Global Estimates of Syphilis in Pregnancy and Associated Adverse Outcomes: Analysis of Multinational Antenatal Surveillance Data
Background:
The World Health Organization initiative to eliminate mother-to-child transmission of syphilis aims for ≥90% of pregnant women to be tested for syphilis and ≥90% to receive treatment by 2015. We calculated global and regional estimates of syphilis in pregnancy and associated adverse outcomes for 2008, as well as antenatal care (ANC) coverage for women with syphilis.
Methods and Findings:
Estimates were based upon a health service delivery model. National syphilis seropositivity data from 97 of 193 countries and ANC coverage from 147 countries were obtained from World Health Organization databases. Proportions of adverse outcomes and effectiveness of screening and treatment were from published literature. Regional estimates of ANC syphilis testing and treatment were examined through sensitivity analysis. In 2008, approximately 1.36 million (range: 1.16 to 1.56 million) pregnant women globally were estimated to have probable active syphilis; of these, 80% had attended ANC. Globally, 520,905 (best case: 425,847; worst case: 615,963) adverse outcomes were estimated to be caused by maternal syphilis, including approximately 212,327 (174,938; 249,716) stillbirths (>28 wk) or early fetal deaths (22 to 28 wk), 91,764 (76,141; 107,397) neonatal deaths, 65,267 (56,929; 73,605) preterm or low birth weight infants, and 151,547 (117,848; 185,245) infected newborns. Approximately 66% of adverse outcomes occurred in ANC attendees who were not tested or were not treated for syphilis. In 2008, based on the middle case scenario, clinical services likely averted 26% of all adverse outcomes. Limitations include missing syphilis seropositivity data for many countries in Europe, the Mediterranean, and North America, and use of estimates for the proportion of syphilis that was “probable active,” and for testing and treatment coverage.
Conclusions:
Syphilis continues to affect large numbers of pregnant women, causing substantial perinatal morbidity and mortality that could be prevented by early testing and treatment. In this analysis, most adverse outcomes occurred among women who attended ANC but were not tested or treated for syphilis, highlighting the need to improve the quality of ANC as well as ANC coverage. In addition, improved ANC data on syphilis testing coverage, positivity, and treatment are needed.
Please see later in the article for the Editors' Summary
Published in the journal:
Global Estimates of Syphilis in Pregnancy and Associated Adverse Outcomes: Analysis of Multinational Antenatal Surveillance Data. PLoS Med 10(2): e32767. doi:10.1371/journal.pmed.1001396
Category:
Research Article
doi:
https://doi.org/10.1371/journal.pmed.1001396
Summary
Background:
The World Health Organization initiative to eliminate mother-to-child transmission of syphilis aims for ≥90% of pregnant women to be tested for syphilis and ≥90% to receive treatment by 2015. We calculated global and regional estimates of syphilis in pregnancy and associated adverse outcomes for 2008, as well as antenatal care (ANC) coverage for women with syphilis.
Methods and Findings:
Estimates were based upon a health service delivery model. National syphilis seropositivity data from 97 of 193 countries and ANC coverage from 147 countries were obtained from World Health Organization databases. Proportions of adverse outcomes and effectiveness of screening and treatment were from published literature. Regional estimates of ANC syphilis testing and treatment were examined through sensitivity analysis. In 2008, approximately 1.36 million (range: 1.16 to 1.56 million) pregnant women globally were estimated to have probable active syphilis; of these, 80% had attended ANC. Globally, 520,905 (best case: 425,847; worst case: 615,963) adverse outcomes were estimated to be caused by maternal syphilis, including approximately 212,327 (174,938; 249,716) stillbirths (>28 wk) or early fetal deaths (22 to 28 wk), 91,764 (76,141; 107,397) neonatal deaths, 65,267 (56,929; 73,605) preterm or low birth weight infants, and 151,547 (117,848; 185,245) infected newborns. Approximately 66% of adverse outcomes occurred in ANC attendees who were not tested or were not treated for syphilis. In 2008, based on the middle case scenario, clinical services likely averted 26% of all adverse outcomes. Limitations include missing syphilis seropositivity data for many countries in Europe, the Mediterranean, and North America, and use of estimates for the proportion of syphilis that was “probable active,” and for testing and treatment coverage.
Conclusions:
Syphilis continues to affect large numbers of pregnant women, causing substantial perinatal morbidity and mortality that could be prevented by early testing and treatment. In this analysis, most adverse outcomes occurred among women who attended ANC but were not tested or treated for syphilis, highlighting the need to improve the quality of ANC as well as ANC coverage. In addition, improved ANC data on syphilis testing coverage, positivity, and treatment are needed.
Please see later in the article for the Editors' Summary
Introduction
Syphilis is a severe bacterial disease that in pregnancy may manifest as stillbirth, early fetal death, low birth weight, preterm delivery, neonatal death, or infection or disease in the newborn. Both archaeological and literary evidence suggest that mother-to-child transmission (MTCT) of syphilis, commonly referred to as “congenital syphilis,” is an ancient scourge [1],[2]. In modern times the effectiveness of syphilis testing and treatment in preventing MTCT of syphilis is well-recognized [3]. Diagnosis and prevention of MTCT of syphilis is feasible, inexpensive, and cost-effective in nearly every situation evaluated [4]. Yet, despite the tools being available for over 60 y, MTCT of syphilis persists as a public health problem.
It is unknown exactly what proportion of pregnant women globally receives adequate testing and treatment for syphilis. The World Health Organization (WHO) has begun to monitor syphilis testing and treatment coverage through the HIV Universal Access reporting system, but quality data are not yet available from all countries. In 2011, 63 of 149 low- and middle-income countries reported on coverage of syphilis testing within antenatal care (ANC), with a median of 68% of women in the reporting countries being tested for syphilis at first ANC visit [5]. However, this coverage estimate may be an overestimate of syphilis testing coverage in low- and middle-income countries, as those countries without a functional syphilis screening program are unlikely to have a functional reporting system. A recent multi-country study to assess introduction of rapid point-of-care tests found that ANC syphilis testing at baseline was nonexistent in the Amazonas region of Brazil, 1.7% in Kampala Hospital and rural ANC centers in Uganda, 17.8% in the district hospital and 51 health facilities in Geita District, Tanzania, 51% in a maternity hospital in Lima and ANC centers in Callao, Peru, and 79.9% in Lusaka Hospital and rural ANC centers in Mongu District, Zambia [6]. Other individual country reports have also documented a low coverage of testing and treatment of syphilis in pregnant women. For example, a study in southern China found that 57% of pregnant women were tested for syphilis from 2004 to 2008 [7]. Another study in two provinces in South Africa found that although 71% of pregnant women were tested for syphilis at first ANC visit, only 74% of women who tested positive for syphilis had treatment documented, and only 36% of seropositive women with documented treatment received the recommended three doses of intramuscular penicillin [8].
