-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Spontaneous vaginal extrusion of the distal catheter of a ventriculoperitoneal shunt
Spontánní vaginální extruze distálního katetru ventrikuloperitoneálního zkratu
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors: F. Sahinturk; E. Sonmez; N. Altinors
Authors place of work: Department of Neurosurgery, Baskent University School of Medicine, Ankara, Turkey
Published in the journal: Cesk Slov Neurol N 2020; 83(2): 207-208
Category: Dopis redakci
Summary
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Dear editorial office,
A 34-year-old female had undergone a ventriculoperitoneal (VP) shunt operation due to hydrocephalus at another centre 10 years ago. The VP shunt had been revised three times and the last time it was adjusted to 100 mm H2O at the same centre. After 7 years, the patient complained of ataxia, dizziness and vision field defects. She was brought to our hospital`s emergency ward on December 28, 2016. Cranial MRI and diffusion MRI revealed bilateral cerebellar infarcts. She was drowsy and was unable to walk. The previous shunt had been placed through the right posterior parietal burr hole and it was not functional. An external ventricular drainage (EVD) was inserted through the right frontal burr hole, antiplatelet (acetylsalicylic acid 100 mg) and anticoagulant (enoxaparin sodium) medication was started. A new shunt was placed on January 6, 2017 via the same right frontal burr hole and it was adjusted to 140 mm H2O. The old non-functioning shunt was kept. She made a rapid neurological recovery. She was hospitalized at our clinic in January 2018 because of vaginal protrusion of the peritoneal part of the catheter. No CSF was noted at the tip of the catheter. Abdominal CT (Fig. 1) showed rupture and migration of the distal catheter. Examinations were made by the gynaecologist and general surgeon. She was scheduled for revision. The catheter spontaneously extruded as one piece during defecation. There was no sign of infection. A repeated gynaecological examination was performed and no further intervention was recommended. The extruded catheter was a part of the old shunt and for that reason, she was discharged in a good neurological and physical condition.
Fig. 1. Coronel abdominal CT.
Obr. 1. Koronální abdominální CT.
Fig. 2. Sagittal abdominal CT.
Obr. 2. Sagitální abdominální CT.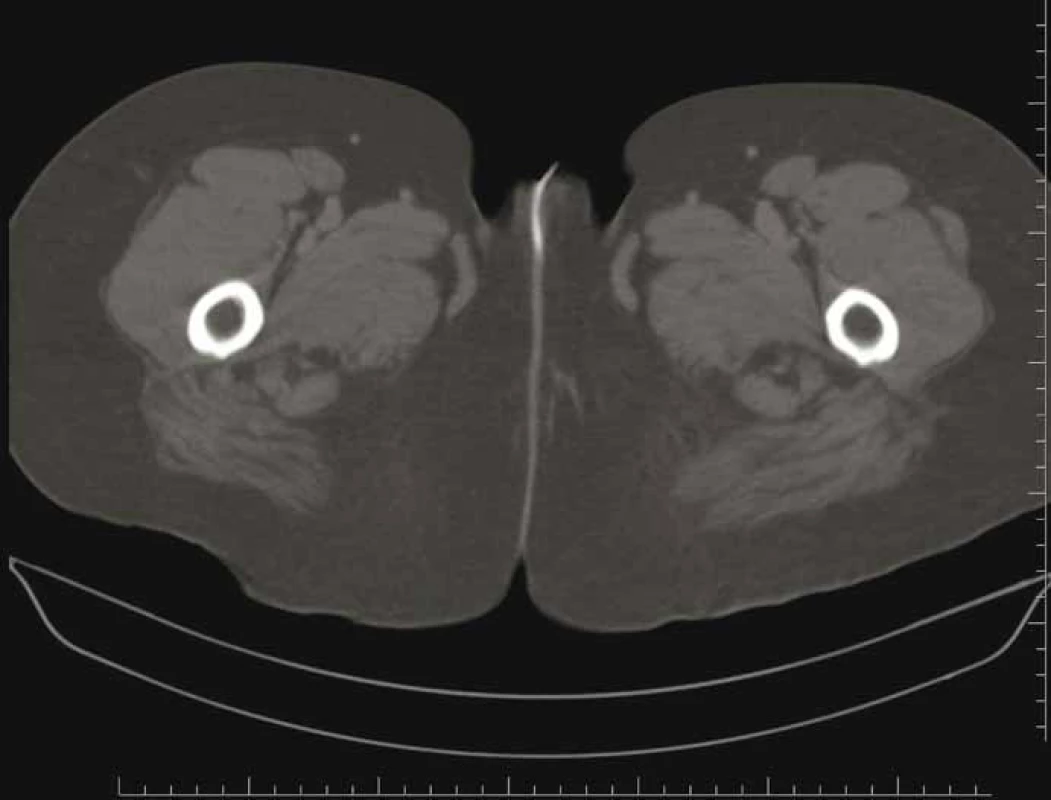
Disconnection and migration of a distal VP shunt catheter to a variety of unfavourable sites were noted in the literature. The perforation of the viscera in some instances may lead to more serious complications. Migration into the heart [1], gastric perforation and protrusion into the oral cavity [2], protrusion through the anus [3], bladder perforation [4], scrotal perforation [5] and different abdominal complications [6] are among them.
