-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Genome-Wide Association Study Identifies as a Susceptibility Gene for Pediatric Asthma in Asian Populations
Asthma is a complex phenotype influenced by genetic and environmental factors. We conducted a genome-wide association study (GWAS) with 938 Japanese pediatric asthma patients and 2,376 controls. Single-nucleotide polymorphisms (SNPs) showing strong associations (P<1×10−8) in GWAS were further genotyped in an independent Japanese samples (818 cases and 1,032 controls) and in Korean samples (835 cases and 421 controls). SNP rs987870, located between HLA-DPA1 and HLA-DPB1, was consistently associated with pediatric asthma in 3 independent populations (Pcombined = 2.3×10−10, odds ratio [OR] = 1.40). HLA-DP allele analysis showed that DPA1*0201 and DPB1*0901, which were in strong linkage disequilibrium, were strongly associated with pediatric asthma (DPA1*0201: P = 5.5×10−10, OR = 1.52, and DPB1*0901: P = 2.0×10−7, OR = 1.49). Our findings show that genetic variants in the HLA-DP locus are associated with the risk of pediatric asthma in Asian populations.
Published in the journal: Genome-Wide Association Study Identifies as a Susceptibility Gene for Pediatric Asthma in Asian Populations. PLoS Genet 7(7): e32767. doi:10.1371/journal.pgen.1002170
Category: Research Article
doi: https://doi.org/10.1371/journal.pgen.1002170Summary
Asthma is a complex phenotype influenced by genetic and environmental factors. We conducted a genome-wide association study (GWAS) with 938 Japanese pediatric asthma patients and 2,376 controls. Single-nucleotide polymorphisms (SNPs) showing strong associations (P<1×10−8) in GWAS were further genotyped in an independent Japanese samples (818 cases and 1,032 controls) and in Korean samples (835 cases and 421 controls). SNP rs987870, located between HLA-DPA1 and HLA-DPB1, was consistently associated with pediatric asthma in 3 independent populations (Pcombined = 2.3×10−10, odds ratio [OR] = 1.40). HLA-DP allele analysis showed that DPA1*0201 and DPB1*0901, which were in strong linkage disequilibrium, were strongly associated with pediatric asthma (DPA1*0201: P = 5.5×10−10, OR = 1.52, and DPB1*0901: P = 2.0×10−7, OR = 1.49). Our findings show that genetic variants in the HLA-DP locus are associated with the risk of pediatric asthma in Asian populations.
Introduction
Asthma is the most common chronic disorder in children, and asthma exacerbation is an important cause of childhood morbidity and hospitalization. The prevalence of childhood asthma in Japan is 5.0% among school children in 2006 [1], and an estimated 300 million people worldwide have asthma [2]. Asthma is characterized by airway hyperresponsiveness and inflammation, tissue remodeling, and airflow obstruction. Infiltration of lymphocytes, mast cells, and eosinophils in the airways cause airway inflammation, and T helper (Th) type 2 cytokines play crucial roles in orchestrating the inflammatory responses; thus, asthma is considered a Th2-type immune disease.
Previously conducted genome-wide association studies (GWAS) for asthma identified association with the loci on chromosomes 17q21 (ORMDL3 for Caucasian pediatric asthma, odds ratio (OR) = 1.45, P = 1×10−10) [3], 5q21 (PDE4D for pediatric asthma, OR = 0.6, P = 4.7×10−7) [4], 9q21.31 (TLE4 for Hispanic pediatric asthma, OR = 0.6, P = 6.8×10−7) [5], and 1q31 (DENND1B for Europeans and African ancestries [6], OR = 0.77 and 1.41, respectively; combined P = 1.7×10−13). A GWAS for severe asthma identified association with the region between RAD50 and IL5 on chromosome 5q (OR = 1.64, P = 3.0×10−7) and HLA-DR/DQ (OR = 0.68, P = 9.6×10−6), but they did not include a replication dataset [7]. Recently, Moffatt et al. conducted a large-scale GWAS in Caucasian populations and identified 6 loci (IL18R1, HLA-DQ, IL33, SMAD3, GSDMB/GSDMA, and IL2RB) associated with asthma [8].
In the present study, we conducted the first GWAS in Asian population for pediatric asthma by using Illumina HumanHap550/610-Quad BeadChip (Illumina, San Diego, USA).
Results
GWAS analysis
The GWAS flow chart is shown in Figure 1. We analyzed 450,326 SNPs in 938 cases and 2,376 controls, using standard quality control practices (Table S1). The genotypes in cases and controls were compared using the Cochran–Armitage trend test (Figure 2). There was only minor inflation of the genome-wide statistical results owing to population stratification (genomic control (λGC) = 1.048; Figure 3). Five SNPs (rs3019885, rs987870, rs2281389, rs2064478, and rs3117230) showed strong association with pediatric asthma with P<1×10−8. Of these, rs2064478 and rs3117230 were in complete linkage disequilibrium (LD) (r2 = 1) with rs2281389. In order to validate the results of the GWAS, we tested the remaining 3 SNPs (rs3019885, rs987870, and rs2281389) in 2 independent replication cohorts comprising Asians (Japanese and Koreans), considering P<0.05 as significant replication.
