-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Cholinesterase Inhibitors and Hospitalization for Bradycardia: A Population-Based Study
Background:
Cholinesterase inhibitors are commonly used to treat dementia. These drugs enhance the effects of acetylcholine, and reports suggest they may precipitate bradycardia in some patients. We aimed to examine the association between use of cholinesterase inhibitors and hospitalization for bradycardia.Methods and Findings:
We examined the health care records of more than 1.4 million older adults using a case-time-control design, allowing each individual to serve as his or her own control. Case patients were residents of Ontario, Canada, aged 67 y or older hospitalized for bradycardia between January 1, 2003 and March 31, 2008. Control patients (3∶1) were not hospitalized for bradycardia, and were matched to the corresponding case on age, sex, and a disease risk index. All patients had received cholinesterase inhibitor therapy in the 9 mo preceding the index hospitalization. We identified 1,009 community-dwelling older persons hospitalized for bradycardia within 9 mo of using a cholinesterase inhibitor. Of these, 161 cases informed the matched analysis of discordant pairs. Of these, 17 (11%) required a pacemaker during hospitalization, and six (4%) died prior to discharge. After adjusting for temporal changes in drug utilization, hospitalization for bradycardia was associated with recent initiation of a cholinesterase inhibitor (adjusted odds ratio [OR] 2.13, 95% confidence interval [CI] 1.29–3.51). The risk was similar among individuals with pre-existing cardiac disease (adjusted OR 2.25, 95% CI 1.18–4.28) and those receiving negative chronotropic drugs (adjusted OR 2.34, 95% CI 1.16–4.71). We found no such association when we replicated the analysis using proton pump inhibitors as a neutral exposure. Despite hospitalization for bradycardia, more than half of the patients (78 of 138 cases [57%]) who survived to discharge subsequently resumed cholinesterase inhibitor therapy.Conclusions:
Among older patients, initiation of cholinesterase inhibitor therapy was associated with a more than doubling of the risk of hospitalization for bradycardia. Resumption of therapy following discharge was common, suggesting that the cardiovascular toxicity of cholinesterase inhibitors is underappreciated by clinicians.
: Please see later in the article for the Editors' Summary
Published in the journal: Cholinesterase Inhibitors and Hospitalization for Bradycardia: A Population-Based Study. PLoS Med 6(9): e32767. doi:10.1371/journal.pmed.1000157
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1000157Summary
Background:
Cholinesterase inhibitors are commonly used to treat dementia. These drugs enhance the effects of acetylcholine, and reports suggest they may precipitate bradycardia in some patients. We aimed to examine the association between use of cholinesterase inhibitors and hospitalization for bradycardia.Methods and Findings:
We examined the health care records of more than 1.4 million older adults using a case-time-control design, allowing each individual to serve as his or her own control. Case patients were residents of Ontario, Canada, aged 67 y or older hospitalized for bradycardia between January 1, 2003 and March 31, 2008. Control patients (3∶1) were not hospitalized for bradycardia, and were matched to the corresponding case on age, sex, and a disease risk index. All patients had received cholinesterase inhibitor therapy in the 9 mo preceding the index hospitalization. We identified 1,009 community-dwelling older persons hospitalized for bradycardia within 9 mo of using a cholinesterase inhibitor. Of these, 161 cases informed the matched analysis of discordant pairs. Of these, 17 (11%) required a pacemaker during hospitalization, and six (4%) died prior to discharge. After adjusting for temporal changes in drug utilization, hospitalization for bradycardia was associated with recent initiation of a cholinesterase inhibitor (adjusted odds ratio [OR] 2.13, 95% confidence interval [CI] 1.29–3.51). The risk was similar among individuals with pre-existing cardiac disease (adjusted OR 2.25, 95% CI 1.18–4.28) and those receiving negative chronotropic drugs (adjusted OR 2.34, 95% CI 1.16–4.71). We found no such association when we replicated the analysis using proton pump inhibitors as a neutral exposure. Despite hospitalization for bradycardia, more than half of the patients (78 of 138 cases [57%]) who survived to discharge subsequently resumed cholinesterase inhibitor therapy.Conclusions:
Among older patients, initiation of cholinesterase inhibitor therapy was associated with a more than doubling of the risk of hospitalization for bradycardia. Resumption of therapy following discharge was common, suggesting that the cardiovascular toxicity of cholinesterase inhibitors is underappreciated by clinicians.