The vaginal protrusion of a distal shunt catheter is extremely rare. To date, only eight such cases have been reported in the literature (Tab. 1). Six patients were children under 2 years of age and the other two patients were adults.
Tab. 1. Clinical summary of the patients with vaginal protrusion of distal shunt catheter reported in the literature
Author
Patient age
Medical history
Therapy
Patel 1973
11 months
meningocele repair & VA shunt, VP shunt 7 months after infection positive
total shunt removal, a new shunt inserted later
Mozingo 1974
47 years
previous tentorial meningioma surgery & VA shunt, surgery for recurrent meningioma VP shunt no infection
distal catheter removal, new peritoneal catheter placed
Nagulic 1996
49 days
VP shunt, no infection
removal of the abdominal part of the catheter and replaced by a new one
Farrokhi 2007
16 months
myelomeningocele repair and VP shunt when 4 months old, shunt infection, antibiotic therapy and EVD followed by new VP shunt
therapy for vaginal catheter protrusion is not described
Altas 2012
14 months
VP shunt when newborn, shunt revision when 1 year old
shunt removed, EVD for 1 week, new shunt inserted
Teegala 2012
6 months
VP shunt for Dandy-Walker malformation, infection positive
total removal of the shunt, EVD placement
Bonfield 2015
45 years
Behçet's syndrome, VP shunt for pseudo-tumor cerebri, complete shunt revision for infection total abdominal hysterectomy for endometriosis, no infection
total removal of the shunt, a new VPL shunt inserted a week later, small opening in the vagina sutured
Lotfinia 2017
2 years
VP shunt, shunt revision, no infection
peritoneal catheter removed, replaced by a new peritoneal catheter
EVD – external ventricular drain; VA – ventriculoatrial; VP – ventriculoperitoneal
Bonfield et al [7] discussed their patient and another adult case reported by Mozingo and Cauthen [8] and found some similarities. Both patients had history of hysterectomy, extrusion was through the vaginal cuff and extrusions appeared after a relatively short time following the shunt placement. The case presented by Bonfield was diagnosed Behçet’s disease. The authors claimed that prior hysterectomy and mucosal dysfunction could increase the risk in this particular patient. The exact mechanism of vaginal perforation may not be completely understood with such limited experience, but it seems that previous shunt revisions, abdominal and gynaecological intervention, an overly long distal catheter (especially in children) and infection may play a role in vaginal shunt extrusions.
Zhou et al [9] described fibrosis formation around the tube resulting in adhesion of the shunt to the nearby viscera. It is believed that fibrosis immobilizes the tube and creates risks to the abdominal organs.
Speculation that the physical characteristics of the distal shunt catheter cause perforation of the abdominal viscera has not been regarded as a probable factor.
The therapeutic approach in these cases should include defining the point of rupture of the catheter, removing it safely, repairing the opening in the vaginal wall if necessary, treatment of infection if there is any and the insertion of a new shunt in a timely manner. A temporary EVD may be inserted in shunt dependent patients until a new shunt has been placed. Only the distal catheter is removed in the absence of infection and replaced by a new one. In other instances, the whole shunt may be removed and a new one inserted. The connection of a new peritoneal catheter may be made through a small abdominal incision once the point of disconnection is clearly defined by radiology. Laparoscopic and endoscopic approaches were used and suggested for the treatment of abdominal shunt catheter complications in general.
The treatment should be multidisciplinary including the cooperation of the radiology, general surgery, gynaecology and neurosurgery departments.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Fikret Şahintürk, MD
Department of Neurosurgery
School of Medicine
Baskent University
Fevzi Cakmak Caddesi 10. Sokak
No: 45 Bahcelievler
Ankara
Turkey
e-mail: fikretsahinturk@gmail.comAccepted for review: 18. 7. 2019
Accepted for print: 29. 1. 2020
Zdroje
1. Fewel ME, Garton HJ. Migration of distal ventriculoperitoneal shunt catheter into the heart. Case report and review of the literature. J Neurosurg 2004; 100 (2 Suppl Pediatrics): 206–211. doi: 10.3171/ped.2004.100.2.0206.