In 2007, WHO launched its Initiative for the Global Elimination of Congenital Syphilis, with the goal that by 2015 at least 90% of pregnant women are tested for syphilis and at least 90% of seropositive pregnant women receive adequate treatment [4]. The elimination initiative was designed around improving four public health “pillars”: political advocacy and community engagement; adequate coverage and quality of ANC; access to and quality of syphilis testing in ANC; and routine surveillance, monitoring, and evaluation. The regions of the Americas and the Asia Pacific have also launched elimination initiatives, in both cases initiatives integrated with elimination of MTCT of HIV [9],[10].
In order to assess progress in elimination of MTCT of syphilis and to guide policy and advocacy efforts, global data on the burden of syphilis in pregnancy and associated adverse outcomes are needed. Unfortunately, MTCT of syphilis cannot be easily measured globally because definitive diagnosis is difficult, even in developed countries with robust laboratory infrastructure. Thus, estimating the burden of disease must rely on modeled data. In 2007 WHO reported global estimates for congenital syphilis burden based on a review of published data from 1997 through 2003. This work estimated that annually there were 2,036,753 syphilis infections among pregnant women, of which 65% (1,323,889; range: 728,547 to 1,527,565) resulted in adverse pregnancy outcomes [11]. The 1997–2003 estimates were based upon 45 published studies representing 31 countries. All included studies had a sample size of at least 100 women and determined syphilis seropositivity using both treponemal and non-treponemal tests. The 1997–2003 estimates excluded studies from the United States, Canada, and most of Europe because syphilis is rare in these countries and they would not contribute meaningful numbers of congenital syphilis. The 1997–2003 estimates also did not take existing treatment services into account and did not remove background mortality and morbidity (i.e., expected adverse outcomes that would occur in uninfected women).
In order to support the global initiative for elimination of congenital syphilis, WHO has developed 2008 global estimates of maternal syphilis and associated adverse pregnancy outcomes. The 2008 numbers are intended not only to update the earlier 1997–2003 estimates, but also to use a stronger methodology to take into account existing treatment services, remove background mortality, and incorporate data from a greater number of countries. These updated estimates can be used to guide global and regional policy, program, and advocacy efforts to strengthen maternal and child health services and to monitor progress to eliminate MTCT of syphilis.
Methods
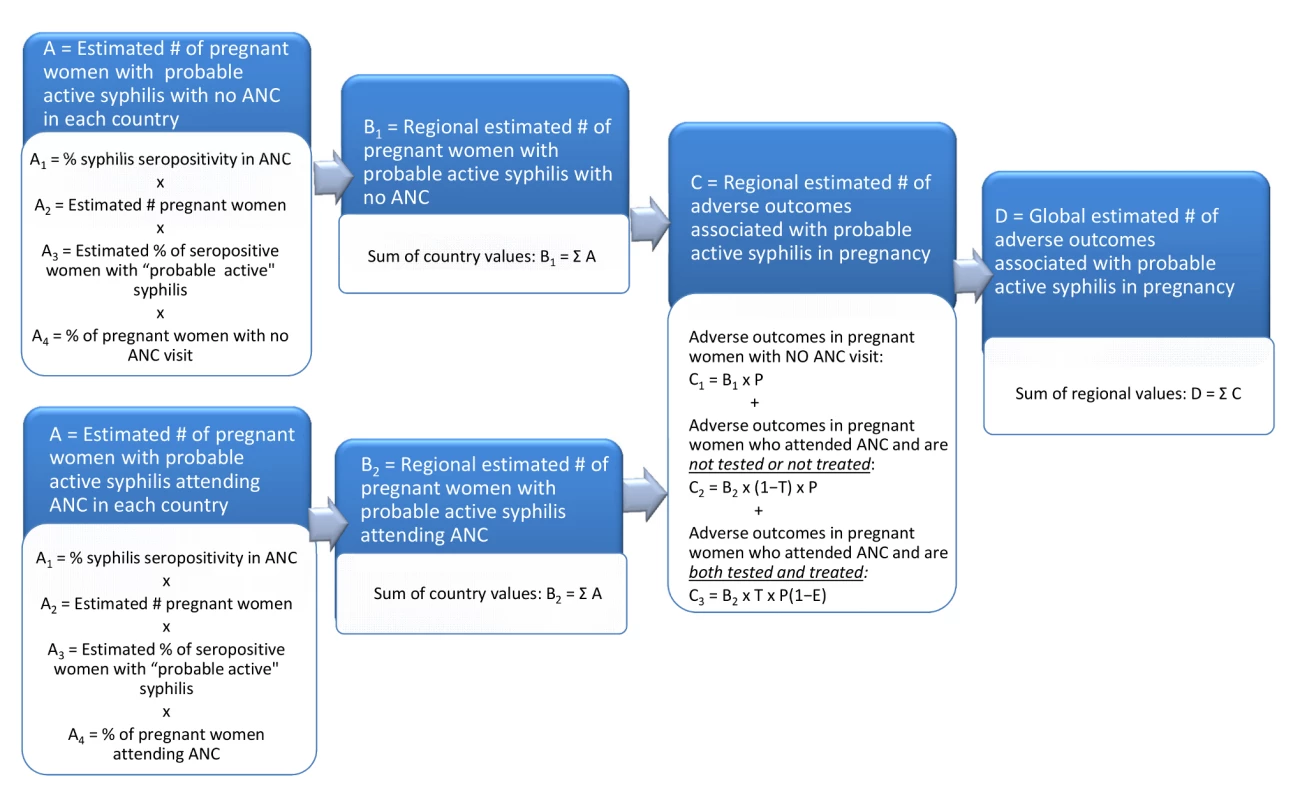
The objective of this analysis was to estimate for 2008 the global and regional number of pregnant women infected with probable active syphilis, as well as the number of associated adverse outcomes of syphilis in pregnancy. This analysis is based upon a health service delivery model that involved four estimation steps (Figure 1): calculation of the number of pregnant women with probable active syphilis in each country, calculation of the number of pregnant women with probable active syphilis in each region, calculation of the number of adverse pregnancy outcomes associated with syphilis in each region, and calculation of the global number of adverse pregnancy outcomes related to syphilis.