: Please see later in the article for the Editors' SummaryIntroduction
Cholinesterase inhibitors such as donepezil, rivastigmine, and galantamine are widely prescribed to improve cognitive function in patients with Alzheimer disease—a condition expected to quadruple in prevalence over the next 50 y [1]. By inhibiting the synaptic metabolism of acetylcholine, these drugs enhance cortical cholinergic neurotransmission [2]. Although cholinesterase inhibitors are generally well tolerated, they may provoke adverse effects in some patients because their cholinergic effects are not confined to the central nervous system [2]. Symptoms of cholinergic excess are often nonspecific and include gastrointestinal upset, diarrhea, hypersalivation, and muscle cramps. In severe instances, these drugs can increase vagal tone and thereby precipitate bradycardia.
Anecdotal reports, small observational studies, and post hoc analyses of clinical trials have produced conflicting results, with some suggesting an increased risk of bradycardia during cholinesterase inhibitor therapy and others finding no such association [3]–[12]. At the time of our study, no large-scale studies had examined, to our knowledge, whether cholinesterase inhibitor use among older patients predisposes to bradycardia.
Frail older adults represent a growing population of cholinesterase inhibitor users. These patients are more prone to the adverse effects of drugs and discontinue cholinesterase inhibitors more often than patients in clinical trials, who are typically healthier than those in clinical practice [10]. We sought to characterize the association between cholinesterase inhibitor therapy and hospitalization for bradycardia in a population of more than 1.4 million older adults.
Methods
Setting and Data Sources
We linked multiple population-based health care databases in an anonymous fashion using unique encrypted health card numbers. This linkage process has been standardized by our research institution (http://www.ices.on.ca), and these methods have been used extensively to study population-based health outcomes, including adverse drug events [13]–[20]. The Ontario Drug Benefit database was used to identify prescription records, and contains comprehensive, high-quality information regarding prescription medications dispensed to Ontario residents aged 65 y and older [21]. The Canadian Institute for Health Information (CIHI) Discharge Abstract Database was used to identify hospital admissions, and contains detailed diagnostic and procedural information for all hospital admissions in Ontario. The National Ambulatory Care Reporting System was used to identify visits to emergency departments. Basic demographic information was obtained from the Ontario Registered Persons Database. Finally, we used the Ontario Health Insurance Plan database to identify claims for inpatient and outpatient physician services. All Ontario seniors receive universal access to hospital care, physicians' services, and prescription drug coverage. The study was approved by the Research Ethics Board of Sunnybrook Health Sciences Centre.
Study Design
We used the case-time-control design to examine the association between cholinesterase inhibitor use and hospitalization for bradycardia among Ontario residents aged 67 y and older. This design is an extension of the case-crossover design first described by Maclure [22],[23], which compares within-patient exposure to a potential risk factor in the period immediately preceding a putative adverse event (the risk interval) to exposure during a different time (the reference interval). Because cases serve as their own controls, fixed patient characteristics are controlled for implicitly under this design [24],[25]. However, the case-crossover design can be vulnerable to spurious associations between a drug and an outcome owing to temporal trends in drug utilization. The case-time-control design corrects for this limitation by incorporating a control group of patients who did not experience the outcome of interest [22],[26]–[28].
Identification of Case Patients
We included all patients aged 67 y and older hospitalized with a diagnosis of bradycardia between January 1, 2003 and March 31, 2008, and restricted our analysis to those patients who were exposed to a cholinesterase inhibitor in the 9 mo prior to the index date. Because we hypothesized that bradycardia caused by cholinesterase inhibitors would be most likely to manifest during the initial period of therapy, we defined our risk interval as the 3-mo period immediately preceding hospitalization, and our reference interval as the months seven through nine prior to the index date (Figure 1). We included a 3-mo wash-out interval between the risk and reference intervals to avoid contamination between the risk and reference intervals, and excluded individuals with pacemaker insertion in the previous 5 y or hospitalization in the year preceding the study entry. Individuals with cholinesterase inhibitor prescription in the wash-out period, or both the risk and reference periods, did not contribute to the analysis.
