Posterior reversible encephalopathy syndrome associated with Neisseria elongata meningitis
Authors:
S. Eliacik 1; O. Akdogan 2; F. Uysal Tan
Authors‘ workplace:
Department of Neurology, School of, Medicine, Hitit University, Corum, Turkey
1; Department of Infectious Diseases and, Clinical Microbiology, School of Medicine, Hitit University, Corum, Turkey
2
Published in:
Cesk Slov Neurol N 2020; 83/116(5): 570-571
Category:
Letter to Editor
doi:
https://doi.org/10.14735/amcsnn2020570
Dear editor,
Posterior reversible encephalopathy syndrome (PRES) is a well-described clinical-radiological entity that refers to reversible subcortical vasogenic brain edema mostly affecting the posterior cerebral hemispheres [1]. The posterior predilection might be caused by relatively lower sympathetic vascular innervation of the region [2]. The association between infection and PRES is well recognised as the 3rd or the 4th common predisposing factor, but PRES related to meningitis is extremely rare [2,3]. We present a case of PRES associated with Neisseria elongata meningitis.
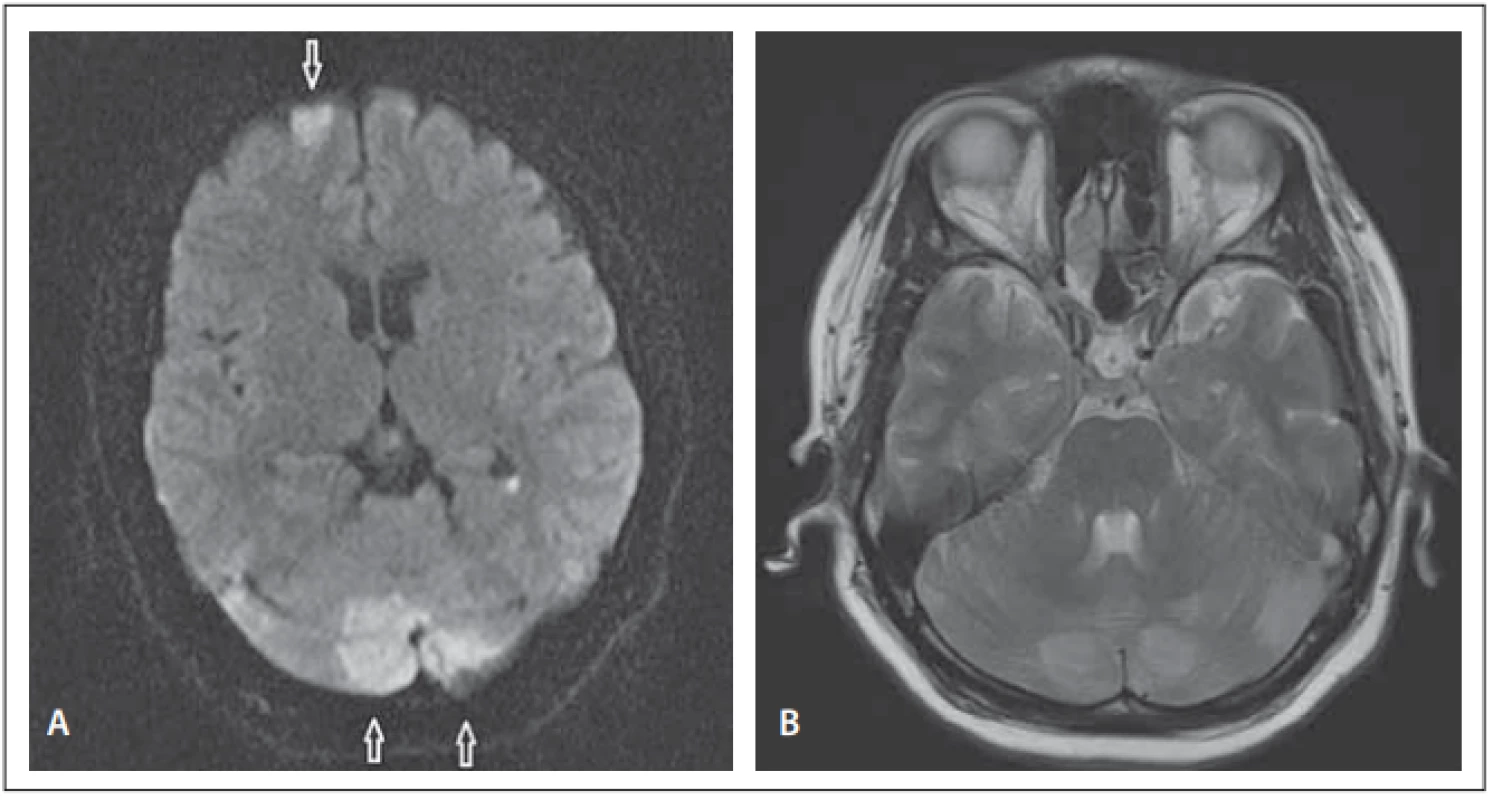
A previously healthy 35-year-old woman was admitted to the emergency department with headache, nausea, vomiting, fever, sleepiness and loss of consciousness. She had no previous complaints and the symptoms occurred with in the last few days but were gradually getting worse. She was referred to the intensive care unit upon recognition of fever (38.4 °C), somnolence and meningeal irritation signs such as neck stiffness. Laboratory tests showed leucocytosis (WBC 34,790/µL) and increased C-reactive protein (173 mg/L) and procalcitonin (1.39 ng/mL) levels. Lumbar puncture was purulent, cerebrospinal fluid (CSF) had the following composition: 377.94 mg/dL protein, 30 mg/dL glucose (concomitant blood glucose 181 mg/dL), and 1,800 WBC with abundant neutrophils. Cultures