Profile of Cancer Patients Treated at the Emergency Room of a Tertiary Cancer Care Centre in Southern Brazil
Profil pacientů s nádory léčených na pohotovosti referenčního střediska nádorové péče v jižní Brazílii
Počet návštěv onkologických pacientů na pohotovosti za účelem vyšetření a léčby se neustále zvyšuje. Pacienti s nádorovým onemocněním představují výzvu pro pohotovostní tým, protože mohou mít akutní příznaky ještě nediagnostikované malignity, neurčité příznaky související s onemocněním nebo s komplikacemi způsobené léčbou, z nichž některé mohou být mírné nebo potenciálně život ohrožující. Nemocnice San Antonio je veřejná instituce nacházející se ve městě Blumenau (SC, jižní Brazílie), která funguje jako referenční centrum pro pacienty s rakovinou a poskytuje péči pro více než milion a půl lidí. Cílem tohoto výzkumu je popsat epidemiologický profil onkologické populace, která navštívila pohotovost této nemocnice za dobu více než 6 měsíců, počínaje 1. dubnem 2011 a konče 31. říjnem 2011. Pohotovost navštívilo celkem 1 051 onkologických pacientů ve věku od 19 do 89 let. Nejčastěji vyhledávali péči pacienti s urologickými nádory, nádory prsu, horního a dolního gastrointestinálního traktu a nádory plic. Třemi nejčastějšími stížnostmi byly bolest, respirační symptomy a gastrointestinální symptomy. Návštěvy byly nejvíce zaznamenány během dne a hlavně v pondělí a úterý. Zlepšení primární péče a efektivity na onkologických klinikách je velice důležité zejména pro uspokojení vysoké poptávky po návštěvách, aby se tak zabránilo zbytečným návštěvám na oddělení pohotovosti.
Klíčová slova:
záchranná služba – statistika a číselné údaje – zdravotnictví – nádory – komplikace – terapie – bolest – příjem pacientů
Authors:
R. Kraft Rovere; C. Dagnoni; Gomes Corrêa C. E.; Dias De Oliveira E.; F. C. Figueira; J. Sapelli
Authors‘ workplace:
Department of Oncology, Santo Antonio Hospital, Blumenau, Santa Catarina, Brazil
Published in:
Klin Onkol 2012; 25(6): 452-456
Category:
Original Articles
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do bi omedicínských časopisů.
Obdrženo: 14. 5. 2012
Přijato: 31. 5. 2012
Overview
The number of cancer care visits in the emergency department for evaluation and treatment has been steadily increasing. Cancer patients represent a challenge for the emergency team because they may have acute symptoms of still undiagnosed malignancy, vague symptoms related to the disease or complications of cancer treatment, all of which can be either mild or potentially life-threatening. The Santo Antonio Hospital is a public institution located in the city of Blumenau (SC, southern Brazil), which serves as a reference centre for cancer care patients for a population of over a million and a half. The objective of this research was to describe the epidemiological profile of the oncologic population who were treated at the emergency department of this hospital, during a period of over six months, starting on April 1st , 2011 to October 31st of the same year. There were 1,051 oncologic visits during this period, with the age ranging from 19 to 89 years. The greater demand for care was sought by patients with urological, breast, upper and lower gastrointestinal tract and lung cancer. The three major complaints of the consultations were pain, respiratory and gastrointestinal symptoms. The visits occurred mainly during daytime mostly on Mondays and Tuesdays. The improvement of primary care services and efficiency of oncology clinics in meeting the high demand for appointments is extremely important, in order to prevent unnecessary visits to the emergency department.
Key words:
emergency service – statistics & numerical data – health services – neoplasms – complications – therapy – pain – patient admission
Introduction
The number of cancer patients presenting to the emergency department for evaluation and treatment has increased. There are several possible reasons for this fact. As the population grows old, the prevalence of cancer increase naturally [1]. In addition, the survival of cancer patients has dramatically increased since the early 1900 due to new treatment strategies [2–4]. Finally, recent treatments include more aggressive therapies, which correspond to more patients experiencing treatment-related side effects [5–7].
Cancer patients represent a challenge for the emergency team because they may have acute symptoms of undiagnosed malignancy, vague symptoms related to the disease or complications of cancer treatment. Although cancer is a chronic disease, acute problems such as pain, nausea, vomiting, fever, leukopenia and electrolyte disturbance may result in a visit to the emergency room [8]. Many oncologic emergencies related to the malignant process, such as spinal cord compression, gastrointestinal bleeding and airway obstruction, are usually managed at the emergency department [2].