Fig. 1. Case-time-control design. 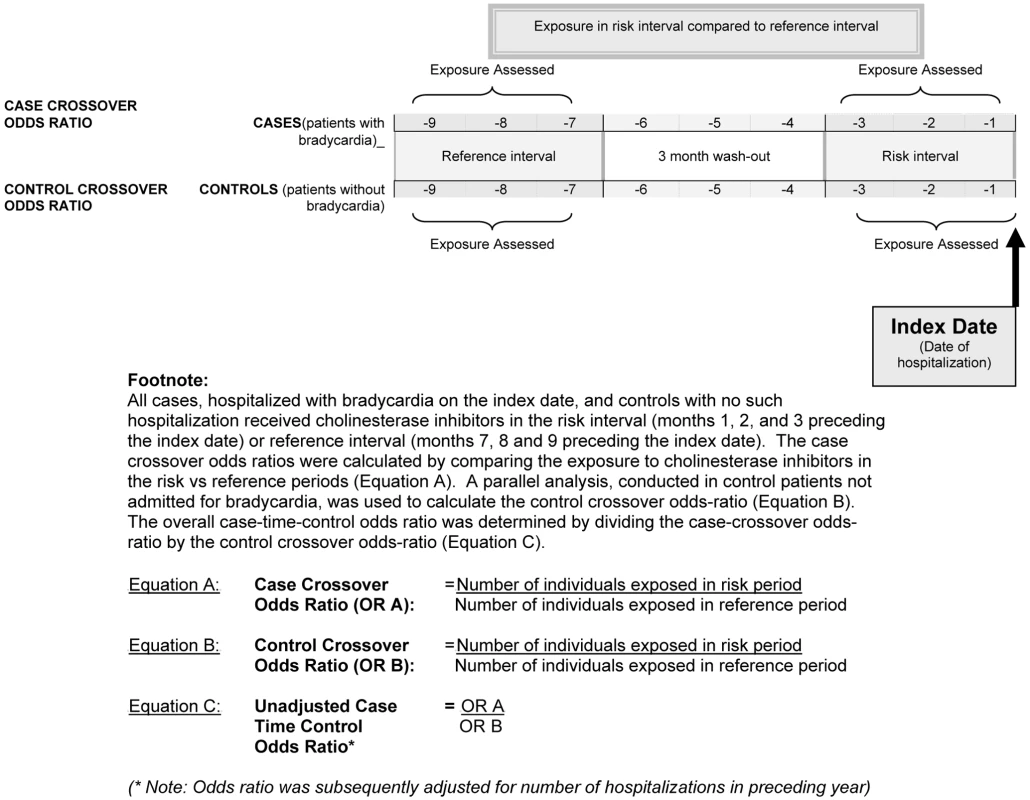
Hospitalizations included emergency department visits and hospital admissions for bradycardia, and were identified using the International Classification of Diseases and Related Health Problems Tenth Revision (ICD-10) [29] code for bradycardia (R001). All hospital visits associated with a diagnosis of bradycardia were included in this study because the CIHI Discharge Abstract Database does not contain direct information on the primary reason for hospital admission. The date of the hospitalization served as the index date, and only the first hospitalization for bradycardia was considered for patients with multiple such admissions during the study period.
Identification of Control Patients
In keeping with the case-time-control design, we corrected for temporal changes in cholinesterase inhibitor use by matching each case with up to three control patients. Control patients did not experience a hospitalization for bradycardia on or before the index date, but did receive at least one prescription for a cholinesterase inhibitor in either of the corresponding risk or reference intervals preceding the index date (Figure 1).
To minimize differences between case and control patients, we selected controls matched on age (born within 1 y of case), sex, and their anticipated risk of bradycardia using a disease risk index, as done previously [30],[31]. The disease risk index was derived by constructing a multivariable regression model that included multiple potential predictors of bradycardia or death, including socioeconomic status, residence in long-term care facility, overall number of prescription drugs prescribed in the preceding year, beta-blockers, calcium channel blockers, digoxin, antiarrhythmics, nitrates, anticoagulants, antiplatelets, diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, HMG-CoA reductase inhibitors, fibric acid derivatives, ezetimibe, oral hypoglycemic agents, insulin, antipsychotic medications, antidepressants, sedative-hypnotics, chemotherapy, corticosteroids, overall number physician clinic visits, emergency department visits, cardiologist visits, internist visits, neurologist visits, geriatrician visits, psychiatrist visits, coronary artery bypass graft, angiography, percutaneous transluminal coronary angioplasty, valve surgery, carotid endarterectomy, peripheral vascular disease procedures, dialysis, echocardiography, electrocardiography, holter monitor, nuclear medicine stress test, carotid doppler ultrasonography, charlson comorbidity index score, renal dysfunction, liver dysfunction, heart failure, diabetes, cancer, cerebrovascular disease (strokes, transient ischemic attacks), cardiac dysrhythmias, myocardial infarction, angina and coronary artery disease, peripheral vascular disease, major infections (respiratory, urogenital, abdominal, gastrointestinal, skin, soft tissue), and alcoholism (Text S1). These potential confounders were consequently summarized into a single disease risk index that predicted the probability of hospital admission for bradycardia [30],[32]. We selected up to three controls with the disease risk scores (within 0.2 standard deviation) closest to the given case.
Statistical Analysis
We derived the case-time-control odds ratio [OR] by dividing the crossover OR among the cases (i.e., the case-crossover group) by the crossover OR among the controls (i.e., the control-crossover group), thereby producing a case-control OR adjusted for time-trend (Figure 1). Crossover ORs were derived from the ratio of discordant pairs, i.e., the number of individuals exposed exclusively during the risk interval as compared to exclusively during the reference interval [27]. By assuming conditional independence of exposure within each 1∶3 matched set, a conditional logistic regression model, adjusting for the length of stay in hospital in the year preceding study entry as an additional measure of comorbidity, was fitted to estimate the overall OR and 95% confidence intervals (CIs) [27].