of CSF, blood, nasopharynx and urine were taken. Antibiotic therapy with meropenem 6 g/day and vancomycin 2 g/day empirically was started with the diagnosis of bacterial meningitis. Her consciousness improved quickly while her headache persisted and the synchronous neurological examination was normal except for bilateral papilledema and facial asymmetry. Diffusion weighted MRI showed focal areas of restriction in the left superior frontal, left posterior parietal; right temporo-occipital regions, both lateral ventricles (linear lesion) and both cerebellar hemispheres (Fig. 1A). Related hyperintense lesions on T2-WI MRI sequences were found especially in both cerebellar hemispheres (Fig. 1B). MR venography was normal.
Obr. 1. (A) Difuzí vážená MR – ložiska restrikce nahoře frontálně vlevo (šipka) a v obou
mozečkových hemisférách (šipky). (B) T2-WI sekvence na MR – hyperintenzní léze
v obou mozečkových hemisférách.
After 3 days of culture from CSF, small (1 mm diameter) colonies of a non-motile, Gram negative coccobacillus grew that was facultative anaerobic, oxidase positive and catalase negative and identified as Neisseria elongata by automated mass spectrometry microbial identification system (Vitek MS; bioMe’rieux, France). Unfortunately, further testing for determination of subspecies was not available.
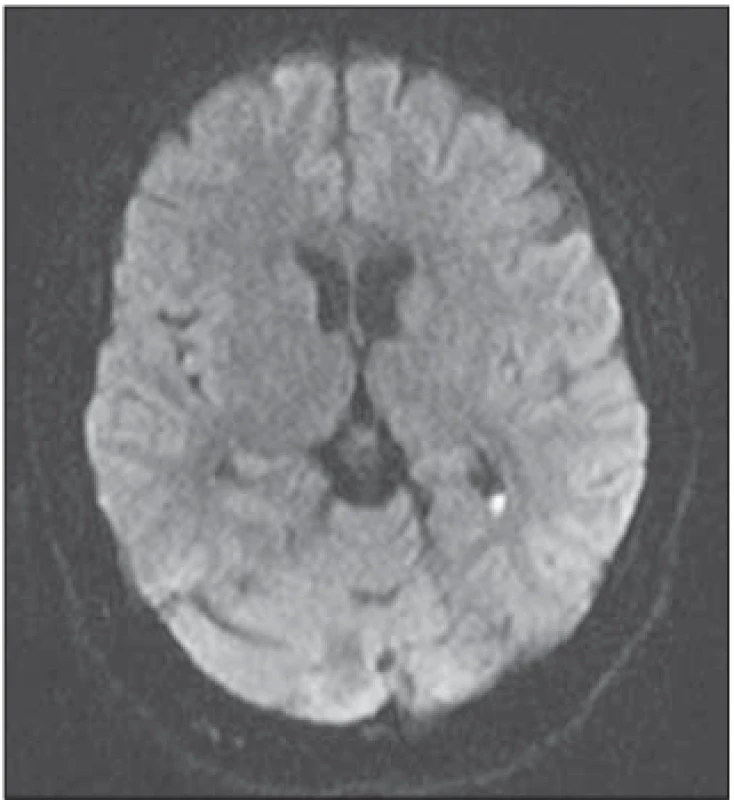
In search for the Marcy l’Etoile, predisposing cardiac disease, trans-esophageal echocardiography was found to be normal. Visual examination and EEG were also non-pathologic. Kept on antibiotic treatment for bacterial meningitis and symptomatic treatment for headache, the patient recovered symptomatically and radiologically. After 10 days, the cerebral lesions were mostly resolved (Fig. 2) and completely disappeared at the 8th week on control MRI studies confirming the diagnosis of PRES associated with meningitis.