Wherever possible, this analysis was done using data provided routinely by countries to United Nations organizations (country-specific data points are available in Dataset S1). Countries were allocated to one of six regions based on WHO regional classifications [12]. For this analysis we defined “probable active syphilis infection” as seropositivity on both treponemal and non-treponemal tests, because women without confirmed test results may have had false positive tests or old or untreated disease that would be unlikely to pose a risk of syphilis transmission to the fetus. We defined “stillbirth” as death of a fetus of at least 28 wk gestation or at least 1,000 g weight, and “early fetal death” as fetal death occurring from 22 to 28 wk gestation (i.e., second and early third trimester); we did not include first trimester losses (miscarriages) [13].
Step A: Estimate the Number of Pregnant Women with Probable Active Syphilis in Each Country
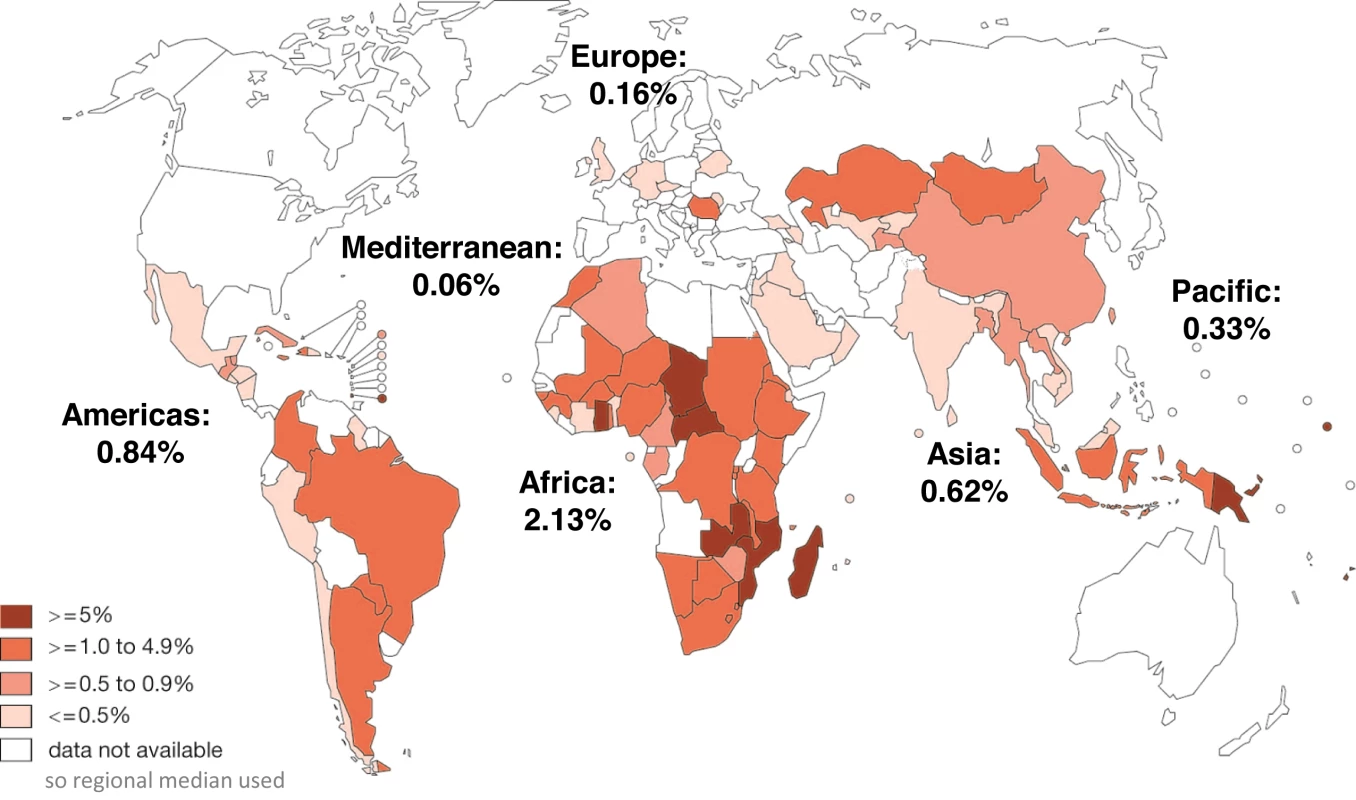
For Step A1, data on syphilis seropositivity among ANC attendees for each country were those data reported through the WHO HIV Universal Access reporting system for 2008 (data available at the WHO Global Health Observatory Data Repository: http://apps.who.int/gho/data/?theme=main). If 2008 data were not available, we used data reported for 2009 (Figure 2). In 2008 and 2009, data were reported for 97 of 193 countries (50.3%). A regional median was used for countries that did not report data in 2008 or 2009. Countries could report either ANC sentinel survey results or routinely conducted antenatal program data to the HIV Universal Access reporting system. In this reporting system, type of syphilis test used is not reported; thus, it was not possible to distinguish whether reported seropositivity was based upon treponemal, non-treponemal, or combined test results.
The estimated number of pregnant women in Step A2 was calculated for each country as the sum of the number of live births per United Nations Population Division estimates for 2008, stillbirths (after 28 wk gestation) per 2008 published estimates, and early fetal deaths (22–28 wk gestation) [14]. Estimates of early fetal deaths are not available for many countries; thus, we estimated these to be approximately 20% of stillbirths based on the early to late fetal death relationship in a limited number of studies mainly in high-income countries [15],[16]. Estimations of fetal deaths did not include first trimester losses (miscarriages).