We hypothesized that individuals with pre-existing cardiovascular disease and individuals co-using negative chronotropic agents might be at particularly high risk for bradycardia. To examine these risk groups, we performed a stratified analysis in those with a history of cardiovascular disease (defined as previous myocardial infarction, congestive heart failure, angina, or arrhythmias), and those coprescribed negative chronotropic medications such as beta-adrenergic antagonists, digoxin, or the nondihydropyridine calcium channel antagonists verapamil and diltiazem.
Drug interactions with cholinesterase inhibitors can occur via the cytochrome P450 enzyme 2D6. However, given the relatively few P450 2D6 inhibitors, we felt it was more relevant to focus on the pharmacodynamic interaction between cholinesterase inhibitors and negative chronotropic agents.
To test the specificity of our findings, we performed a sensitivity analysis in which proton pump inhibitors served as the exposure of interest rather than cholinesterase inhibitors. All analyses used a two-sided type I error rate of 0.05 and were performed using SAS version 9.1 (SAS Institute).
Results
Between January 1, 2003 and March 31, 2008, we identified 27,333 hospitalizations for bradycardia among Ontario residents 67 y and older. Of these, 10,323 were excluded because they were hospitalized in the year prior to the index date, and 15,805 were excluded because they had not used cholinesterase inhibitors in the 9 mo prior to index date (Figure 2). Among the remaining patients, we further excluded 191 individuals exposed to cholinesterase inhibitors during the wash-out interval, and patients who had a pacemaker or could not be matched to at least one control (n≤5), leaving 1,009 eligible cases. Among these cases, 848 (84%) received a cholinesterase inhibitor in both the risk and reference periods, leaving 161 cases to inform our matched pairs analysis of individuals who had received a cholinesterase inhibitor in either the risk or reference period, but not both. Of these cases, 148 (92%) were fully matched to three controls and 157 (98%) were matched to at least two controls. We identified 466 matched controls from 42,833 potential controls.
Fig. 2. Flow diagram of case selection. 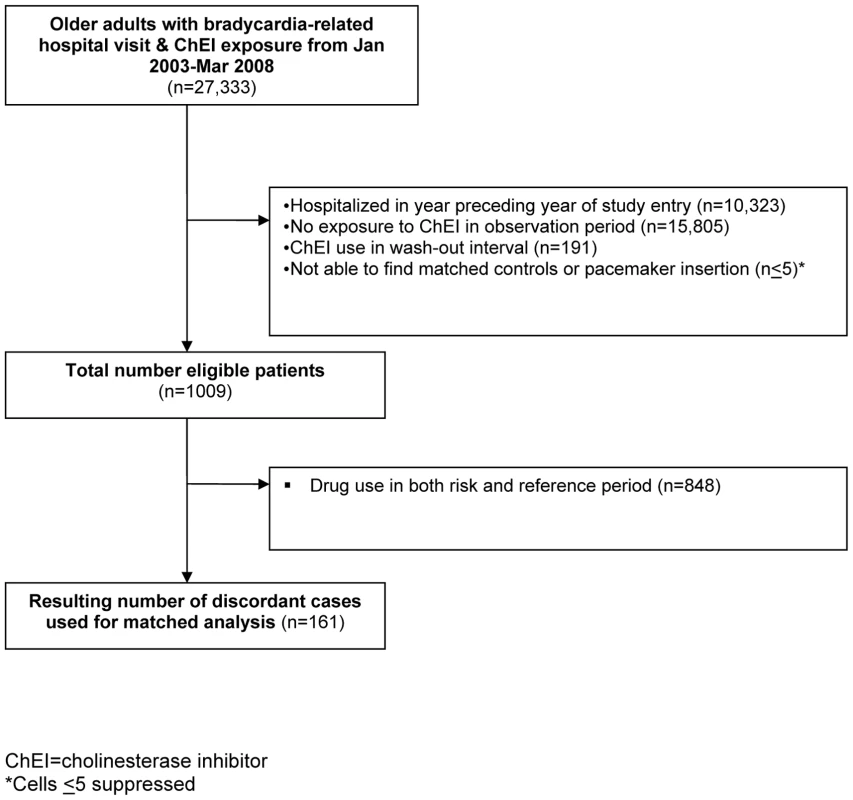
The characteristics of cases and controls were highly similar (Table 1). The mean age of patients was 83 y (standard deviation 5.4 y) and 320 (51%) were female. A higher proportion of controls were in long-term care facilities, although the overall proportion remained low in both groups. Donepezil was the most frequently prescribed cholinesterase inhibitor in these patients accounting for 117 of the 161 (73%) cases and 292 of the 466 (63%) controls. Seventeen patients (11%) received a pacemaker during their hospitalization, and six (4%) individuals died prior to discharge from hospital.