The Santo Antonio Hospital is a public institution located in the city of Blumenau (State of Santa Catarina, Southern Brazil), which acts as a reference center for the National Brazilian Health System in the care of cancer patients to the region of Itajaí’s Middle Valley. Thus, the objective of this research was to describe the epidemiological profile of the oncologic population who come tothe emergency department of this hospital.
Patients and Methods
This research was conducted at St. Antonio Hospital, located in the city of Blumenau (SC), using information from the statistical service and electronic medical files.
To collect the data, a survey was performed electronically in all patients enrolled in the oncology outpatient setting of St. Antonio Hospital who sought the emergency room of the same hospital during the period spanning from the April 1st, 2011 to October 31st of the same year.
The studied population was composed of patients with a previous diagnosis of malignancy, seen in the emergency room of St. Antonio Hospital in the period described above.
Considering all the patients either in active treatment or follow up, we gathered more than 1,500 opened files (i.e. still alive during the timespan of our research).
Only adult patients were considered meaning we included only patients over 16 into this study. Patients without cancer diagnosis were excluded as well.
Only primary cancer was recorded, eventual metastases or secondary cancers were not reported.
The investigated study variables were sociodemographic, based on information reported in medical records: gender, age, reason for consultation, type of cancer, day of week, time, and if the visit resulted in hospital admission or discharge.
Gender was divided into male and female, and age was grouped into four different subtypes: 16–40, 41–60, 61–80 and above 80 years old.
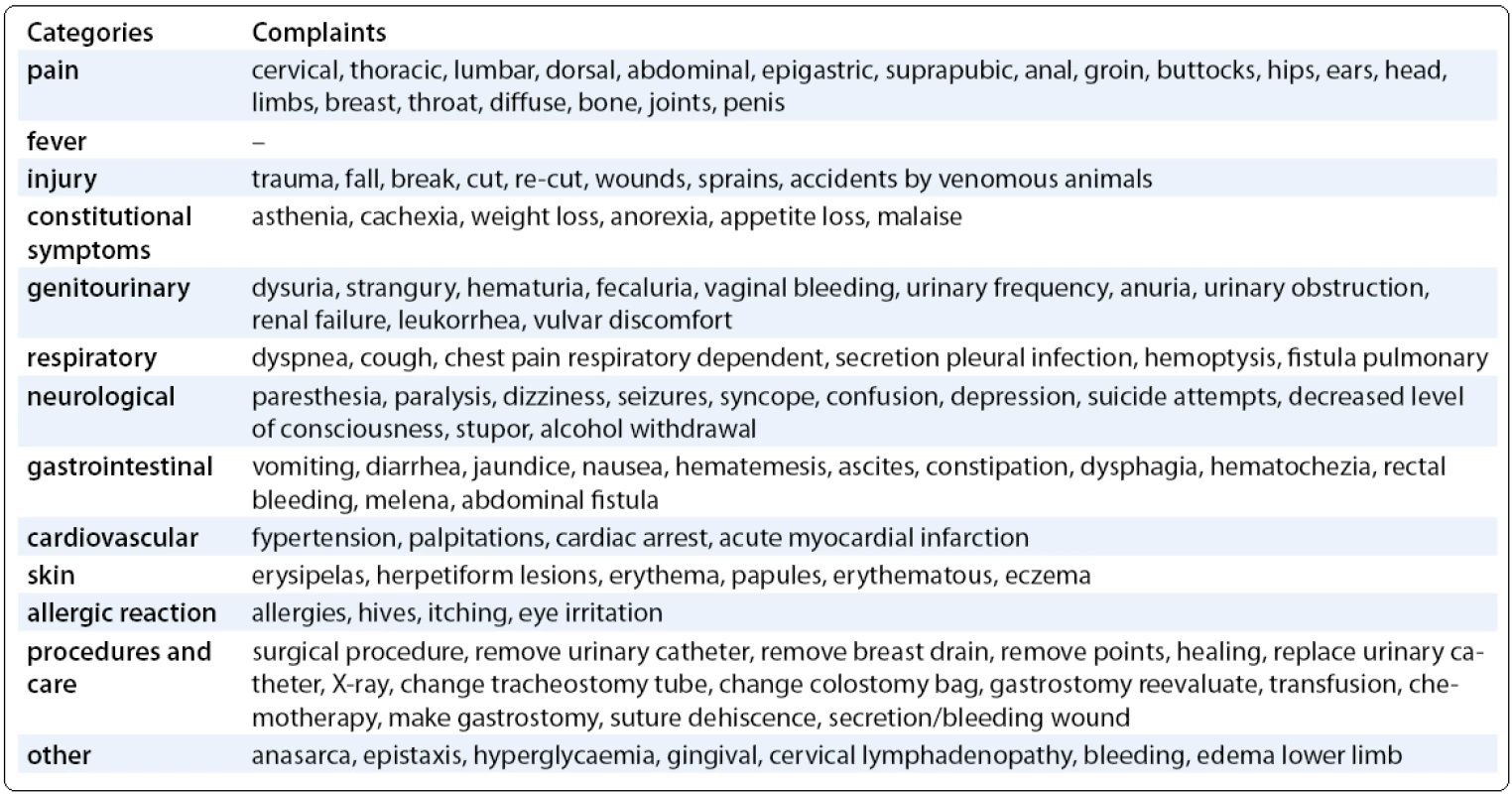
The reasons for the visit were divided into large groups: pain, fever, external injury, constitutional symptoms, genitourinary, respiratory, neurological, gastrointestinal, cardiovascular, skin, allergic reaction, procedures and care and other (Tab. 1).
