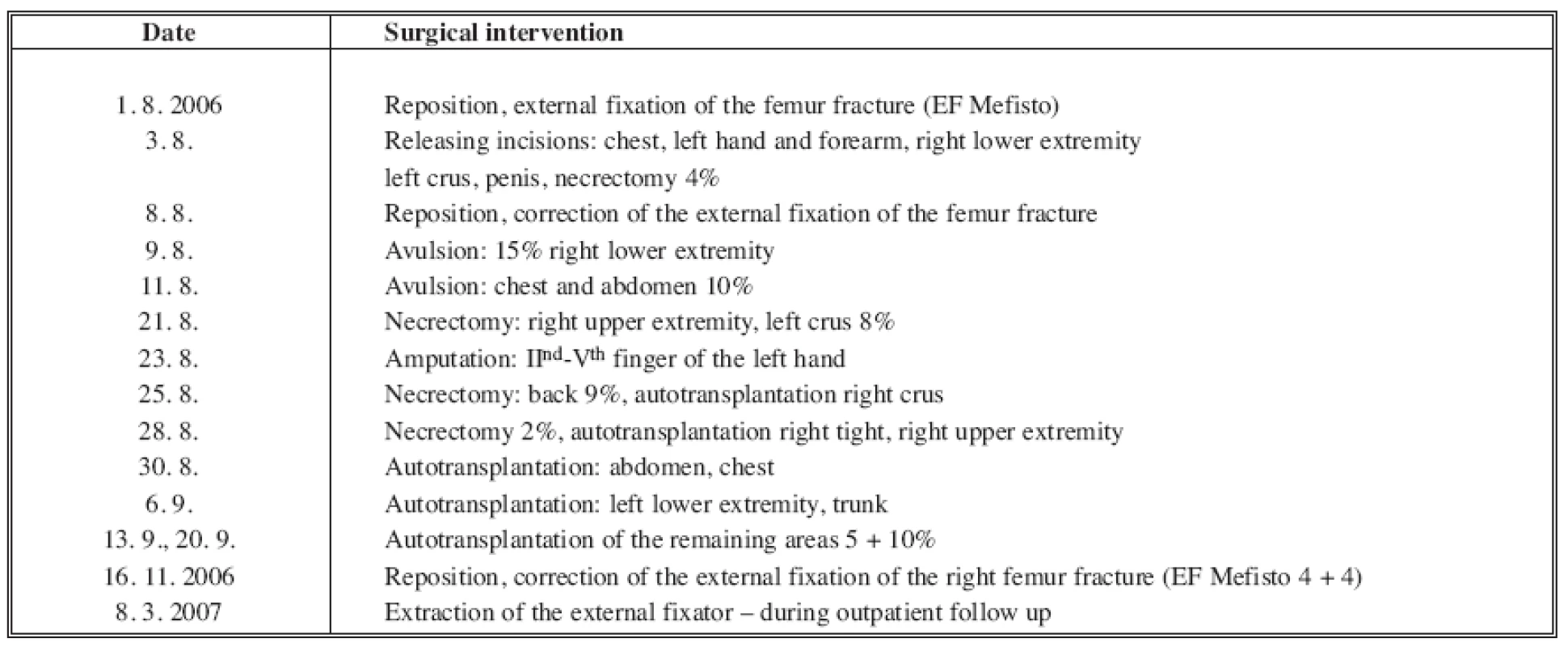
A majority of short bones fractures, vertebral and skull fractures are treated conservatively, which allows to fully concentrate on the treatment of burns. Complications are caused by circular burns, when the patients must be turned. Most frequently the combination of fractures and burns occur on upper or lower extremities. Fractures without dislocation of fragments can only be treated with a classical plaster cast if it is outside the burned area. Some workplaces may prefer the open-method treatment of the burn when using skeletal traction. However, the method of skeletal traction can not provide a perfect immobilization of the fractured fragments because there is a need for frequent rebandaging of the burned area. Metal material used for traction should not run through the burned area, because sooner or later it leads to an infection and loosening of the wire. The same reasons lead to certain reservations regarding the use of external fixators. Despite that, some authors recommend external fixators in open fractures or in an area with severe burns. When the skin is healed it is possible to change the external fixator to internal osteosynthesis. The most convenient treatment of fracture in the area of burn is a stable osteosynthesis that allows for a good manipulation with the extremity. However, due to severe burns in the area of thigh we have not in this case used the internal femoral fracture osteosynthesis with a reconstruction nail, which we use in cases of solely mechanical injuries. Osteosynthesis after dislocated fractures should be completed as soon as the patient’s status allows. Preferably, it should be completed within 48 hours after the injury, because later than that danger of infection in the burned area increases and there is aĘrisk of infection transmission from skin into the bone.
Opinions on surgical treatment of fracture through the burned area vary.
- In burns of 2nd degree where the incision runs through the burned area it is possible to sew the incision after osteosynthesis and treat the burn as usual.
- Experimental works on dogs in Houston tried the possibility to perform the osteosynthesis 24 hours after the necrectomy and covering of the area with autotransplants. However, the use of this method in human medicine is not further mentioned by authors.