Tab. 1. Characteristics of cases and controls. 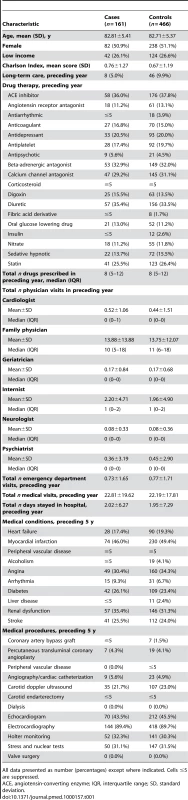
All data presented as number (percentages) except where indicated. Cells ≤5 are suppressed. In the primary analysis, recent initiation of cholinesterase inhibitors was significantly associated with hospitalization for bradycardia (adjusted OR 2.13, 95% CI 1.29–3.51, p = 0.003; Table 2). Among cases and controls with previously diagnosed cardiac disease, the association between recent use of cholinesterase inhibitors and bradycardia was similar (adjusted OR 2.25, 95% CI 1.18–4.28, p = 0.014). The association persisted among the cases and controls receiving negative chronotropic medications (adjusted OR 2.34; 95% CI 1.16–4.71, p = 0.017). As expected, we found no association between recent initiation of proton pump inhibitors and bradycardia (adjusted OR 1.13, 95% CI 0.93–1.37, p = 0.228).
Tab. 2. Risk of bradycardia-related hospital admissions and recent cholinesterase inhibitor use. 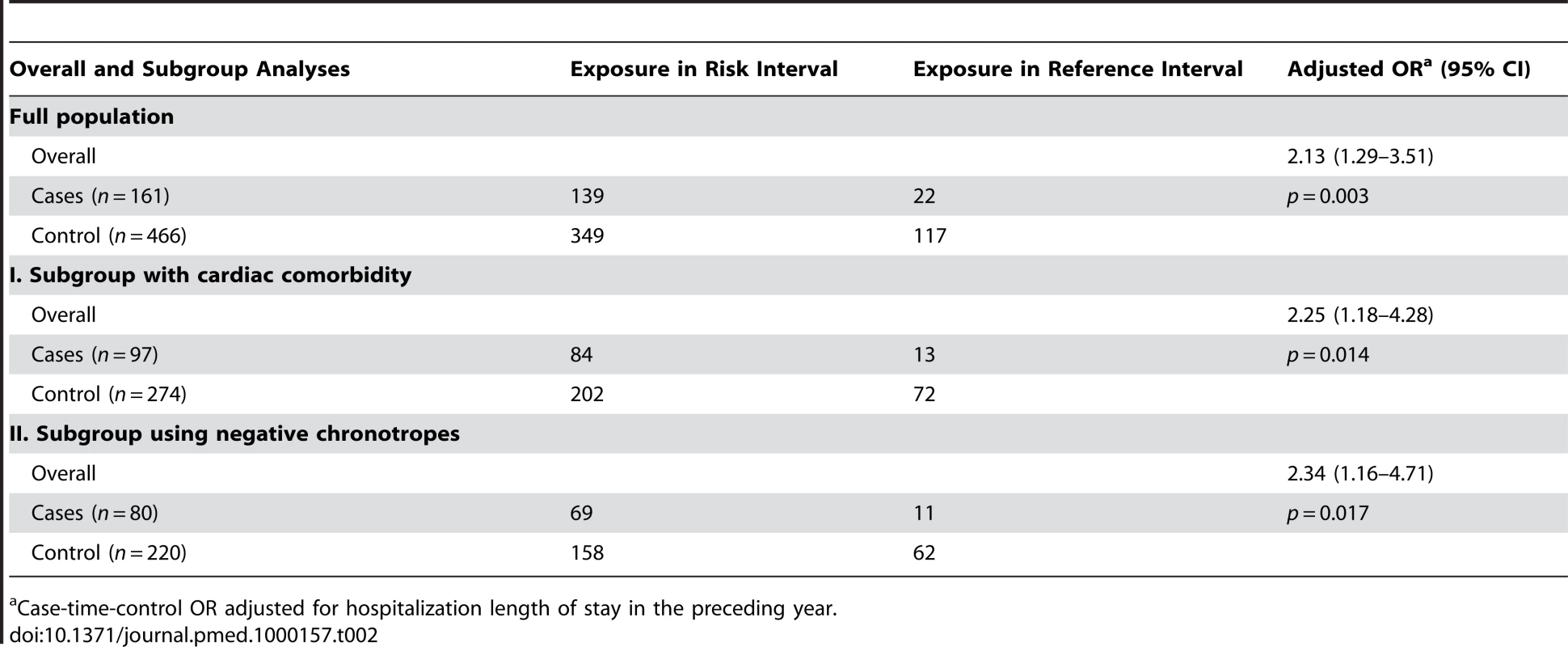
Case-time-control OR adjusted for hospitalization length of stay in the preceding year. Secondary Analyses
Because bradycardia is a relatively common occurrence in older patients, we hypothesized that the potential contribution of cholinesterase inhibitors to the development of bradycardia might not be recognized, and that therapy might be continued following discharge. After excluding individuals who received pacemakers during their hospital stay, 138 cases survived to discharge. Of these cases, subsequent prescription records indicated that cholinesterase inhibitors were restarted in 78 individuals (57%) within 100 d of hospital discharge. A post hoc examination of the 3-mo period following resumption of therapy in those 78 individuals showed that three (3.8%) individuals were readmitted to hospital or visited the emergency department with a diagnosis of bradycardia.