Fig. 1. Flow chart of the present study. 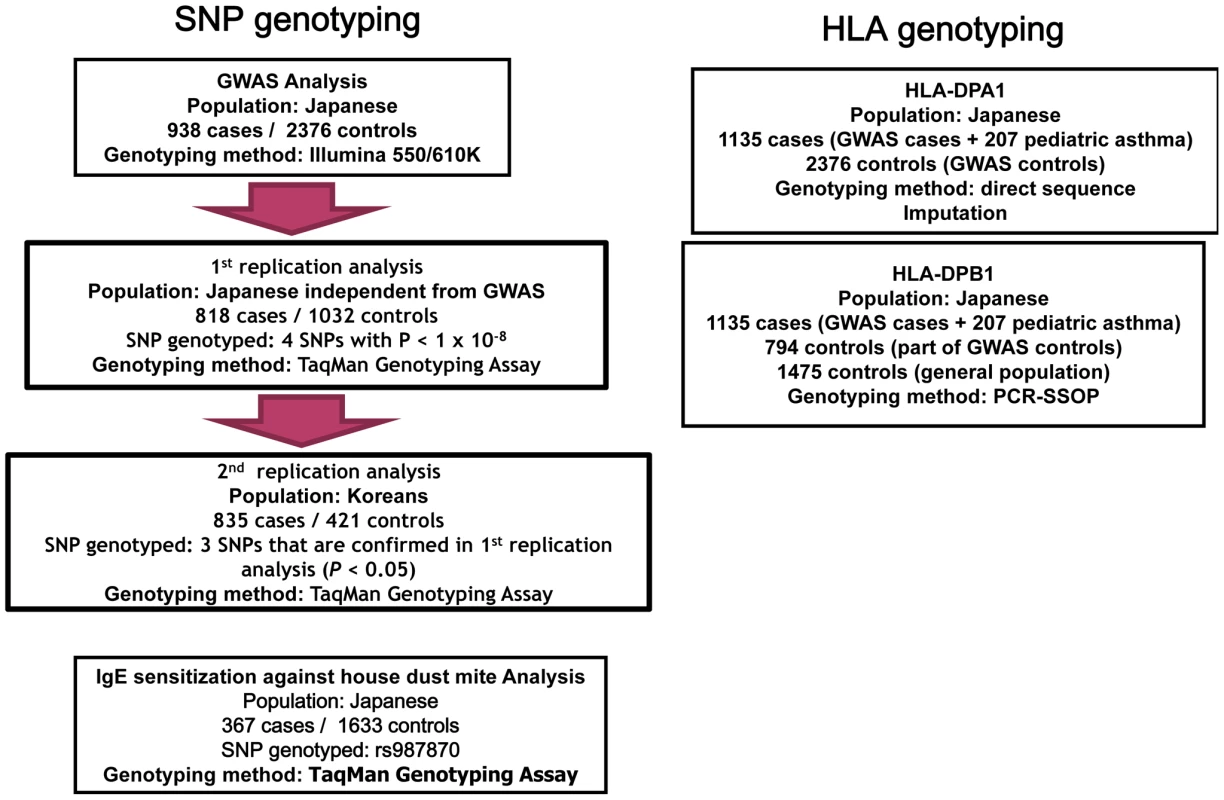
Fig. 2. P values of GWAS. 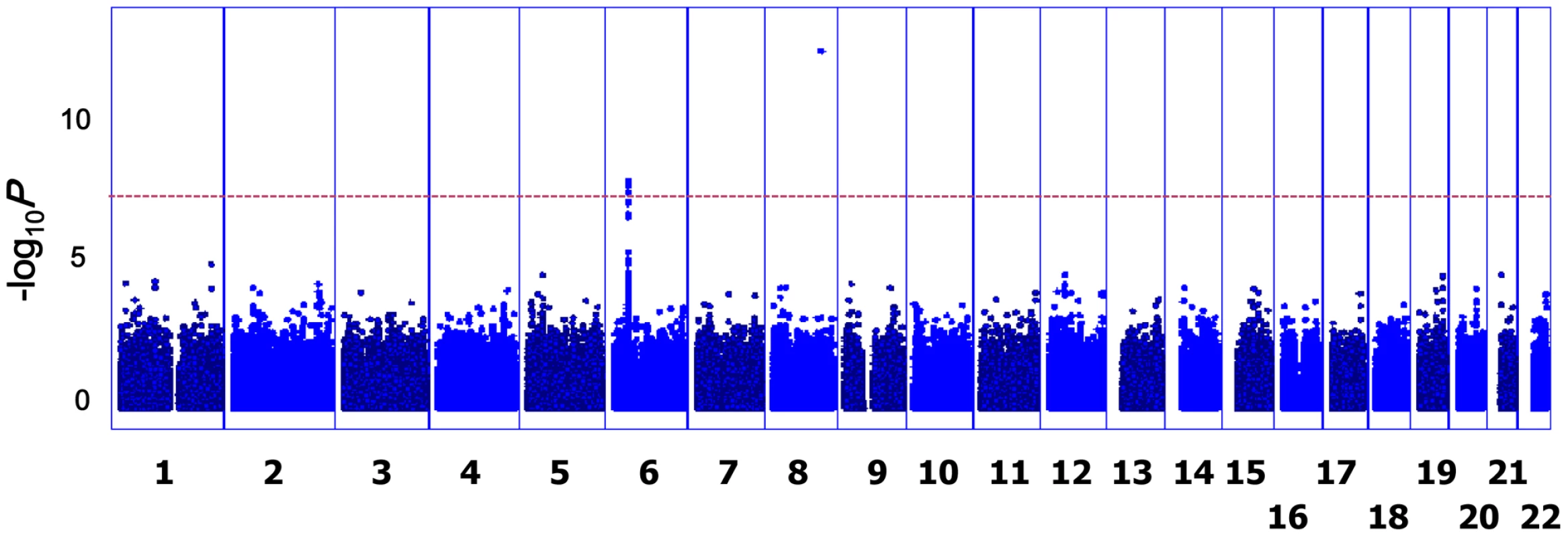
The Manhattan plot shows the Cochran–Armitage trend test P values for 938 cases of asthma and 2,376 controls; 450,326 autosomal SNPs were considered in the study. The dashed line indicates the genome-wide significance level (P<5×10−8). Fig. 3. Quantile–quantile (Q–Q) plot of GWAS for pediatric asthma. 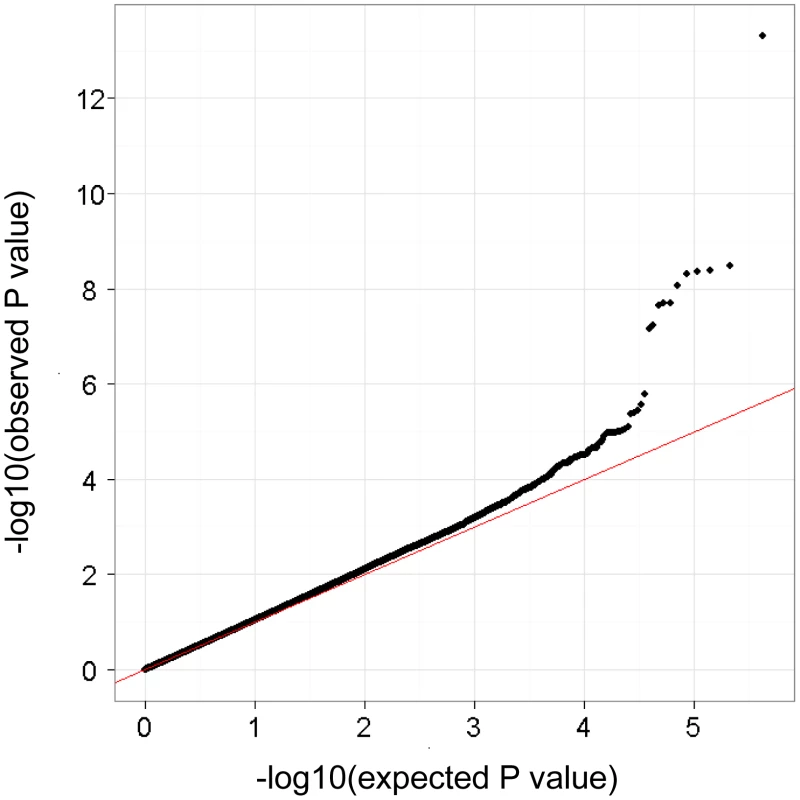
The results of the Cochrane–Armitage trend P are plotted as dots and the line y = x is in red. The horizontal and vertical lines represent expected P values under null distribution and observed P values, respectively. Of these 3 SNPs, significant associations were noted at rs987870 in both cohorts (Table 1). To merge the findings of these studies, we conducted meta-analysis with a fixed-effects model by using the Mantel–Haenszel method. As shown in Table 1, the Mantel–Haenszel P value of 2.3×10−10 was noted for rs987870 (OR = 1.40, confidence interval (CI) = 1.26–1.55).