The type of cancer was separated in categories: head and neck (mouth, pharynx and larynx), gynecological (endometrial, cervical and ovarian cancer), breast, lung, urological (prostate, kidney, testicular and bladder), lower gastrointestinal tract (colon, sigmoid colon, rectum, anal canal), upper gastrointestinal tract (esophagus, stomach, pancreas and liver), hematologic (leukemia and lymphoma), skin (melanoma and non--melanoma) and other (brain, sarcoma, unknown site and other).
The days of the week ranged from Monday to Sunday.
The time was divided into two major groups: daytime (07.00 to 18.59) or nighttime (19.00 to 06.59).
Visits were defined based on results – either hospital admission or discharge.
The study protocol was reviewed and approved by the Ethics Committee in Research of the Hospital Foundation in Blumenau.
This study ensures total privacy of data collected from medical records of patients.
Results
Between the period of April 1st, 2011 to October 31st, 2011, there were 2,036 visits to the emergency department of St. Antonio Hospital from patients linked to the oncology clinic. Of these, 1,051 were cancer patients and therefore included in the study. Of all patients included, 283 were female and 269 male. Thus, the average consultation was 1.9 per patient.
Ages ranged from 19 years to 89 years. Most women (48.76%) were between 41 to 60 years and most men (48.33%) were aged 61 to 80 years (Fig. 1).
The most frequent types of cancers of all visits in the emergency department, during the analysed period, were urological (148 visits – 14%), breast (146 visits – 13.9%) and upper gastrointestinal tract (145 visits – 13, 8%) (Fig. 2).

The majority of care occurred on Monday (173 visits – 16.5%) and Tuesday (168 attendances – 16%), both during the day. Sunday was the least busy day concerning the number of oncologic visits (110 visits – 10.5%) (Fig. 3).

Regarding major complaints, pain was naturally the symptom that led to more visits to the emergency department, totaling 39.2%. In addition to pain symptoms, respiratory symptoms (13.42%), gastrointestinal (11.7%) and constitutional (9%) symptoms had significant rate (Fig. 4). When stratifying by tumor sites symptoms: pain was the most common complaint of head and neck, gynecological, breast, urologic, low and high gastrointestinal tract, hematological, skin and others cancers. On the other hand, respiratory symptoms only prevailed in lung cancers.

Only a third of the visits resulted in hospitalization (30.54%). Majority of visits (69.46%) ended with release of the patient.
Discussion
This study examined the oncologic population treated at the emergency room of St. Antonio Hospital in Blumenau, over a period of six months, running from April 1st, 2011 to October 31st, 2011. Exactly 1,051 oncologic visits were analysed in the emergency department during this period, with many patients seeking assistance more than once, resulting in an average of 1.9 visits per patient. A similar phenomenon was demonstrated in the study of Mayer et al [8], where the average was 1.4 visits per patient. Most care was given to women.
The age ranged from 19 to 89 years. The age group most prevalent among women was 41 to 60 years, whereas among men it was higher, 61 to 80 years. In Yates and Barrett [3] study, as well as in Mayer et al [8], the average age was 65 years. In a publication of Swenson et al [2], this value was 68.9 years and in Porta et al [9] it was 67.7 years. These data reflect an aging population that can get more and better therapeutic possibilities, not only in cancer but also other comorbidities such as cardiovascular increasing overall survival [10].