Discussion
Using the health care records of more than 1.4 million Ontario residents aged 67 y and older, we found that treatment with cholinesterase inhibitors was associated with a doubling in the risk of hospitalization for bradycardia. Importantly, although cholinesterase inhibitors are reversible precipitants of bradycardia, the drugs were resumed following discharge in greater than half the cases, presumably because the potential causative role of these drugs in the hospitalization was not appreciated. In many patients, cholinesterase inhibitors are associated with marginal improvement in cognition and global functioning [1],[33]. Consequently, recent guidelines suggest that cholinesterase inhibitors should not be standard of care for patients with dementia, but instead urge physicians to weigh each individual's expected risks and benefits before initiating therapy. Our large-scale population-based assessment of the risk of bradycardia with cholinesterase inhibitors in clinical practice should help inform the risk-benefit assessment for clinicians and patients. A recent study used an alternate cohort design to examine a primary outcome of syncope in patients receiving cholinesterase inhibitors. In a secondary analysis, these investigators also observed an elevated risk of bradycardia (adjusted hazard ratio 1.69; 95% CI 1.32–2.15) associated with cholinesterase inhibitor use, which complements the findings of our study [34].
The risk of bradycardia observed in our study may cause clinicians and patients to reconsider therapy with these drugs, particularly for patients in whom little or no cognitive improvement is observed early in therapy [35],[36]. At a minimum, our findings should alert clinicians to the potential role of cholinesterase inhibitors in patients with bradycardia, for whom resumption of treatment may be inadvisable.
Our study has several limitations that merit emphasis. Administrative databases contain information on hospitalizations, emergency department visits, diagnoses, procedures, physicians' claims, outpatient clinic visits, and drug dispensing data. However, they lack the clinical richness of a medical chart. Accordingly, we were not able to capture the severity of dementia, lifestyle habits such as smoking, diet, alcohol use, exercise, over-the-counter drug use, in-hospital drug use, laboratory values, and the results of diagnostic testing.
However, we relied on the unique crossover design feature that controls for fixed patient characteristics by allowing each patient to serve as his or her own control. Consequently, concerns regarding potential confounders, including disease severity, were largely overcome. The crossover design also relies on the temporal association between an exposure and outcome, and this feature enabled us to examine whether bradycardia-related hospitalization was likely secondary to cholinesterase inhibitors as opposed to underlying comorbidities. More specifically, the crossover design examines whether an exposure is more likely to occur immediately preceding an event or during another period when bradycardia did not occur. If the exposure is not associated with the outcome, then no temporal association would be expected. The presence of underlying comorbidities would not be expected to confound the cholinesterase inhibitor–bradycardia relationship unless the comorbidities were associated with both cholinesterase inhibitor use and bradycardia. To further control for confounding, we corrected for temporal changes in cholinesterase inhibitor use by matching each case with up to three control patients on the basis of an extensive disease risk index score.
We identified episodes of bradycardia resulting in emergency department visits or hospital admissions, but we were unable to identify individuals in whom bradycardia did not culminate in hospital care, including cases in which bradycardia led to death [37]. Therefore, our analysis likely underestimates the true risk of cardiovascular harm associated with cholinesterase inhibitors. The coding for bradycardia has not been validated and it is possible that some cases of bradycardia were missed if the code for bradycardia has low sensitivity. However, we expect that the positive predictive value for the bradycardia code would be reasonable because the diagnosis for bradycardia is based upon a fairly straightforward medical assessment. The occurrence of random miscoding would only have attenuated our estimates and biased the results towards the null. It is likely that the cases of bradycardia captured in our study were clinically significant because they were severe enough to be documented in the patient's chart and coded in the CIHI database.