Step A3 included an estimation of the proportion of seropositive pregnant women with probable active syphilis infection. A value of 65% was used as a correction factor to estimate the proportion of seropositive women with both treponemal and non-treponemal syphilis test positivity for the data reported through the HIV Universal Access reporting system. The correction factor was based on data from a literature review of 45 studies on syphilis in pregnancy from 2004 to 2008 [17]. Of these, three studies reported results of treponemal and non-treponemal tests for all pregnant women [18]–[20]. Among all women with either syphilis test positive, the proportion of women with both the treponemal test and the non-treponemal test positive was found to be 63.9% in Mozambique, 61.7% in Bolivia, and 68.0% in Tanzania.
Step A4 involved estimating for each country the proportion of pregnant women with and without at least one ANC visit. We used the most recent data for a country available in the WHO Global Health Observatory from 2000 to 2010; data were available for 147 countries [21]. A regional median was used for countries for which data were not available. The four values in Step A were multiplied to obtain the estimated number of pregnant women infected with probable active syphilis attending and not attending ANC in each country.
An approximate uncertainty range for the global number of pregnant women with probable active syphilis was calculated using the delta method and a 10% relative error at the national level for three input variables: syphilis seropositivity, number of pregnancies, and the correction factor for the estimated proportion of women with syphilis with probable active disease.
Step B: Estimate the Number of Pregnant Women Infected with Probable Active Syphilis in Each Region
Step B involved summing the country values to provide regional estimates of the number of pregnant women with probable active syphilis not attending ANC (B1), as well as the number attending ANC (B2).
Step C: Estimate the Number of Adverse Pregnancy Outcomes Associated with Syphilis in Each Region
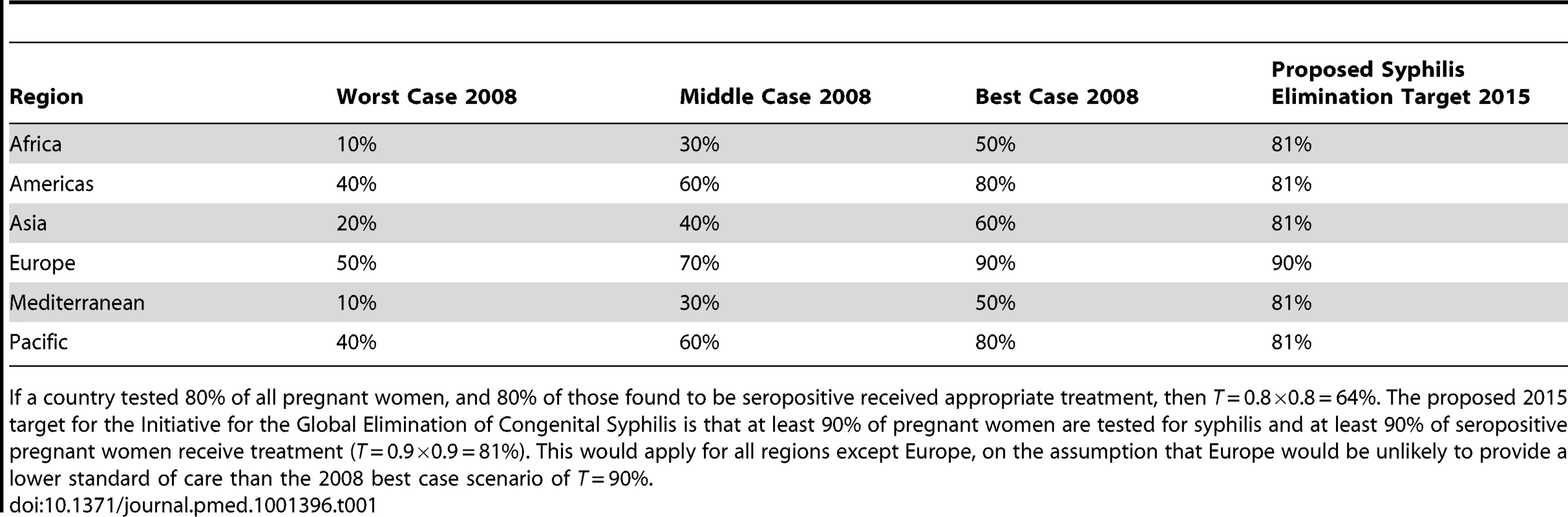
The objective of Step C was to estimate for each region the total number of adverse pregnancy outcomes related to maternal syphilis. We calculated the number of specific adverse pregnancy outcomes in five categories: any adverse outcome, stillbirth or early fetal death, neonatal death, prematurity or low birth weight, and an infected newborn. Because of the limited availability of data on the proportion of pregnant women tested in ANC and, of those found to be positive, the proportion treated adequately, we devised a simple sensitivity analysis that considered three testing and treatment coverage scenarios defined in consultation with WHO regional advisors: worst, middle, and best case (Table 1). In addition, we considered the scenario proposed as a target for 2015 in the WHO Initiative for the Global Elimination of Congenital Syphilis, in which at least 90% of pregnant women are tested for syphilis at first antenatal visit, and at least 90% of seropositive pregnant women are adequately treated (i.e., testing and treatment coverage T = 81% for all regions, except Europe, which was assumed to maintain T = 90%).
In Step C1, the total number of adverse outcomes in pregnant women with probable active syphilis who did not attend ANC was calculated as the product of the regional number of infected pregnant women not attending ANC and the proportion P of those women expected to have a syphilis-related adverse outcome without treatment. P for each adverse outcome category was obtained from a meta-analysis of published clinical literature assessing adverse pregnancy outcomes among women with probable active syphilis without adequate treatment: Pany adverse outcome = 0.52, Pstillbirth/early fetal death = 0.21, Pneonatal death = 0.09, Pprematurity/low birth weight = 0.06, and Pinfected newborn = 0.16 [22].
We also estimated the number of adverse outcomes in pregnant women with probable active syphilis who attended ANC (Step C2 and Step C3). Not all women who attend ANC are tested for syphilis and adequately treated if seropositive. Therefore, we estimated adverse outcomes for women who were both tested and treated (T) (Table 1), as well as for those who were not (1−T). In women who are not both tested and treated, the number of adverse outcomes is the number not tested and treated multiplied by the proportion expected to have an adverse outcome (P). Even among women who are both tested and treated, a small number of adverse events can be expected, particularly if syphilis cases are identified late in pregnancy. A systematic review by Blencowe et al. found that the effectiveness E of screening and treatment with penicillin in reducing adverse outcomes was as follows: Eneonatal death = 0.80, Eprematurity/low birth weight = 0.64, and Einfected newborn = 0.97 [23]. For this analysis, Estillbirth/early fetal death = 0.82 was based on the estimate of effectiveness for stillbirth alone, and Eany adverse outcome = 0.84 was based on the weighted mean of Eneonatal death, Eprematurity/low birth weight, Einfected newborn, and Estillbirth/early fetal death, using as weights the proportion of women with the corresponding adverse outcome.