Tab. 1. Results of GWAS and replication studies for 4 SNPs. 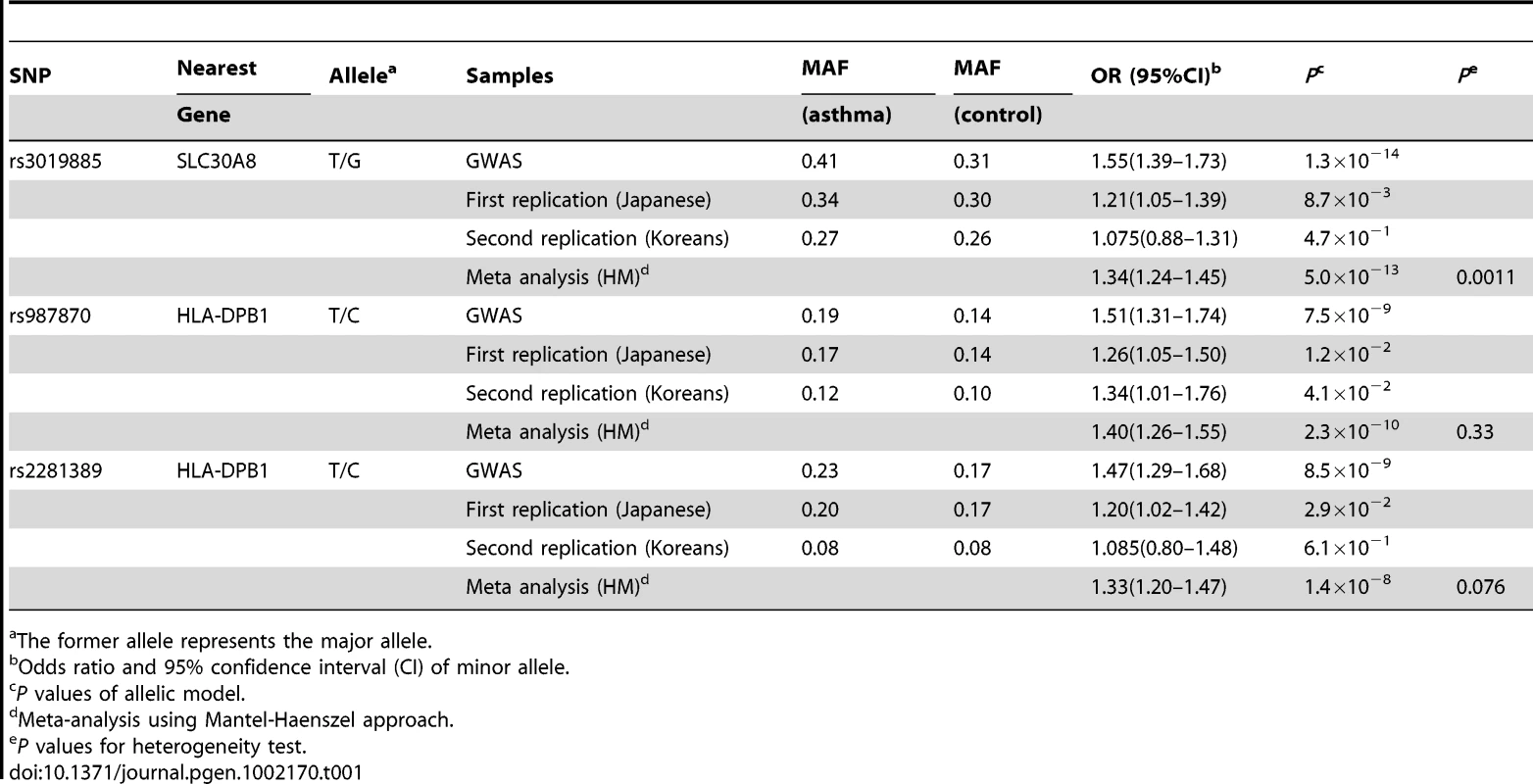
The former allele represents the major allele. HLA-DP association with pediatric asthma
The rs987870 is located between HLA-DPA1 and HLA-DPB1. Genotype imputation using MACH [9] revealed association between asthma and the SNPs that were in strong LD with rs987870 (Figure 4, Table S2). Moreover, rs987870 C allele was in complete LD with DPA1*0201 (r2 = 1). We determined HLA-DPA1 genotypes by using direct sequencing and MACH imputation of the data from 1135 cases and 2376 controls and found that DPA1*0201 was strongly associated with pediatric asthma (P = 5.2×10−10, OR = 1.52, Table 2). Then, we determined the HLA-DPB1 genotypes in 1135 cases and 2296 controls and found that DPB1*0901 was associated with pediatric asthma (P = 2.0×10−7, OR = 1.49, Table 3). DPB1*0901 was in strong LD with DPA1*0201 and rs987870 C allele (D prime = 0.93). Because more than 90% of pediatric asthma patients were allergic to house dust mites, it is possible that the association was due to IgE reactivity (sensitization) against mites. We performed an association study for mite sensitization using independent adult subjects without allergic respiratory diseases such as asthma and perennial allergic rhinitis (367 subjects with house dust mite-specific IgE and 1633 subjects without mite-specific IgE). Subjects with house dust mite-specific IgE were non-allergic in terms of symptoms but possessed mite-specific IgE. Subjects without mite-specific IgE did not exhibit allergic symptoms. We did not find an association between rs987870 and mite sensitization (P = 0.54, OR = 1.07, Table S3).