Obr. 2. Kontrolní difuzí vážená MR po
10 dnech. Ložiskové léze v důsledku
edému z velké části vymizely.
Various definitions of PRES share common basic features that are present in more than 90% of the cases, namely: specific neurological symptoms (headache, nausea, vomiting, convulsions), predisposing factors, specific radiologic pattern (focal areas in the parieto-occipital regions of hyperintense somewhat symmetrical signals on FLAIR [fluid attenuated inversion recovery] sequences), related vasogenic brain edema, reversibility and exclusion of other patterns of encephalopathy and edema [1,2].
The exact pathophysiological mechanism leading to PRES remains conflicting. There are 2 main theories; the vasogenic theory implies the loss of autoregulation in cerebral blood flow due to sudden severe increase in blood pressure leading to cerebral hyperperfusion, vascular injury and damage to the blood-brain-barrier and resultant vasogenic edema. However, like our patient, more than 1/3 of the cases were found to be normotensive, thus an alternative mechanism based on endothelial dysfunction-injury or vasoconstriction causing hypoperfusion and ischemia was put forward [3]. The endothelial injury might be cytotoxic (immune suppressants-toxins), immunogenic (autoimmune diseases) or neuropeptide related (infection-sepsis) considering common risk factors such as arterial hypertension, renal diseases-transplantation-immune suppression, sepsis-infection, preeclampsia and autoimmune diseases [3,4]. Infection-sepsis was reported as an important predisposing factor in 20–25% of the cases [3,5].
The PRES was most probably related to cerebral infection in our patient who had clear initial clinical features like fever, meningeal irritation signs, leucocytosis, increased C-reactive protein and procalcitonin levels, purulent lumbar puncture with abundant neutrophils and so on. Thus, antibiotics were started and any additional vascular imaging was not performed. However, vascular imaging methods could be helpful to understand the blood flow conditions during the PRES as loss of cerebral small artery and precapillary sphincter autoregulation, leading to vasodilatation and finally to hyperperfusion and vasogenic edema, which might be the mechanism in normotensive patients.
N. meningitidis normally colonizes the nasopharynx asymptomatically and the ability to invade the blood stream for the life-threatening meningitis, N. meningitidis’ virulence is related to acquisition-possession of a polysaccharide capsule probably after genetic transport from other Neisseria species [6]. Capsule genes were identified in nonpathogenic Neisseria species, including Neisseria subflava and Neisseria elongata showing potential for human disease [6]. Neisseria elongata (family Neisseriaceae) is also a commensal of the oropharynx and subspecies nitroreducens is a rarely reported cause of septicaemia and endocarditis usually in patients with cardiac valve disease or history of a dental procedure-infection [7,8]. PRES related to meningitis is extremely rare and to our knowledge this is the first case of N. elongata meningitis associated PRES [2,9]. CNS involved-complicated N. elongata infection is also a very rarely reported event [7]. As mentioned before, cardiac valve disease or dental procedure history is commonly present in N. elongata infections. Though our patient did not have any cardiac disease, common dental procedures might be a probability.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
The Editorial Board declares that the manu script met the ICMJE “uniform requirements” for biomedical papers.