Step D: Estimate the Global Number of Adverse Pregnancy Outcomes Related to Syphilis
Step D summed the regional estimates for each adverse outcome to produce a global estimate of the number of adverse pregnancy outcomes related to syphilis.
Finally, we calculated the number of adverse pregnancy outcomes averted by current services by subtracting the number of adverse outcomes in the middle case testing-and-treatment-coverage scenario from a baseline number of adverse outcomes estimated in the absence of any services.
Results
We estimated that in 2008 there were 1,360,485 (range 1,160,195–1,560,776) pregnant women with probable active syphilis infections, and of these women, 1,085,637 (79.8%) attended ANC. The estimated number of infected pregnant women by region was 535,203 in Africa (39.3%), 106,500 in the Americas (7.8%), 603,293 in Asia (44.3%), 21,602 in Europe (1.6%), 40,062 in the Mediterranean (3.0%), and 53,825 (4.0%) in the Pacific. Without any screening or treatment services, these pregnant women with probable active syphilis would have had 707,452 adverse pregnancy outcomes, including 285,702 stillbirths or early fetal deaths, 122,444 neonatal deaths, 81,629 premature or low birth weight infants, and 217,678 infected newborns. Thus, in the absence of any antenatal syphilis screening and treatment, an estimated 408,146 fetal or perinatal deaths and 299,307 infants at risk for early death would have resulted from maternal syphilis infection.
Figure 3 shows the estimated number of adverse outcomes in 2008 associated with syphilis globally and by region for the worst, middle, and best case scenarios of testing and treatment of women who are seropositive. Considering the middle case scenario, we estimated that globally there were 520,905 (best: 425,847; worst: 615,963) adverse outcomes associated with syphilis in pregnancy, which included 212,327 (best: 174,938; worst: 249,716) stillbirths or early fetal deaths, 91,764 (best: 76,141; worst: 107,397) neonatal deaths, 65,267 (best: 56,929; worst: 73,605) preterm or low birth weight infants, and 151,547 (best: 117,848; worst 185,245) infected newborns. In summary, globally in 2008 in a middle case scenario, untreated maternal syphilis resulted in approximately 304,091 fetal or perinatal deaths and 216,814 syphilis-infected infants at risk for early death. Examination of any adverse outcome by region showed that the majority of adverse outcomes (87%) were in Africa and Asia. Of note, 66% of all adverse outcomes occurred in women who had attended ANC.
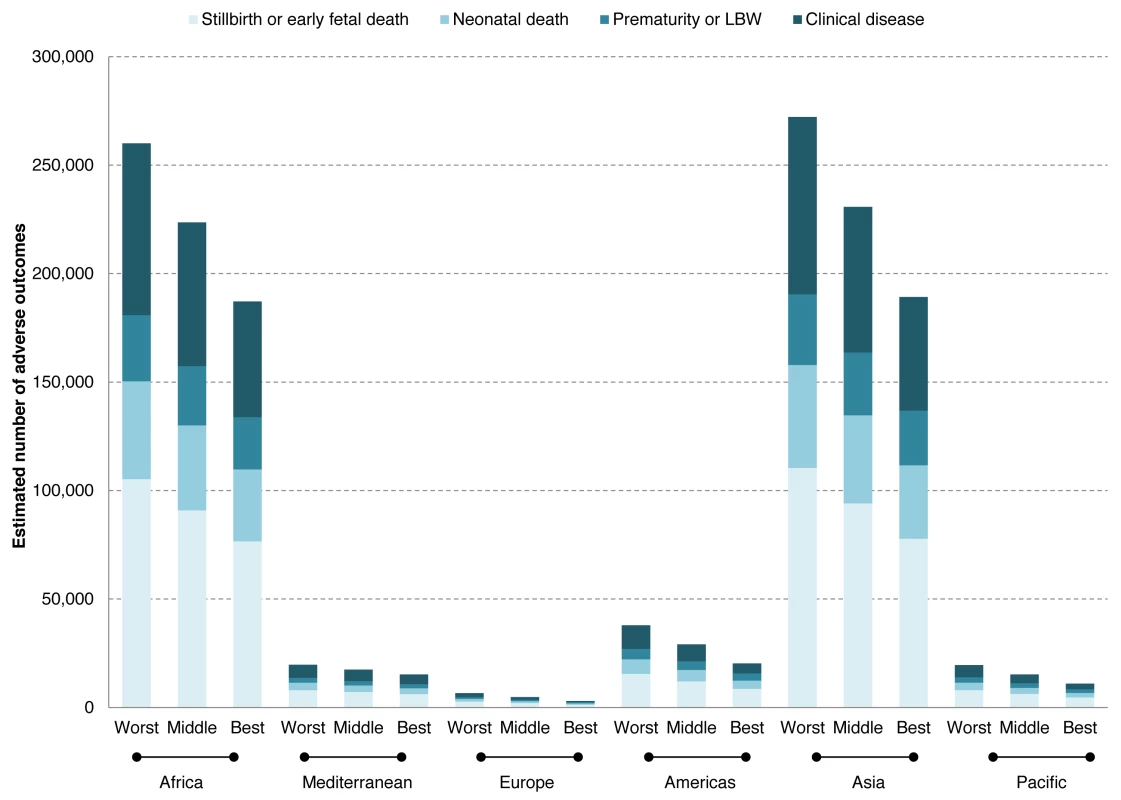
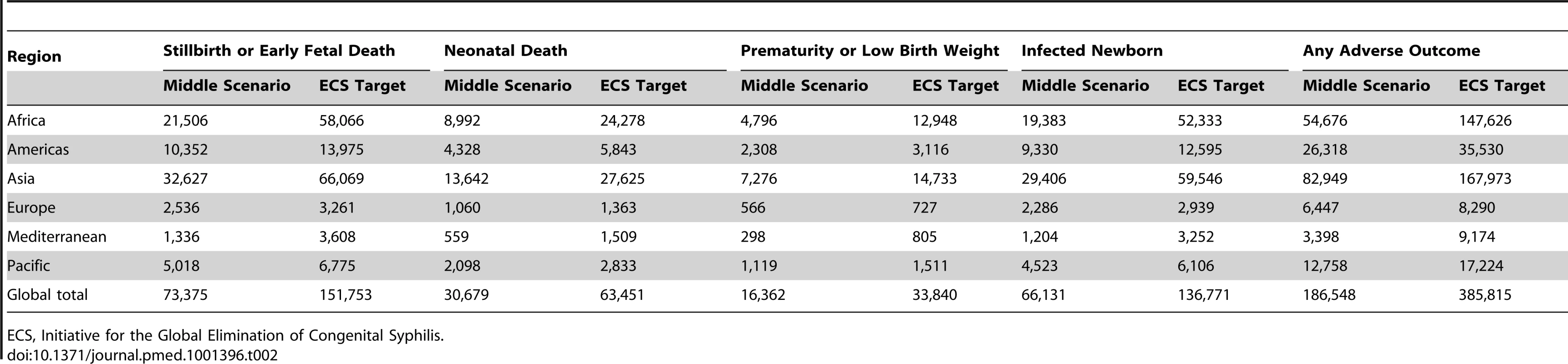
In 2008, using the middle case scenario for antenatal screening and treatment, approximately 186,548 (26%) of all adverse outcomes of syphilis in pregnancy were averted. Specifically, the averted outcomes were 73,375 stillbirths or early fetal deaths, 30,679 neonatal deaths, 16,362 preterm or low birth weight infants, and 66,131 infected newborns (Table 2). By region, the number of all adverse outcomes averted in 2008 in the middle case scenario was estimated as 54,676 in Africa, 26,318 in the Americas, 82,949 in Asia, 6,447 in Europe, 3,398 in the Mediterranean, and 12,758 in the Pacific. If the elimination initiative targets for 2015 of at least 90% testing and 90% treatment had been reached in 2008, then 385,815 (55%) of all adverse outcomes could have been averted: 151,753 stillbirths or early fetal deaths, 63,451 neonatal deaths, 33,840 preterm or low birth weight infants, and 136,771 infected newborns.
Discussion
Globally, nearly 1.4 million pregnant women in 2008 had probable active syphilis infection and were at risk of transmitting the disease perinatally to their unborn children. This is lower than previously reported 1997–2003 WHO estimates of approximately 2 million pregnant women annually with untreated syphilis infection, and suggests some progress may have been made over the past decade in syphilis prevention and control. However, the extent of progress is difficult to determine, as the estimates used differing methodological approaches. In comparison to the 1997–2003 estimates, the 2008 estimates were intended to take into account existing treatment services, remove background mortality and morbidity unrelated to syphilis, and better account for the anticipated increasing availability of testing and treatment over time. In addition, because of the paucity of published cross-sectional survey data since 2003 on syphilis in pregnancy, the 2008 estimates were based on data reported to WHO routinely by countries through the HIV Universal Access reporting system rather than on data from a literature review.