Fig. 4. Association findings of genotyped (squares) and imputed (circles) SNPs in the HLA-DP region. 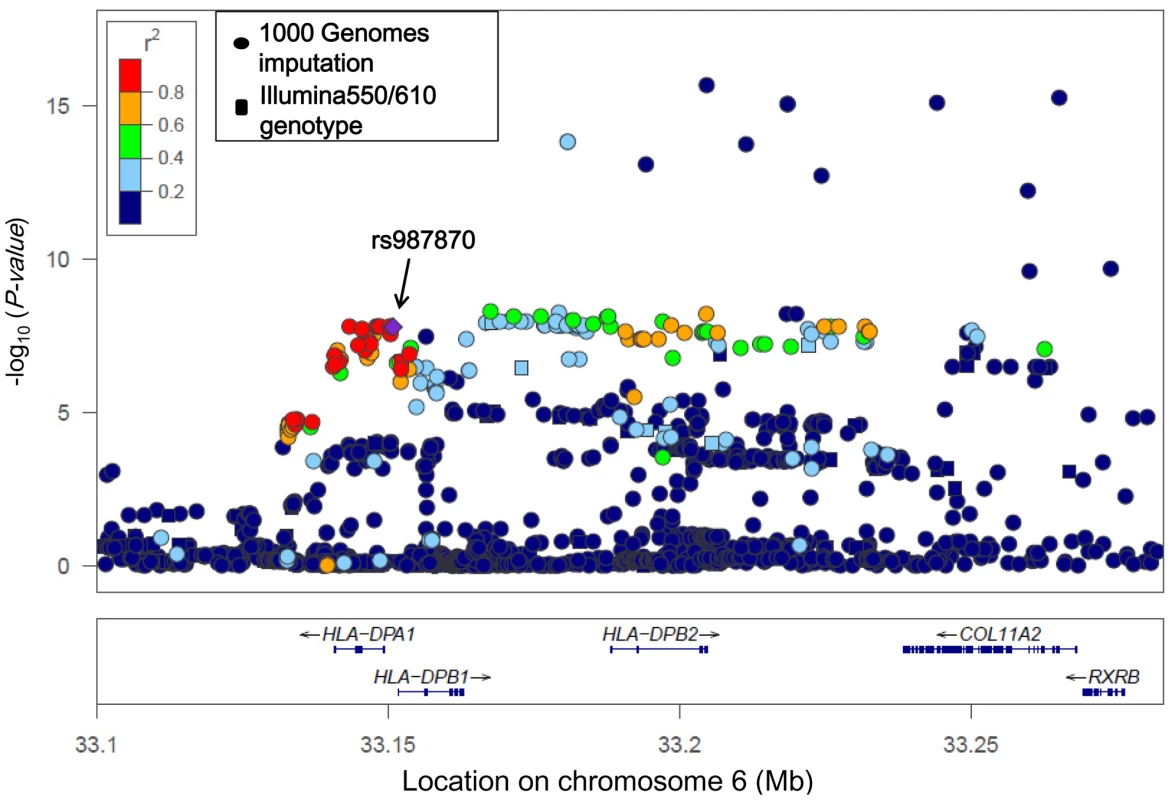
SNP rs987870, which consistently showed an association with pediatric asthma in 3 independent populations, is located in the LD block between HLA-DPA1 and HLA-DPB1. The color intensity of each symbol reflects the extent of LD with rs987870: from red (r2>0.8) to blue (r2<0.2). The physical positions are based on NCBI build 36 of the human genome. Tab. 2. HLA-DPA1-rs987870 Haplotype analysis of pediatric asthma. 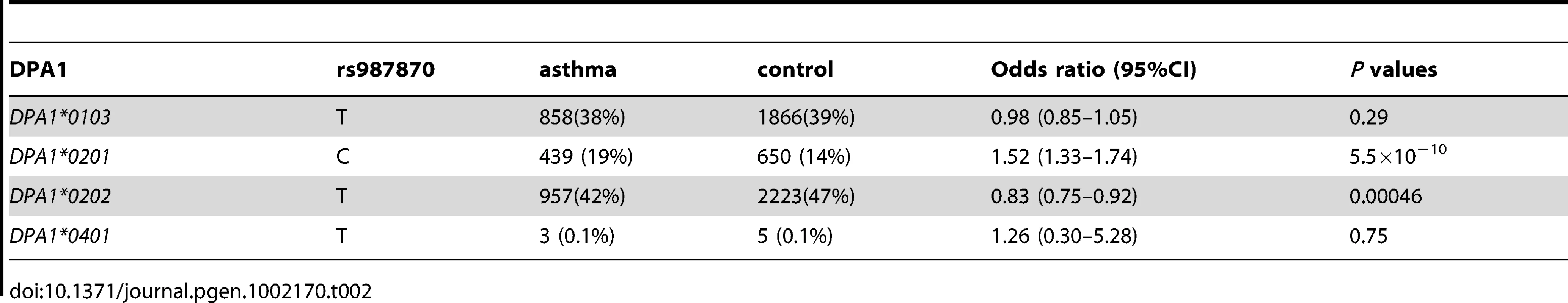
Tab. 3. HLA-DPB1 allele frequency in pediatric asthma and controls. 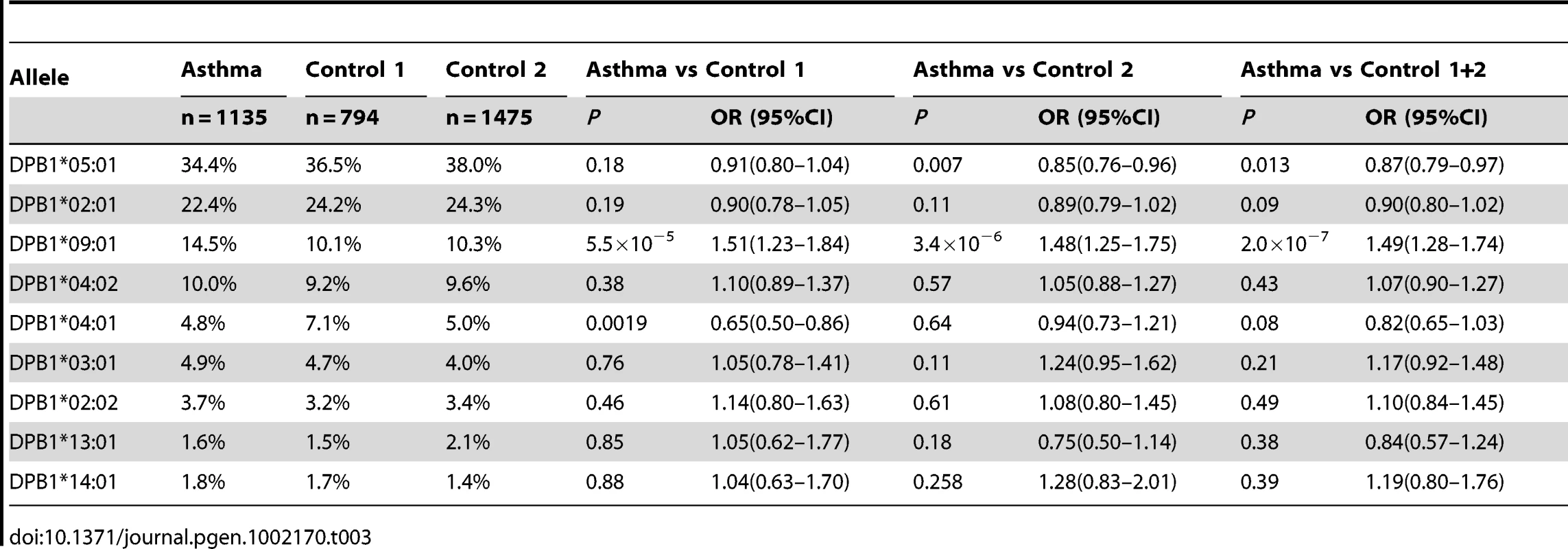
Discussion
Our GWAS in Asian populations found HLA-DP as susceptibility gene for pediatric asthma. Majority of pediatric asthmas are atopic (i.e., familial tendency to produce IgE antibodies against common environmental allergens) and possess specific IgE against the house dust mite. Mite sensitization is more prevalent in Asia than in Europe and is observed in 39% of the general adult population in Japan [10]. High prevalence of mite sensitization in asthmatic children has also been reported in Taiwan, where 94.2% of children with asthma are sensitized against Dermatophagoides pteronyssinus [11]. However, only a small subset of subjects with house dust allergy develop asthma [12].
We performed an independent association study for mite sensitization in adult subjects without allergic respiratory diseases and did not find an association between rs987870 and mite sensitization without symptoms. If the relative risk for mite sensitization in the individuals carrying a putative risk allele was 1.4 and the allele frequency was 0.15 compared to that in individuals without the allele, the statistical power of the sample size for mite sensitization study was 0.92 at an alpha level of 0.05. These results suggested that DPA1*0201 and DPB1*0901 may be associated with asthma rather than IgE production against house dust mite.
The association signal was stretched in the region of HLA-DPB2, collagen, type XI, alpha 2 (COL11A2), and Retinoid X receptor beta (RXRB) (Figure 4). Because of LD in this region, it is difficult to specifically identify causative variants. HLA-DPB2 is a pseudogene. COL11A2 encodes a component of type XI collagen called the pro-alpha2(XI) chain. Mutations in COL11A2 have been associated with non-syndromic deafness, otospondylomegaepiphyseal dysplasia, Weissenbacher-Zweymüller syndrome, and Stickler syndrome (OMIM ID *120290). RXRB belongs to the RXR family and is involved in mediating the effects of retinoic acid. RXRB forms a heterodimer with the retinoic acid receptor and thus preferentially increases its DNA binding and transcriptional activity at promoters containing retinoic acid [13]. All SNPs showing strong association with asthma (P<1×10−10) were located in introns or intergenic regions. LD of these associated SNPs with rs987870 was not strong; therefore, it is likely that the functional effect is due to DPA1*0201 and DPB1*0901.