We were unable to assess the absolute risk of bradycardia due to cholinesterase inhibitor therapy, and we could not be certain that resumption of cholinesterase inhibitors following hospital discharge truly reflected a lack of appreciation for the potential negative chronotropic effects of therapy. Since most patients were taking donepezil, we were not able to contrast risks with individual cholinesterase inhibitors given the low prevalence of use with the other agents. Future studies are needed to address the relative harms of the individual drugs in this class.
Our post hoc examination of the 78 patients who resumed cholinesterase inhibitor after hospital discharge showed that only 4% were readmitted to hospital or visited the emergency department with a diagnosis of bradycardia in the 3 mo following resumption of therapy. It is hard to know how to interpret this post hoc analysis. We did not evaluate out-of-hospital death, and could not ascertain whether cholinesterase inhibitor therapy was restarted with a reduced dose or more gradual dose titration, whether changes to other medications were made, or whether closer outpatient follow up for bradycardia was undertaken.
Finally, because we relied on drug dispensing data as a proxy for drug adherence, there was a potential for exposure misclassification.
While bias and confounding can threaten any observational study, the likelihood of these was reduced substantially by the design of our study, in which every case served as his or her own control, thereby lessening between-patient variability, and by the use of a disease risk index, an advanced matching technique, which resulted in considerable similarity between cases and controls (Table 1) [31],[32].
In summary, we found that cholinesterase inhibitors are associated with a significantly increased risk of hospitalization for bradycardia among older outpatients, and that the risk is similar in patients with cardiovascular comorbidity and those receiving concurrent therapy with negative chronotropic drugs. Our findings highlight the importance of careful clinical evaluation prior to initiating cholinesterase inhibitor therapy, and vigilant monitoring thereafter in order to prevent adverse cardiac events. Cholinesterase inhibitors should be prescribed judiciously, and because these drugs carry a risk of serious adverse events, they should be continued only if the benefits outweigh the risks. Finally, it is important for clinicians to be aware of the potential negative chronotropic effects of cholinesterase inhibitors, and reassess the merits of continued therapy in patients who develop bradycardia while taking these drugs. The frequent resumption of cholinesterase inhibitors following discharge suggests that bradycardia may not be widely recognized as a potential adverse effect of this class of medications.
Supporting Information
Zdroje
1. QaseemA
SnowV
CrossJT,Jr
ForcieaMA
HopkinsR,Jr
2008 Current pharmacologic treatment of dementia: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med 148 370 378
2. MasudaY
2004 Cardiac effect of cholinesterase inhibitors used in Alzheimer's disease–from basic research to bedside. Curr Alzheimer Res 1 315 321
3. Calvo-RomeroJM
Ramos-SaladoJL
1999 [Symptomatic sinus bradycardia associated with donepezil]. Revista de Neurologia 28 1070 1072
4. SuleymanT
TevfikP
AbdulkadirG
OzlemS
2006 Complete atrioventricular block and ventricular tachyarrhythmia associated with donepezil. Emerg Med J 23 641 642
5. BordierP
GarrigueS
BaroldSS
BressollesN
LanusseS
2003 Significance of syncope in patients with Alzheimer's disease treated with cholinesterase inhibitors. Europace 5 429 431
6. NewbyVJ
KennyRA
McKeithIG
2004 Donepezil and cardiac syncope: a case report. Int J Geriatr Psychiatry 19 1110 1112
7. TavassoliN
SommetA
Lapeyre-MestreM
BagheriH
MontrastrucJ
2007 Drug interactions with cholinesterase inhibitors: an analysis of the french pharmacovigilance database and a comparison of two national drug formularies. Drug Safety 30 1063 1071
8. RoisinT
Van ErmenA
RogiersA
2006 Cardiac adverse effects with cholinesterase inhibitors. Drug Safety 29 930
9. ShepherdG
Klein-SchwartzW
EdwardsR
1999 Donepezil overdose: a tenfold dosing error. Ann Pharmacother 33 812 815
10. GillSS
BronskillSE
MamdaniM
SykoraK
LiP
2004 Representation of patients with dementia in clinical trials of donepezil. Can J Clin Pharmacol 11 e274 e285
11. BordierP
GarrigueS
LanusseS
MargaineJ
RobertF
2006 Cardiovascular effects and risk of syncope related to donepezil in patients with Alzheimer's disease. CNS Drugs 20 411 417
12. MorganrothJ
GrahamS
HartmanR
AnandR
2002 Electrocardiographic effects of rivastigmine. J Clin Pharmacol 42 558 568