Despite differences in methodology, both the 1997–2003 and the 2008 estimates indicate that syphilis in pregnancy continues to be an important cause of mortality and morbidity in pregnancy. This is unsettling given the fact that universal syphilis screening in ANC and prompt treatment of women testing positive are basic interventions that have been proven to be cost-effective even in low prevalence settings. Additionally, rapid point-of-care syphilis tests allowing testing and treatment in almost any clinical setting were not widely available in 2003, but certainly should have been by 2008. These 2008 estimates support that countries in every region of the world should scale up screening and treatment for syphilis in pregnancy, and that doing so could substantially reduce preventable perinatal death and disability.
Our estimates suggest that over 520,000 adverse pregnancy outcomes due to syphilis occurred in 2008, of which approximately 215,000 were stillbirths or early fetal deaths, 90,000 were neonatal deaths, 65,000 were premature or low birth weight infants, and another 150,000 were infected newborns. Our estimates do not include additional deaths that would be expected to occur after the first month of life due to prematurity, low birth weight, or congenital infections, estimated in one study to result in approximately 10% mortality by 1 y (i.e., approximately 21,500 additional infant deaths) [24].
Approximately one-fifth (20%) of all pregnant women with syphilis did not attend ANC. Thus, efforts to ensure universal access to early ANC are fundamental in eliminating congenital syphilis, as well as other causes of preventable infant mortality. But importantly, our data suggest that two-thirds of the adverse outcomes due to syphilis occurred in women who had attended ANC at least once, but either were not screened or, if they were screened and tested positive, did not receive appropriate treatment with intramuscular benzathine penicillin. The vast majority of outcomes that occurred in 2008 could have been prevented had the women received quality early ANC that included syphilis testing and access to effective therapies, as recommended by WHO. Syphilis testing and treatment are relatively inexpensive compared with other interventions, with tests typically costing less than US$1, and treatment slightly less than that. To reduce cases of congenital syphilis, it will be important to incorporate syphilis testing and treatment into routine procurement and distribution systems to ensure that pregnant women receive an essential minimal package of ANC interventions.
Existing health care services were able to avert one out of every four expected adverse outcomes in 2008. However, if the proposed testing and treatment targets for 2015 outlined in the Initiative for the Global Elimination of Congenital Syphilis had been reached in 2008, over half of all expected adverse outcomes could have been averted. Further research is needed to define how many cases and what level of service delivery is needed to attain the ultimate goal of “elimination of congenital syphilis as a public health problem.” However, given that screening and treatment for preventing MTCT of syphilis is not 100% effective, primary prevention of syphilis in pregnant women is also an important strategy that needs to be addressed to truly eliminate congenital syphilis.
While substantial progress has been made in the utilization of ANC (in 2009 WHO estimated that approximately 81% of all pregnant women had attended at least one ANC visit) [25], congenital syphilis still occurred for a variety of reasons: many of these visits were too late to avert an adverse outcome, clinics may not have offered testing, testing may not have been affordable, women may not have followed up or received their test results, treatment may not have been available, or treated women may have been reinfected by untreated sexual partners [26].