In HLA-DP, Caraballo et al. reported that DPB1*0401 is significantly decreased in patients with allergic asthma in Mulatto population (an admixture population of European and African ancestries) [14]. Apart from the study of Caraballo et al., the association between HLA-DP alleles and asthma was restricted to occupational [15] or aspirin-induced asthma [16]. Howell et al. reported associations between HLA-DR genotype and asthma and between HLA-DPA1*0201 and IgE specific to grass pollen mix and the pollen allergen Phl p 5 [17]. Grass pollen allergy is not a major cause of asthma in Japan [18]; therefore, the HLA-DPA1*0201 association in the present study was less likely to be due to sensitization to grass pollen.
DPA1*0201 has also been reported to be positively associated with lower levels of rubella-induced antibodies [19], cytokine immune responses against measles vaccine [20], and ulcerative colitis [21], and negatively associated with type 1 diabetes [22]. DPB1*0901 was shown to be associated with systemic sclerosis [23], non-permissive mismatches for hematologic stem cell transplantation [24], ulcerative colitis [21], and Takayasu's arteritis [25]. HLA-DP molecules present short peptides of largely exogenous origin to CD4-positive helper T cells and other T cells, leading to subsequent immunological responses. T cells recognize complex formation between a specific HLA type and a particular antigen-derived epitope. Therefore, HLA molecules capable of binding a particular epitope can restrict T cell induced-immune responses, leading to association between particular HLA types and immune-related diseases. Type 1 diabetes is a Th-1 type immune disease. Varney et al. studied 1,771 type 1 diabetes multiplex families, analyzing them by the affected family-based control method [26], and found that DPA1*0201 has a protective effect on the development of type 1 diabetes (adjusted P = 5×10−4, OR 0.7) [22]. Epidemiologic studies have associated type 1 diabetes with lower prevalence of asthma and other allergic diseases [26], [27]. Also, the previous GWAS of rheumatoid arthritis, other Th-1 type immune disease, has shown that rs987870 C allele confers protection against rheumatoid arthritis [28]. These findings suggest that HLA-DPA1*0201 could determine Th1/Th2 dominance and could partially explain the inverse relationship between asthma and Th-1 type immune diseases.
Previous GWAS involving European, Mexican, and African populations showed association of asthma with SNPs located in several newly discovered genes. Our GWAS dataset supported an association between identical SNPs reported in ORMDL3/GSDMB/GSDMA, IL5/RAD50/IL13, HLA-DR/DQ, and SMAD3 and pediatric asthma (P<0.05, Table S4). Two asthma GWA studies revealed an association of HLA-DQ with pediatric/adult asthma in Caucasians [7], [8]. HLA-DQ, like HLA-DP, is an αβ heterodimer of the MHC Class II type. Like HLA-DP, HLA-DQ recognizes and presents foreign antigens, but is also involved in recognizing common self-antigens and presenting those antigens to the immune system.