Funda Uysal Tan, MD
Department of Neurology School of Medicine
Hitit University
Erol Olcok Hospital Çorum
Turkey
e-mail: fundauysaltan@yahoo.com
Accepted for review: 11. 5. 2020
Accepted for print: 8. 10. 2020
Sources
1. Gao B, Lyu C, Lerner A et al. Controversy of posterior reversible encephalopathy syndrome: what have we learnt in the last 20 years? J Neurol Neurosurg Psychiatry 2018; 89 (1): 14–20. doi: 10.1136/jnnp-2017-316225.
2. Panda M, Rustogi D, Singh A et al. Posterior reversible encephalopathy syndrome in a child with meningitis presenting with transient visual loss and hypertension. Indian J Pediatr 2013; 80 (11): 965–967. doi: 10.1007/s12098-012-0937-z.
3. Racchiusa S, Mormina E, Ax A et al. Posterior reversible encephalopathy syndrome (PRES) and infection: a systematic review of the literature. Neurol Sci 2019; 40 (5): 915–922. doi: 10.1007/s10072-018-3651-4.
4. Lamy C, Oppenheim C, Mas JL. Posterior reversible encephalopathy syndrome. Handb Clin Neurol 2014; 121 : 1687–701. doi: 10.1016/B978-0-7020-4088-7.00109-7.
5. Bartynski WS, Boardman JF, Zeigler ZR et al. Posterior reversible encephalopathy syndrome in infection, sepsis, and shock. AJNR Am J Neuroradiol 2006; 27 (10): 2179–2190.
6. Clemence ME, Maiden MC, Harrison OB. Characterization of capsule genes in non-pathogenic Neisseria species. Microb Genom 2018; 4 (9): e00020. doi: 10.1099/mgen.0.000208.
7. Hsiao JF, Lee MH, Chia JH et al. Neisseria elongata endocarditis complicated by brain embolism and abscess. J Med Microbiol 2008; 57 (Pt 3): 376–381. doi: 10.1099/jmm.0.47493-0.
8. Wong JD, Janda JM. Association of an important Neisseria species, Neisseria elongata subsp. nitroreducens, with bacteremia, endocarditis, and osteomyelitis. J Clin Microbiol 1992; 30 (3): 719–720.
9. Hye-Na P, Yun-Sook K. Posterior reversible encephalopathy syndrome following meningitis in pregnancy. Soonchunhyang Med Sci (SMS) 2017; 23 (1): 38–41. doi: 10.15746/sms.17.008
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2020 Issue 5
- Memantine Eases Daily Life for Patients and Caregivers
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
- Advances in the Treatment of Myasthenia Gravis on the Horizon
-
All articles in this issue
- Diffuse low grade gliomas
- Respiratory rehabilitation in patients with amyotrophic lateral sclerosis
- Socio-economic impact of headache disorders –reasons and improvement possibilities
- Neurorehabilitation in patients with amyotrophic lateral sclerosis
- Surgical treatment of degenerative scoliosis
- Functional and structural cortical changes in patients with non-specific low back pain
- Cognitive-motor interference after stroke
- Sonographic evaluation of sciatic nerve in individuals with S1 radicular symptoms
- Taste strips – the method of a self-administered taste function test
- The efficiency of micro-vascular decompression versus micro-vascular decompression with partial sensory rhizotomy for classical trigeminal neuralgia – a retrospective analysis of 58 patients
- Patient with Parkinson‘s disease in data sources of the National Health Information System
- Treatment with intravenous trombolysis out of stroke center
- Decompressive craniectomy in malignant middle cerebral artery infarction – monoinstitutional retrospective analysis of a set of 33 patients
- Consecutive low-flow and high-flow EC-IC bypass in ischemia prevention during internal carotid artery sacrifice in intracavernous aneurysm
- Venous sinus stenting in idiopathic intracranial hypertension
- Posterior reversible encephalopathy syndrome associated with Neisseria elongata meningitis
- Hyperbarická oxygenoterapie & mozek; přehled z výroční konference EUBS 2019
- Amnesia Light and Brief Assessment (ALBA) test – the second version and repeated examinations
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Diffuse low grade gliomas
- Respiratory rehabilitation in patients with amyotrophic lateral sclerosis
- Amnesia Light and Brief Assessment (ALBA) test – the second version and repeated examinations
- Neurorehabilitation in patients with amyotrophic lateral sclerosis