Our estimates are subject to some limitations. First, there are no global data on estimated numbers of early fetal deaths; national estimates of early fetal deaths had to be crudely extrapolated from estimated numbers of stillbirths using a correction factor based mainly on data from high-income countries. Improved data on early fetal death, in particular in low- and middle-income countries, is necessary to understand the full extent of the impact of this limitation.
In addition, these estimates rely on data reported through the HIV Universal Access reporting system and do not include separate published studies of syphilis seropositivity, as was previously done for the 1997–2003 estimates. The advantage of HIV Universal Access data is that they are reported by most developing countries on a routine basis, involve a larger sample size than most published studies, and are less subject to a publication bias. However, several countries did not report through the HIV Universal Access system, including some high-income countries in North America, Europe, and the Mediterranean with low syphilis seropositivity, as well as some particularly low resource countries without organized screening programs and with high syphilis seropositivity. It is unclear how this underreporting would affect the overall estimates.
Although countries are asked to report nationally representative data, it is possible that these data are over-representative of urban populations with greater access to syphilis prevention and treatment services than rural populations. If syphilis seropositivity is higher in rural settings (and programs are less effective), our calculations may underestimate the true burden of syphilis-associated adverse outcomes.
In addition, HIV Universal Access data do not include information on testing methodologies, test titer, stage of disease, or treatment history, and therefore it is unclear whether or not a country's data includes women with latent or previously treated disease. This analysis applied a correction factor for “probable active” disease to the entire dataset to account for this; however, adjustment may not have been necessary in all cases and may have led to underestimation of the true burden of active disease.
Because of a lack of representative data on current testing and treatment coverage, these estimates relied on expert opinion of current testing and treatment coverage, and the experts may have miscalculated. In order to explore the validity of these estimates, we present a basic sensitivity analysis of testing and treatment coverage to account for the uncertainty related to this approximation. Although WHO is working to improve collection of data on syphilis testing and treatment through the HIV Universal Access reporting system, these testing and treatment data are not yet felt to be accurate and representative at a global level (the highest performing countries are more likely to report service delivery indicators). Thus, more work with countries to strengthen surveillance and monitoring systems is needed.
Finally, these estimates do not account for the timing of treatment of syphilis in pregnancy. Although syphilis transmission has been documented to occur very early in pregnancy, existing data suggest that catastrophic outcomes due to syphilis require development of the fetal immune system (i.e., after 18–20 wk gestation) [27]. It is also recognized that the effectiveness of screening and treatment is lower in the third trimester than in the first and second trimesters [28].
The limitations of these estimates highlight the urgent need for improved data through stronger national surveillance and monitoring systems. All countries should know at least the three core indicators related to MTCT of syphilis in their population: what proportion of ANC attendees are tested for syphilis, what proportion are seropositive, and what proportion of syphilis seropositive ANC attendees are adequately treated [29]. WHO hopes to work with countries to improve capacity to monitor and report on these three core indicators through the WHO HIV Universal Access reporting system. Better national data are also needed on how early pregnant women seek care and how many women have early fetal deaths, as well as how estimates of adverse outcomes such as congenital syphilis and stillbirth attributable to syphilis compare to actual reported cases of congenital syphilis and stillbirth attributable to syphilis.
In summary, this analysis indicates that syphilis continues to be an important cause of adverse outcomes of pregnancy, including substantial numbers of perinatal deaths and disabilities. Given that an increasing proportion of the infant mortality that Millennium Development Goal 4 aims to address by 2015 occurs during the first month of life, investing in elimination of MTCT of syphilis is a low-hanging fruit for reducing neonatal mortality, as well as stillbirths. Primary prevention of syphilis in people of reproductive age is an important first step towards reducing these deaths. Better data are needed to raise local awareness of the burden of syphilis in pregnancy, an old scourge that is often overlooked in modern day public health programs. Countries also need to ensure that quality-assured syphilis testing is available in all ANC settings, now possible even in remote care settings with the introduction of rapid point-of-care diagnostics. In addition, efforts are needed to ensure universal access to early ANC, as well as improved quality of ANC, so that all pregnant women receive an essential package of services that includes routine and early access to point-of-care testing and adequate treatment for syphilis if seropositive. MTCT of syphilis can only be eliminated if decision-makers at all levels prioritize the provision and quality of this basic ANC service.
Elimination of MTCT of syphilis directly supports attainment of Millennium Development Goals 4, 5, and 6 through reduction in infant mortality, improved maternal health, and primary prevention of HIV [30]. With just a short amount of time left to achieve the Millennium Development Goals, the United Nations Secretary-General launched the Global Strategy for Women's and Children's Health, which calls for improved coordination around maternal and newborn health issues [31]. Bringing ministries of health and partners together to provide universal coverage of antenatal syphilis screening and to ensure treatment of all pregnant women infected with syphilis is a specific example of an activity that would greatly support the Global Strategy for Women's and Children's Health.
Supporting Information
Zdroje
1. RothschildBM (2005) The history of syphilis. Clin Infect Dis 40: 1454–1463.
2. CrosbyAWJr (1969) The early history of syphilis: a reappraisal. Am Anthropol 2: 218–227.
3. HawkesS, MatinN, BroutetN, LowN (2011) Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 11: 684–691.
4. World Health Organization (2007) The global elimination of congenital syphilis: rationale and strategy for action. Geneva: World Health Organization. Available: http://www.who.int/reproductivehealth/publications/rtis/9789241595858/en/index.html. Accessed 17 January 2013.
5. World Health Organization (2011) Progress report 2011: Global HIV/AIDS response. Geneva, Switzerland. Available: http://www.who.int/hiv/pub/progress_report2011/en/index.html. Accessed 17 January 2013.
6. MabeyDC, SollisKA, KellyHA, BenzakenAS, BitarakwateE, et al. (2012) Point-of-care tests to strengthen health systems and save newborn lives: the case of syphilis. PLoS Med 9: e1001233 doi:10.1371/journal.pmed.1001233
7. YangLG, TuckerJD, WangC, ShenSY, ChenXS, et al. (2011) Syphilis test availability and uptake at medical facilities in southern China. Bull World Health Organ 89: 798–805.