13. JuurlinkDN
MamdaniMM
LeeDS
KoppA
AustinPC
2004 Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med 351 543 551
14. MamdaniM
JuurlinkDN
LeeDS
RochonPA
KoppA
2004 Cyclo-oxygenase-2 inhibitors versus non-selective non-steroidal anti-inflammatory drugs and congestive heart failure outcomes in elderly patients: a population-based cohort study. Lancet 363 1751 1756
15. RayJG
MamdaniM
TsuyukiRT
AndersonDR
YeoEL
2001 Use of statins and the subsequent development of deep vein thrombosis. Arch Intern Med 161 1405 1410
16. LeeDS
TuJV
JuurlinkDN
AlterDA
KoDT
2005 Risk-treatment mismatch in the pharmacotherapy of heart failure. JAMA 294 1240 1247
17. LipscombeLL
GomesT
LevesqueLE
HuxJE
JuurlinkDN
2007 Thiazolidinediones and cardiovascular outcomes in older patients with diabetes. JAMA 298 2634 2643
18. JuurlinkDN
MamdaniM
KoppA
LaupacisA
RedelmeierDA
2003 Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA 289 1652 1658
19. MamdaniMM
TuK
van WalravenC
AustinPC
NaylorCD
2000 Postmenopausal estrogen replacement therapy and increased rates of cholecystectomy and appendectomy. CMAJ 162 1421 1424
20. Park-WyllieLY
JuurlinkDN
KoppA
ShahBR
StukelTA
2006 Outpatient gatifloxacin therapy and dysglycemia in older adults. N Engl J Med 354 1352 1361
21. LevyAR
O'BrienBJ
SellorsC
GrootendorstP
WillisonD
2003 Coding accuracy of administrative drug claims in the Ontario Drug Benefit database. Can J Clin Pharmacol 10 67 71
22. MaclureM
1991 The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol 133 144 153
23. MaclureM
MittlemanMA
2000 Should we use a case-crossover design? Annual Review of Public Health 21 193 221
24. DonnanPT
WangJ
2001 The case-crossover and case-time-control designs in pharmacoepidemiology. Pharmacoepidemiol Drug Saf 10 259 262
25. SchneeweissS
SturmerT
MaclureM
1997 Case-crossover and case-time-control designs as alternatives in pharmacoepidemiologic research. Pharmacoepidemiol Drug Saf 6 (Suppl 3) S51 S59
26. SuissaS
1998 The case-time-control design: further assumptions and conditions. Epidemiology 9 441 445
27. SuissaS
1995 The case-time-control design. Epidemiology 6 248 253
28. GreenlandS
1996 Confounding and exposure trends in case-crossover and case-time-control designs. Epidemiology 7 231 239
29. Canadian Institute for Health Information 2003 The International Statistical Classification of Diseases and Related Health Problems - Tenth Revision Ottawa, Canada Canadian Institute for Health Information
30. JuurlinkDN
MamdaniMM
KoppA
RedelmeierDA
2006 The risk of suicide with selective serotonin reuptake inhibitors in the elderly. Am J Psychiatry 163 813 821
31. ArbogastPG
RayWA
2009 Use of disease risk scores in pharmacoepidemiologic studies. Stat Methods Med Res 18 67 80
32. ArbogastPG
KaltenbachL
DingH
RayWA
2008 Adjustment for multiple cardiovascular risk factors using a summary risk score. Epidemiology 19 30 37
33. RainaP
SantaguidaP
IsmailaA
PattersonC
CowanD
2008 Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med 148 379 397
34. GillSS
AndersonGM
FischerHD
BellCM
LiP
2009 Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med 169 867 873
35. WinbladB
GauthierS
ScintoL
FeldmanH
WilcockGK
2008 Safety and efficacy of galantamine in subjects with mild cognitive impairment. Neurology 70 2024 2035
36. US FDA 2005 Possible increased mortality in patients with mild cognitive impairment. Dear Healthcare Professional Letter: www.fda.gov/medwatch/SAFETY/2005/reminylDDLmarch.pdf
37. GreenbergHM
1984 Bradycardia at onset of sudden death: potential mechanisms. Ann N Y Acad Sci 427 241 252
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2009 Číslo 9- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Ghostwriting: The Dirty Little Secret of Medical Publishing That Just Got Bigger
- Ensuring Integrity in Comparative Effectiveness Research: Accentuate the Negative
- The GRADE System for Rating Clinical Guidelines
- Improving the Quantitative Basis of the Surgical Burden in Low-Income Countries
- Cholinesterase Inhibitors and Hospitalization for Bradycardia: A Population-Based Study
- Inflammatory Markers and Outcomes in Cardiovascular Disease
- Changing Patterns of Dengue Epidemiology and Implications for Clinical Management and Vaccines
- Grading Quality of Evidence and Strength of Recommendations: A Perspective
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Changing Patterns of Dengue Epidemiology and Implications for Clinical Management and Vaccines
- Grading Quality of Evidence and Strength of Recommendations: A Perspective
- Inflammatory Markers and Outcomes in Cardiovascular Disease
- The GRADE System for Rating Clinical Guidelines
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