We failed to replicate the top SNPs of PDE4D, TLE4, DENND1B, IL18R1, and IL2RB that were reported in the original articles, but several SNPs in the regions surrounding PDE4D and IL2RB showed significant association when we set the significance level at P = 0.05 (Table S4). The different LD patterns/allele frequencies observed in PDE4D and IL2RB in Asians and Caucasians may explain the different SNP associations observed in different ethnic populations. rs1342326 in IL33 was not polymorphic in the Asian population.
There were several limitations of the present GWAS. The controls for the GWAS and 1st replication samples were from adult populations. Information regarding history of asthma in early childhood or other asthma-related information (i.e., status of allergic sensitization and lung function) was not collected for these controls. Therefore, we cannot exclude the possibility that our control samples may include subjects who outgrew asthma. The prevalence of pediatric asthma in Japan is around 5%; therefore, our GWAS samples have reduced power compared with that of selected controls. In the 1st replication Japanese controls, subjects with present and past history of allergic diseases were excluded, and Korean controls in the 2nd replication were non-allergic pediatric controls (Table S5).
The genomic control value in the present study was 1.053, indicating minor population stratification. The Japanese population comprises 2 clusters (Hondo and Ryukyu; Hondo is the mainland of Japan and Ryukyu is the name of the island south of Japan). We performed principal component analysis using EIGENSTRAT software [29] to identify subjects belonging to Ryukyu. Because 2nd or 3rd generation Chinese live in Japan, and the genetic population structure in Chinese differs from that in Japanese, we also performed principal component analysis to exclude Chinese subjects. Although hidden population stratification may exist, its influence on the final results is not expected to be significant.
rs3019885 is located in intron 2 of solute carrier family 30 (SLC30A8), and showed strong association in the GWAS population. The association was replicated in the independent Japanese samples, but not in the Korean population. SLC30A8 is a zinc efflux transporter expressed at high levels only in the pancreas; the GWAS revealed that variants of SLC30A8 are associated with type 2 diabetes [30]. Japanese and Koreans are genetically close but we cannot exclude the possibility that the association of rs3019885 with pediatric asthma is population specific.
In conclusion, we performed the first GWAS in Asian population for pediatric asthma and found that DPA*0201/DPB1*0901 is strongly associated with pediatric asthma. The association with the HLA-DP locus emphasizes the importance of the HLA-class II molecules on the biological pathways involved in the etiology of pediatric asthma, and suggests that HLA-DP can be a therapeutic target for asthma.
Materials and Methods
Ethical statement
The study was approved by the institutional review board and the ethics committee of each institution. Written informed consent was obtained from each participant in accordance with institutional requirements and the Declaration of Helsinki Principles.
Subject participants
Characteristics of pediatric asthma cases and controls are summarized in Table S5.
GWAS population
All subjects with asthma were child or child-onset (<15 years old) asthmatics in Japan. Patients were recruited from 3 pediatric hospitals and 1 pediatric clinic, and the diagnosis of the asthma in all patients was confirmed by specialists in pediatric allergology on the basis of the criteria of the National Institutes of Health, USA, with minor modifications.
The control cases for the GWAS were healthy Japanese adult subjects from Osaka (n = 964), Tokyo (n = 660), and Ibaraki (n = 778) who had no current history of asthma [31]. In the GWAS, we genotyped 978 cases with pediatric asthma and 2402 controls using Illumina HumanHap550v3/610-Quad Genotyping BeadChip (Illumina, San Diego, USA). Subjects from Osaka and Ibaraki were randomly selected from residents of Suita city and Tone town, respectively. Subjects from Tokyo were hospital workers from Keio University Hospital, Tokyo. We excluded samples considered duplicated, related (first - or second-degree relatives), or belonging to Han Chinese or Ryukyu. In total, 938 cases and 2376 controls were considered for further analysis.
First replication population (Japanese)
We recruited 818 subjects with childhood atopic asthma from the Osaka Prefectural Medical Center for Respiratory and Allergic Diseases, Dokkyo University School of Medicine, National Research Institute for Child Health & Development, National Sagamihara Hospital, and Chiba University Hospital. All subjects with bronchial asthma were diagnosed according to the criteria of the National Institutes of Health (National Heart, Lung, and Blood Institute, National Institutes of Health, 1991) by physicians who were asthma specialists [32], [33]. After the exclusion of individuals who had been diagnosed with asthma, atopic dermatitis, or nasal allergies by physicians' interviews, 825 healthy individuals were recruited from the Midousuji Rotary Club [32], [33]. Two hundred and seven control subjects who never had the symptoms of allergic rhinitis/asthma and did not show any sensitization to 7 common aeroallergens were recruited from Fukui [34].
Second replication population (Korean)
Patients with pediatric asthma were enrolled at Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. The control subjects were age-matched children with no history of asthma or other allergic diseases, negative skin prick test, and normal total IgE values (<100 IU/mL) recruited from the same district (Seoul). Total of 835 cases and 421 controls participated in this study. The details of the patients and controls were described in a previous study [35].
Subjects for IgE sensitization against house dust mite
General populations for mite sensitivity study were recruited from Fukui [10] and Tsukuba in Japan. Total and specific IgE levels (produced in response to Japanese cedar, Dermatophagoides, Dactylis glomerata, Ambrosia artemisiifolia, Candida albicans, and Aspergillus) were measured using the CAP-RAST method (for Fukui samples; Pharmacia Diagnostics AB, Uppsala, Sweden) or MAST-26 (for Tsukuba samples; Hitachi Chemical Co. Ltd., Tokyo, Japan). Positive sensitization against house dust mite was defined as specific IgE levels against the house dust mite (Dermatophagoides farinae or Dermatophagoides pteronyssinus) greater than or equal to 0.70 IU/ml (class 2) or lumicount greater than 2.76 (class 2). Subjects with asthma (current or past) or perennial allergic rhinitis were excluded from the analysis. Sensitized subjects (Mite-positive) were non-allergic in terms of symptoms but possessed mite-specific IgE. Non-sensitized subjects (Mite-negative) did not show any allergic symptoms and did not have mite-specific IgE.
Subjects for HLA-DPA1 typing
Cases with asthma included 938 subjects used in GWAS analysis and 207 Japanese subjects with child - or child-onset (<15 years) asthmatics recruited in Tsukuba. The diagnosis of asthma in all patients was confirmed by specialists in pediatric allergology on the basis of the criteria of the National Institutes of Health, USA, with minor modifications. The control subjects were 2378 subjects that were used in GWAS analysis. Because most of the DNA from the GWAS controls was not available for genotyping, and we found that imputation of the HLA-DPA1 allele using GWAS results was highly accurate (error rate, 0.003), we decided to genotype the HLA-DPA1 allele by direct sequencing and imputation. Among the subjects for HLA-DPA1 genotyping (1135 cases and 2376 controls), genotyping of 383 subjects was performed by direct sequencing and genotyping of the remaining 3128 samples was performed by imputation.