8. Dinh TH, Lewis D, Trege L, Likibi M, Molebatsi T, et al.. (2008) Prevalence of and adherence to HIV prophylaxis and syphilis treatment regimens in pregnant women receiving antenatal care services in public facilities in Northern Cape and Gauteng Provinces, South Africa, 2004–2006 [poster presentation]. HIV/AIDS Implementers' Meeting; 3–7 June 2008; Kampala, Uganda.
9. Pan American Health Organization (2010) Regional initiative for the elimination of vertical transmission of HIV and congenital syphilis in Latin America and the Caribbean: regional monitoring strategy. Available: http://new.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=6944&Itemid=. Accessed 17 January 2013.
10. Joint United Nations Programme on HIV/AIDS, United Nations Children's Fund, United Nations Population Fund, World Health Organization (2011) Elimination of new paediatric HIV infections and congenital syphilis in Asia-Pacific, 2011–2015: conceptual framework; monitoring and evaluation guide. Available: http://www.eptctasiapacific.org/documents/cs-framework_0.pdf. Accessed 17 January 2013.
11. SchmidG, StonerBP, HawkesS, BroutetN (2007) The need and plan for global elimination of congenital syphilis. Sex Transm Dis 34: S5–S10.
12. World Health Organization (2013) About WHO: WHO—its people and offices. Available: http://www.who.int/about/structure/en/index.html. Accessed 17 January 2013.
13. World Health Organization (1993) International statistical classification of diseases and related health problems: tenth revision, volume 2. Instruction manual. Geneva: World Health Organization.
14. CousensS, BlencoweH, StantonC, ChouD, AhmedS, et al. (2011) National, regional, and worldwide estimates of stillbirth rates in 2009 with trends since 1995: a systematic analysis. Lancet 377: 1219–1330.
15. LawnJ, BlencoweH, PattinsonR, CousensS, KumarR, et al. (2011) Stillbirths: Where? When? Why? How to make the data count? Lancet 377: 1448–1463.
16. FlenadyV, KoopmansL, MiddletonP, FrøenF, SmithG, et al. (2011) Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet 377: 1331–1340.
17. World Health Organization (2012) Global incidence and prevalence of selected curable sexually transmitted infections—2008. Available: http://www.who.int/reproductivehealth/publications/rtis/stisestimates/en/index.html. Accessed 17 January 2013.
18. LujanJ, Arrazola de OnateW, DelvaW, ClaeysP, SambolaF, et al. (2008) Prevalence of sexually transmitted infections in women attending antenatal care in Tete province, Mozambique. S Afr Med J 98: 49–51.
19. TinajerosF, GrossmanD, RichmondK, SteeleM, GarciaSG, et al. (2006) Diagnostic accuracy of a point-of-care syphilis test when used among pregnant women in Bolivia. Sex Transm Infect 82: 17–21.
20. Watson-JonesD, ChangaluchaJ, GumodokaB, WeissH, RusizokaM, et al. (2002) Syphilis in pregnancy in Tanzania. I. Impact of maternal syphilis on outcome of pregnancy. J Infect Dis 186: 940–947.
21. World Health Organization (2013) Global Health Observatory Data Repository: antenatal care coverage. Available: World Health Statistics Health inequities Antenatal care coverage. Accessed 17 January 2013.
22. GomezGB, KambML, NewmanLM, MarkJ, BroutetN, et al. (2012) Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ E-pub ahead of print. Article ID: BLT.12.107623.
23. BlencoweH, CousensS, KambM, BermanS, LawnJE (2011) Lives Saved Tool supplement detection and treatment of syphilis in pregnancy to reduce syphilis related stillbirths and neonatal mortality. BMC Public Health 11 Suppl 3 S9.
24. McDermottJ, SteketeeR, LarsenS, WirimaJ (1993) Syphilis-associated perinatal and infant mortality in rural Malawi. Bull World Health Organ 71: 773–780.
25. World Health Organization (2013) Global Health Observatory: antenatal care—situation. Available: http://www.who.int/gho/maternal_health/reproductive_health/antenatal_care_text/en/index.html. Accessed 17 January 2013.
26. KambML, NewmanLM, RileyPI, MarkJ, HawkesSJ, et al. (2010) A road map for the global elimination of congenital syphilis. Obstet Gynecol Int 2010: 312798.
27. BermanSM (2004) Maternal syphilis: pathophysiology and treatment. Bull World Health Organ 82: 433–438.
28. HawkesS, GomezG, BroutetN (2013) Early antenatal care: does it make a difference to outcomes of pregnancy associated with syphilis? A systematic review and meta-analysis. PLoS ONE In press.
29. World Health Organization (2011) Methods for surveillance and monitoring of congenital syphilis elimination within existing systems. Available: http://www.who.int/reproductivehealth/publications/rtis/9789241503020/en/index.html. Accessed 17 January 2013.
30. MwapasaV, RogersonSJ, KwiekJJ, WilsonPE, MilnerD, et al. (2006) Maternal syphilis infection is associated with increased risk of mother-to-child transmission of HIV in Malawi. AIDS 20: 1869–1877.
31. United Nations Secretary-General Ban Ki-moon (2010) Global strategy for women's and children's health. Available: http://www.everywomaneverychild.org/images/content/files/global_strategy/full/20100914_gswch_en.pdf. Accessed 17 January 2013.
Štítky
Interné lekárstvoČlánok vyšiel v časopise
PLOS Medicine
2013 Číslo 2
- MUDr. Lenka Klimešová: Multiodborová vizita je kľúč k efektívnejšej perioperačnej liečbe chronickej bolesti
- Realita liečby bolesti v paliatívnej starostlivosti v Nemecku
- Statiny indukovaná myopatie: Jak na diferenciální diagnostiku?
- Nech brouka žít… Ať žije astma!
- Co dělat při intoleranci statinů?
Najčítanejšie v tomto čísle
- Prognosis Research Strategy (PROGRESS) 3: Prognostic Model Research
- Prognosis Research Strategy (PROGRESS) 2: Prognostic Factor Research
- Whole Genome Sequencing versus Traditional Genotyping for Investigation of a Outbreak: A Longitudinal Molecular Epidemiological Study
- Prevalence of Age-Related Macular Degeneration in Nakuru, Kenya: A Cross-Sectional Population-Based Study