2. Yilmaz MB, Egemen E, Tonge M et al. Transoral protrusion of a peritoneal catheter due to gastric perforation 10 years after a ventriculoperitoneal shunting: case report and review of the literature. Turk Neurosurg 2013; 23 (2): 285–288. doi: 10.5137/1019-5149.JTN.4904-11.1.
3. Adeloye A. Protrusion of ventriculo peritoneal shunt through the anus: report of two cases. East Afr Med J 1997; 74 (5): 337–339.
4. Ueda Y, Kakino S, Hashimoto O et al. Perforation of the bladder by a peritoneal catheter: an unusual late complication of ventriculo-peritoneal shunt. No Shinkei Geka 1998; 26 (5): 413–416.
5. Rehm A, Bannister CM, Victoratos G. Scrotal perforation by a ventriculoperitoneal shunt. Br J Neurosurg 1997; 11 (5): 443–444. doi: 10.1080/02688699745970.
6. Odebode TO. Jejunal perforation and peroral extrusion of a peritoneal shunt catheter. Br J Neurosurg 2007; 21 (2): 235–236. doi: 10.1080/02688690701264346.
7. Bonfield CM, Weiner GM, Bradley MS et al. Vaginal extrusion of a ventriculo-peritoneal shunt catheter in an adult. J Neurosci Rural Pract 2015; 6 (1): 97–99. doi: 10.4103/0976-3147.143212.
8. Mozingo JR, Cauthen JC. Vaginal perforation by a Raimondi peritoneal catheter in an adult. Surg Neurol 1974; 2 (3): 195–196.
9. Zhou F, Chen G, Zhang J. Bowel perforation secondary to ventriculoperitoneal shunt: case report and clinical analysis. J Int Med Res 2007; 35 (6): 926–929. doi: 10.1177/147323000703500624.
Štítky
Detská neurológia Neurochirurgia Neurológia
Článek Poměr fosforylovaného tau proteinu k beta amyloidu v likvoru predikuje pozitivitu amyloidové PETČlánek Chirurgická léčba benigních neurogenních tumorů mediastina – analýza 7letého souboru pacientůČlánek Dopis redakciČlánek Komentář redakceČlánek Prof. Mraček oslavil 90 letČlánek Odešla MUDr. Olga Baudyšová
Článok vyšiel v časopiseČeská a slovenská neurologie a neurochirurgie
Najčítanejšie tento týždeň
2020 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Neuromultivit v terapii neuropatií, neuritid a neuralgií u dospělých pacientů
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
-
Všetky články tohto čísla
- Cévní morfologie, symptomy, diagnostika a léčba ischemických příhod mozkového kmene
- Je koncept vaskulární demence trvale udržitelný?
- Je koncept vaskulární demence trvale udržitelný? NE
- Je koncept vaskulární demence trvale udržitelný? Komenář
- Mezinárodní klasifikace bolestí hlavy (ICHD-3) – oficiální český překlad
- Schwannóm extrakraniálnej časti trojklanného nervu
- Chirurgická léčba mozkových metastáz
- Cavum septi pellucidi, cavum vergae a cavum veli interpositi
- Poměr fosforylovaného tau proteinu k beta amyloidu v likvoru predikuje pozitivitu amyloidové PET
- Provocative factors and treatment response in juvenile myoclonic epilepsy – experience from a tertiary epilepsy center
- Chirurgická léčba benigních neurogenních tumorů mediastina – analýza 7letého souboru pacientů
- Transkraniální sonografie mediotemporálního laloku u pacientů s Alzheimerovou demencí
- Endarterektomie zevní karotické tepny
- Vestibulární funkce u pacientů s kochleárním implantátem
- Cystická hydatidóza mozečku – vzácná kazuistika
- A case of late brachial plexopathy after chemotherapy and radiotherapy
- Spontaneous vaginal extrusion of the distal catheter of a ventriculoperitoneal shunt
- Opakovaná trombektómia u pacienta so zriedkavou kombináciou etiologických faktorov
- Dopis redakci
- Komentář redakce
- Prof. Mraček oslavil 90 let
- Odešla MUDr. Olga Baudyšová
- K jubileu profesorky Soni Nevšímalové
- Česká a slovenská neurologie a neurochirurgie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Cavum septi pellucidi, cavum vergae a cavum veli interpositi
- Cévní morfologie, symptomy, diagnostika a léčba ischemických příhod mozkového kmene
- Mezinárodní klasifikace bolestí hlavy (ICHD-3) – oficiální český překlad
- Chirurgická léčba mozkových metastáz
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