Tumor categories were stratified according to the types of cancers that treated patients during the stated period presented. The greater demand for care was noted (in decreasing order) for patients with urological, breast, upper and lower gastrointestinal tract and lung cancer, with nearly two thirds of patients. This profile was similar to that presented in the research of Mayer et al [8], where the most common diagnoses were lung, colorectal, breast and prostate cancer, as well as in Yates and Barrett [3] where prevailed lung, bowel, breast, prostate and esophagus cancer. Also, Yucel et al [11] reported the most common primary cancer sites were the thorax, the gastrointestinal system and the genitourinary system.
The three major complaints of the consultations were in descending order: pain, respiratory and gastrointestinal symptoms, matching the study by Mayer et al [8]. In Swenson et al [2] study, patients admitted to the emergency room had symptoms related to terminal illness or with their own chemotherapy, such as pain, gastrointestinal symptoms, asthenia and dyspnea.
The visits included in this study occurred mainly during the day and the majority on Monday and Tuesday. Likewise, the majority of patients admitted to the emergency department in the study of Yates and Barrett [3] and Mayer et al [8] were during the day.
We have a multidisciplinary team with regular lectures to patients given on a weekly basis, and leaflets explaining the possible undesirable side effects of chemo and radiotherapy, stating precisely when the patient needs to go to the hospital (for example excessive bleeding or febrile neutropenia), or when the patients may seek his primary or family doctor (for instance for mild pain or nausea). Nevertheless, little success has been achieved, as most of the cancer patients chose to go directly to the tertiary cancer centre.
It is believed that many patients sought emergency rather than clinics for easier and faster access or even for concern of not receiving proper care in primary care centres, where primary doctors often feel that meeting cancer patients is out of their scope, even when easy solving simple problems are the issue. We estimate that at least 90% of patients come without any previous referral, and the remainder 10% are sent by their primary physician.
Reviewing our database, we also sought to answer a question about the real need of an emergency visit of the patient. The question might be complex, as the issue is subjective, given different settings. As this is a retrospective study, the individuals classified as having acute symptoms of pain, for example, could have been either affected with mild or excruciating acute pain. Also, the reference primary doctor centre also differs; from nearby minor hospitals to much less structured health centres. Nevertheless, reanalysing the charts, we estimate that a minimum of 50% of patients’ visits to the hospital were unnecessary and could have been solved by the primary doctor or planned consultation, reducing the burden of both the emergency and oncology teams.
We have also found another interesting piece of data – over 80% of patients seeking the emergency room were patients in active treatment (chemotherapy in about 80% of cases and the remainder in hormone or targeted therapy) and that almost 90% of these patients had advanced disease. This specific data reflects directly the fact that more and more cancer patients live longer, hence are in constant need of medical care.
More than two thirds of visits were completed with the discharge of the patient, unlike what was reported in Mayer et al [8]. This evidence strengthens our opinion that many emergency visits could have been avoided if patients could solve their problems in routine oncology consultation or better care in the respective central health units for the designated areas of where the patient lives according to our national health system, in which people are allocated to a primary family doctor and his reference unit.
It is easily explainable given the fact that many of the visits to the emergency department were related to symptoms poorly managed in the primary care, such as pain, respiratory, gastrointestinal and constitutional symptoms, many of them are inherent in the natural disease history. Even other reasons – such as those cited in injury and procedures and care, for example – that made the patient seek emergency room, could be resolved in the outpatient clinic and thus reduce the burden of unnecessary consultations in the emergency room, improving their quality of assistance.
Limitations of this study are patients selection, many of whom may have obtained their first cancer diagnosis in the emergency department and therefore were not included in the study because they were not yet registered in the outpatient oncology setting. Moreover, given the retrospective nature of the survey, data may be missing or not properly filled in the electronic charts.
Due to the increasing prevalence and incidence of cancer in the general population as previously explained, it is crucial to understand the proper management of cancer patients by emergency physicians, especially in a reference hospital for these patients. It is extremely important, also, to improve primary care services and efficiency of oncology clinics in meeting the high demand for appointments, preventing unnecessary visits to the emergency department and burnout of medical teams.
Another point of interest is that, in many studies performed in different hospitals and countries, the results have not shown discrepant results, meaning that our survey comprising over a thousand consultations has produced significant data which may be extrapolated to other tertiary cancer centres, giving more weight to our work.