- In comminuted fractures it is recommended to complete the necrectomy, bloody reposition with rinsing of the fracture site with antibiotics and subsequent suture of soft tissues and closure of the defect with autotransplants or temporarily with a biological cover (allotransplants, xenotransplants).
- Some workplaces recommend proceeding radically with the use of early two-team surgery method. Within two days after the injury, or preferably even the same day of admission after the patient is prepared, a team of two surgeons erudite in the treatment of burns complete a necrectomy according to the judged depth of necrosis and with the evaluation of transplants type. Concurrently, they harvest dermoepidermal autotransplants, which they expand by the use of meshdermatom. After that the trauma surgeon completes aĘstable osteosynthesis. Final closure of the wound is again completed by the team specialized in the treatment of burns. The subsequent treatment plan follows as usual.
- In particularly severe comminuted fractures with derangement of the blood supply and damage to the soft tissues it is necessary to consider an amputation as a lifesaving treatment. Particularly, if the fracture is associated with a critical extent of the burn when there is danger of sepsis or in patients who would not cooperate in the treatment of combined injury due to other illnesses, in elderly patients or after a mass accident in exceptional situations. It is recommended to complete an exarticulation in the most distal joint rather than amputation through the burned area and bone due to the possibility of infection transmission.
Conclusion
Many traits associated with the combined thermal and mechanical injuries, particularly the treatment course, treatment method, and prognosis of the status require an individual approach to particular patients based on evaluation of factors, which describe seriousness of the burn trauma. Based on our experience we move towards more active and early surgical solution of these complicated traumatic statuses. Particularly, considering that despite not a very high absolute number of the total injuries (up to 5% of thermal and mechanical injuries) these injuries concern mainly young individuals in a productive age and who can be this way saved and returned back to active life.
Acknowledgments
This work was completed within the scope of the research project supported by the grant IGA MZ NR 8853-4/06.
Address for correspondence:
Ass. Prof. Leo Klein, M.D., PhD.
Department of Burn Medicine
Šrobárova 50
100 34 Prague 10
Czech Republic
E-mail: klein@fnkv.cz
Zdroje
1. Alonso,J., Geissler,W., Hughes,JL. External fixation of femoral fractures. Indications and limitations. Clin. Orthop. Relat. Res., 241, 1989, p. 83-88.
2. Dossett,AB., Hunt,JL., Purdue,GF., et al. Early orthopedic intervention in burn patients with major fractures. J. Trauma, 31, 1991, p. 888-892.
3. Douša P., Bartoníček J., Havránek P.,Ipsilaterální zlomeniny proximálního konce a diafýzy femuru. Úraz. Chir., 13, 2005, p. 72-80.
4. Drábková, J. Polytrauma v intenzívní medicíně. Praha, Grada Publishing a.s., 2002, p. 307.
5. Charousková,M., Klein,L., Hofmann A.,Naše zkušenosti s léčbou zlomenin v popáleném terénu. Voj. Zdrav. Listy, 52, 1983, p. 196-199.
6. Königová R., et al. Komplexní léčba popálenin. Praha, Grada Publishing a.s., 1999, p. 455.
7. Purdue GF, Hunt JL. Multiple trauma and the burn patient. Am. J. Surg., 158, 1989, p. 536-539.
8. Santaniello JM., Luchette FA., Esposito TJ., et al. Ten year experience of burn, trauma, and combined burn/trauma injuries comparing outcomes. J. Trauma, 57, 2004, p. 696-701.
9. Scalea, TM., Boswell, SA., Scott, JD., et al. External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J. Trauma, 48, 2000, p. 613-621.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek ČESKÉ A SLOVENSKÉ SOUHRNYČlánek HOW EAST DISCOVERED WEST
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2008 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
- Možnosti využití metamizolu v léčbě akutních primárních bolestí hlavy
-
Všetky články tohto čísla
- MutilATing electrotrauma – case REPORT
- Award of the G. Whitaker International Burns Prize for 2007
- Specific aspects of the treatment of patients with multiple mechanical and burn injuries
- Catheter-Related Infections in Burn Patients at the Burn Centre of the University Hospital in Ostrava
- G. WHITAKER INTERNATIONAL BURNS PRIZE – PALERMO (Italy)
- Acinetobacter – serious danger FOR burn patients
- THE 25TH ANNIVERSARY OF BRNO BURN CENTRE: WHAT HAS CHANGED AND WHAT HAS NOT
- THE EFFECT OF NIFEDIPINE ON THE PATENCY OF MICROVASCULAR ANASTOMOSIS IN RATS
- Report of the 12th Congress of European Burns Association (EBA), Budapest, Hungary, September 12–15, 2007
- ČESKÉ A SLOVENSKÉ SOUHRNY
- HOW EAST DISCOVERED WEST
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Specific aspects of the treatment of patients with multiple mechanical and burn injuries
- Acinetobacter – serious danger FOR burn patients
- THE EFFECT OF NIFEDIPINE ON THE PATENCY OF MICROVASCULAR ANASTOMOSIS IN RATS
- MutilATing electrotrauma – case REPORT
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