Subjects for HLA-DPB1 typing
Cases with asthma included 938 subjects used in GWAS analysis and 207 Japanese subjects with child - or child-onset (<15 years) asthmatics; the same as those used in HLA-DPA1 typing. The control 1 subjects for HLA-DPB1 typing were 794 healthy adult subjects from Tokyo and 399 subjects were the same as those in GWAS. The control 2 subjects (n = 1475) were general datasets from Japanese population samples publically available at http://www.hla.or.jp/hapro/top.html. Because most of the DNA from the GWAS controls was not available for genotyping, and the imputation of the DPB1 allele using the GWAS results was not possible, we used 794 healthy adult subjects from Tokyo and 399 subjects from the GWAS for DPB1 genotyping (Control 1). The control 2 subjects (n = 1475) were general datasets from Japanese population samples publically available at http://www.hla.or.jp/hapro/top.html. The status of asthma or other allergic diseases for these samples is not available.
Genotyping
Genotyping for GWAS was performed using the Illumina HumanHap550v3/610-Quad Genotyping BeadChip (Illumina), as per manufacturer's instruction.
In replication analyses, genotyping of each individual was performed with the TaqMan genotyping system (Applied Biosystems) on an ABI PRISM 7900HT Sequence Detection System (Applied Biosystems). PCR was performed on a 384-well format, and automatic allele calling was performed using ABI PRISM 7900HT data collection and analysis software, version 2.2.2 (Applied Biosystems).
HLA-DPB1 genotyping of 1135 cases, 794 controls (control 1) and 1475 controls (control 2) were performed with the WAKFlow HLA typing kit (Wakunaga, Hiroshima, Japan), as per manufacturer's instruction. First, the target DNA was amplified by polymerase chain reaction (PCR) with biotinylated primers specifically designed for each HLA-DPB1 locus. Then, the PCR product was denatured and hybridized to complementary oligonucleotide probes immobilized on fluorescent-coded microsphere beads. Concurrently, the biotinylated PCR product was labeled with phycoerythrin-conjugated streptavidin and immediately examined with the Luminex 100 system (Luminex, Austin, TX). Genotype determination and data analysis were performed with the WAKFlow typing software (Wakunaga).
HLA-DPA1 genotyping was performed with direct sequencing of exon 2 with forward primer 5′-TCAGGATGCCCAGACTTTCAA-3′ and reverse primer 5′-CAGGGGGCACTTAGGCTTCC-3′, and with the sequencing primer 5′-TCAGGATGCCCAGACTTTCAA-3′ using the BigDye Terminator v.1.1 Cycle Sequencing Kit (Applied Biosystems) on an ABI PRISM 3130 Genetic Analyzer (Applied Biosystems).
Statistical analysis
In the GWAS, we examined the potential genetic relatedness on the basis of pairwise identity by state for all of the successfully genotyped samples using the EIGENSTRAT software [29]. In the GWAS, we genotyped 978 cases with pediatric asthma and 2402 controls using Illumina HumanHap550v3/610-Quad Genotyping BeadChip (Illumina, San Diego, USA). Samples of duplicated (identical individual or monozygotic twin), first-, second-, and third-degree pairs were detected, and the individual with a lower call rate was excluded from further analysis. PCA was performed, and the results were combined with those obtained for our in-house Ryukyu and Han Chinese reference samples. Yamaguchi-Kabata et al. characterized the Japanese population structure using the genotypes for 140,387 SNPs in 7003 Japanese individuals, along with 60 European, 60 African, and 90 East-Asian individuals, in the HapMap project and found that the Japanese population is composed of 2 clusters (Hondo and Ryukyu) [36]. Hondo is the biggest island of Japan, and the island of Ryukyu is located in southern Japan. Also, we have 2nd or 3rd generation Chinese living in Japan, and Chinese present a different genetic population structure from Japanese. Therefore, we excluded samples belonging to Han Chinese or Ryukyu, and 938 cases and 2376 controls were considered for further analysis.
Cluster plots of SNPs were checked by visual inspection and SNPs with ambiguous calls were excluded. We excluded SNPs with a low genotyping rate (<90%), minor allele frequency less than 0.01 in either pediatric asthma cases or controls, or with Hardy-Weinberg equilibrium P value<10−4 in controls. Finally, 450,326 SNPs were used for the GWAS. Details regarding the exact number of remaining SNPs after applying each quality control criterion are available in Table S1.
The genomic control inflation factor (λGC), defined as the median association test statistic across all SNPs divided by its expected value, was calculated by the method proposed by Devlin et al. [37]. GWAS and replication analyses were performed using the Cochran–Armitage trend test and χ2 test. The meta-analysis was performed with the Mantel–Haenszel approach as a fixed-effects model [38]. All statistical findings were reported without correction. The results of GWAS were plotted with GWAS GUI v0.0.2 [39]. HLA-DP region was plotted with LocusZoom [40]. The power calculation was performed with Genetic Power Calculator [41]. Quantile-quantile (Q-Q) plot was plotted with ggplot2 package [42] in R version 2.10.0 (http://www.r-project.org/).
Imputation of genotypes in the DP region was performed with MACH version 1.0 [9] with 1000 Genome Project data (1000G 2010-6 release, http://www.sph.umich.edu/csg/yli/mach/download/1000G-2010-06.html).
HLA-DPA1 allele imputation
The HLA-DP region was in strong linkage disequilibrium and some DPB1 alleles were known to be linked with particular DPA1 alleles. First, we imputed HLA-DPA1 alleles by using the actual genotype data of samples obtained from Illumina HumanHap550v3/610-Quad (Illumina) and 1000 Genome Project data of Asian origin (JPT+CHB) (http://www.sph.umich.edu/csg/abecasis/MaCH/download/1000G-2010-06.html). The accuracy of the imputated data was confirmed by direct sequencing. The error rate of imputation was 1/352 (0.003).