Rodrigo Kraft Rovere, MD
Department of Medical Oncology
Santo Antonio Hospital
Santa Catarina, Blumenau
Brazil
e-mail: rodrigorovere@hotmail.com
Submitted: 14. 5. 2012
Accepted: 31. 5. 2012
Sources
1. Jemal A, Bray F, Center MM et al. Global cancer statistics. CA Cancer J Clin 2011; 61(2): 69–90.
2. Swenson KK, Rose MA, Ritz L et al. Recognition and evaluation of oncology-related symptoms in the emergency department. Ann Emerg Med 1995; 26(1): 12–17.
3. Yates M, Barrett A. Oncological emergency admissions to the Norfolk and Norwich University Hospital: an audit of current arrangements and patient satisfaction. Clin Oncol (R Coll Radiol) 2009; 21(3): 226–233.
4. Halfdanarson TR, Hogan WJ, Moynihan TJ. Oncologic emergencies: diagnosis and treatment. Mayo Clin Proc 2006; 81(6): 835–848.
5. Christman K, Muss HB, Case LD et al. Chemotherapy of metastatic breast cancer in the elderly. The Piedmont Oncology Association experience [see comment]. JAMA 1992; 268(1): 57–62.
6. Tomasello G, Chiesa MD, Buti S et al. Dose-dense chemotherapy in metastatic gastric cancer with a modified docetaxel-cisplatin-5-fluorouracil regimen. Tumori 2010; 96(1): 48–53.
7. Dalla Chiesa M, Tomasello G, Buti S et al. Sequential chemotherapy with dose-dense docetaxel, cisplatin, folinic acid and 5-fluorouracil (TCF-dd) followed by combination of oxaliplatin, folinic acid, 5-fluorouracil and irinotecan (COFFI) in metastatic gastric cancer: results of a phase II trial. Cancer Chemother Pharmacol 2011; 67(1): 41–48.
8. Mayer DK, Travers D, Wyss A et al. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 2011; 29(19): 2683–2688.
9. Porta M, Fernandez E, Belloc J et al. Emergency admission for cancer: a matter of survival? Br J Cancer 1998; 77(3): 477–484.
10. Hardoon SL, Whincup PH, Lennon LT et al. How much of the recent decline in the incidence of myocardial infarction in British men can be explained by changes in cardiovascular risk factors? Evidence from a prospective population-based study. Circulation 2008; 117(5): 598–604.
11. Yucel N, Sukru Erkal H, Sinem Akgun F et al. Characteristics of the admissions of cancer patients to emergency department. J BUON 2012; 17(1): 174–179.
Labels
Paediatric clinical oncology Surgery Clinical oncologyArticle was published in
Clinical Oncology

2012 Issue 6
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Spasmolytic Effect of Metamizole
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole in perioperative treatment in children under 14 years – results of a questionnaire survey from practice
- Metamizole vs. Tramadol in Postoperative Analgesia
-
All articles in this issue
- Liver Function Assessment in Oncology Practice
- EML4-ALK Fusion Gene in Patients with Lung Carcinoma: Biology, Diagnostics and Targeted Therapy
- Cost Analysis of XELOX and FOLFOX-4 Chemotherapy Regimens for Colorectal Carcinoma
- Therapeutic Results of the Treatment Brain Tumors Using Radiosurgery and Stereotactic Radiotherapy
- Proteins of Resistence and Drug Resistence in Ovarian Carcinoma Patients
- A Case Report: Patient with Advanced Ovarial Tumour and Supporting Care
- Paraneoplastic Neurological Syndrome in 64-year-old Patient in Association with a Small Cell Lung Carcinoma
- Molecular Basis of Waldenström Macroglobulinemia
- Why Mitochondria are Excellent Targets for Cancer Therapy
- Profile of Cancer Patients Treated at the Emergency Room of a Tertiary Cancer Care Centre in Southern Brazil
- Incidentally Discovered White Subcupsular Liver Nodules during Laparoscopic Surgery: Biliary Hamartoma and Peribiliary Gland Hamartoma
- Clinical Oncology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Liver Function Assessment in Oncology Practice
- Cost Analysis of XELOX and FOLFOX-4 Chemotherapy Regimens for Colorectal Carcinoma
- Incidentally Discovered White Subcupsular Liver Nodules during Laparoscopic Surgery: Biliary Hamartoma and Peribiliary Gland Hamartoma
- A Case Report: Patient with Advanced Ovarial Tumour and Supporting Care