Supporting Information
Zdroje
1. KusunokiTMorimotoTNishikomoriRYasumiTHeikeT 2009 Changing prevalence and severity of childhood allergic diseases in kyoto, Japan, from 1996 to 2006. Allergol Int 58 543 548
2. PawankarRBunnagCChenYFukudaTKimYY 2009 Allergic rhinitis and its impact on asthma update (ARIA 2008)–western and Asian-Pacific perspective. Asian Pac J Allergy Immunol 27 237 243
3. MoffattMFKabeschMLiangLDixonALStrachanD 2007 Genetic variants regulating ORMDL3 expression contribute to the risk of childhood asthma. Nature 448 470 473
4. HimesBEHunninghakeGMBaurleyJWRafaelsNMSleimanP 2009 Genome-wide association analysis identifies PDE4D as an asthma-susceptibility gene. Am J Hum Genet 84 581 593
5. HancockDBRomieuIShiMSienra-MongeJJWuH 2009 Genome-wide association study implicates chromosome 9q21.31 as a susceptibility locus for asthma in mexican children. PLoS Genet 5 e1000623 doi:10.1371/journal.pgen.1000623
6. SleimanPMFloryJImielinskiMBradfieldJPAnnaiahK 2010 Variants of DENND1B associated with asthma in children. N Engl J Med 362 36 44
7. LiXHowardTDZhengSLHaselkornTPetersSP 2010 Genome-wide association study of asthma identifies RAD50-IL13 and HLA-DR/DQ regions. J Allergy Clin Immunol 125 328 335 e311
8. MoffattMFGutIGDemenaisFStrachanDPBouzigonE 2010 A large-scale, consortium-based genomewide association study of asthma. N Engl J Med 363 1211 1221
9. LiYWillerCSannaSAbecasisG 2009 Genotype imputation. Annu Rev Genomics Hum Genet 10 387 406
10. ImotoYEnomotoHFujiedaSOkamotoMSakashitaM 2010 S2554X mutation in the filaggrin gene is associated with allergen sensitization in the Japanese population. J Allergy Clin Immunol 125 498 500 e492
11. HuangHWLueKHWongRHSunHLSheuJN 2006 Distribution of allergens in children with different atopic disorders in central Taiwan. Acta Paediatr Taiwan 47 127 134
12. ShibasakiMNoguchiETakedaKTakitaH 1997 Distribution of IgE and IgG antibody levels against house dust mites in schoolchildren, and their relation with asthma. J Asthma 34 235 242
13. YuVCDelsertCAndersenBHollowayJMDevaryOV 1991 RXR beta: a coregulator that enhances binding of retinoic acid, thyroid hormone, and vitamin D receptors to their cognate response elements. Cell 67 1251 1266
14. CaraballoLMarrugoJJimenezSAngeliniGFerraraGB 1991 Frequency of DPB1*0401 is significantly decreased in patients with allergic asthma in a mulatto population. Hum Immunol 32 157 161
15. ChoiJHLeeKWKimCWParkCSLeeHY 2009 The HLA DRB1*1501-DQB1*0602-DPB1*0501 haplotype is a risk factor for toluene diisocyanate-induced occupational asthma. Int Arch Allergy Immunol 150 156 163
16. ChoiJHLeeKWOhHBLeeKJSuhYJ 2004 HLA association in aspirin-intolerant asthma: DPB1*0301 as a strong marker in a Korean population. J Allergy Clin Immunol 113 562 564
17. HowellWMStandringPWarnerJAWarnerJO 1999 HLA class II genotype, HLA-DR B cell surface expression and allergen specific IgE production in atopic and non-atopic members of asthmatic family pedigrees. Clin Exp Allergy 29 Suppl 4 35 38
18. ShibasakiMHoriTShimizuTIsoyamaSTakedaK 1990 Relationship between asthma and seasonal allergic rhinitis in schoolchildren. Ann Allergy 65 489 495
19. OvsyannikovaIGJacobsonRMVierkantRAO'ByrneMMPolandGA 2009 Replication of rubella vaccine population genetic studies: validation of HLA genotype and humoral response associations. Vaccine 27 6926 6931
20. OvsyannikovaIGRyanJEJacobsonRMVierkantRAPankratzVS 2006 Human leukocyte antigen and interleukin 2, 10 and 12p40 cytokine responses to measles: is there evidence of the HLA effect? Cytokine 36 173 179
21. YoshitakeSKimuraAOkadaMYaoTSasazukiT 1999 HLA class II alleles in Japanese patients with inflammatory bowel disease. Tissue Antigens 53 350 358
22. VarneyMDValdesAMCarlsonJANobleJATaitBD 2010 HLA DPA1, DPB1 alleles and haplotypes contribute to the risk associated with type 1 diabetes: analysis of the type 1 diabetes genetics consortium families. Diabetes 59 2055 2062
23. ZhouXLeeJEArnettFCXiongMParkMY 2009 HLA-DPB1 and DPB2 are genetic loci for systemic sclerosis: a genome-wide association study in Koreans with replication in North Americans. Arthritis Rheum 60 3807 3814
24. ZinoEFrumentoGMarktelSSormaniMPFicaraF 2004 A T-cell epitope encoded by a subset of HLA-DPB1 alleles determines nonpermissive mismatches for hematologic stem cell transplantation. Blood 103 1417 1424
25. KimuraAKitamuraHDateYNumanoF 1996 Comprehensive analysis of HLA genes in Takayasu arteritis in Japan. Int J Cardiol 54 Suppl S61 69
26. ThomsenSFDuffyDLKyvikKOSkyttheABackerV 2010 Relationship between type 1 diabetes and atopic diseases in a twin population. Allergy
27. TzengSTHsuSGFuLSChiCS 2007 Prevalence of atopy in children with type 1 diabetes mellitus in central Taiwan. J Microbiol Immunol Infect 40 74 78
28. PlengeRMSeielstadMPadyukovLLeeATRemmersEF 2007 TRAF1-C5 as a risk locus for rheumatoid arthritis–a genomewide study. N Engl J Med 357 1199 1209
29. PriceALPattersonNJPlengeRMWeinblattMEShadickNA 2006 Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 38 904 909
30. SladekRRocheleauGRungJDinaCShenL 2007 A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445 881 885
31. HiuraYTabaraYKokuboYOkamuraTMikiT 2010 A genome-wide association study of hypertension-related phenotypes in a Japanese population. Circ J 74 2353 2359
32. HaradaMNakashimaKHirotaTShimizuMDoiS 2007 Functional polymorphism in the suppressor of cytokine signaling 1 gene associated with adult asthma. Am J Respir Cell Mol Biol 36 491 496
33. HirotaTSuzukiYHasegawaKObaraKMatsudaA 2005 Functional haplotypes of IL-12B are associated with childhood atopic asthma. J Allergy Clin Immunol 116 789 795
34. SakashitaMYoshimotoTHirotaTHaradaMOkuboK 2008 Association of serum interleukin-33 level and the interleukin-33 genetic variant with Japanese cedar pollinosis. Clin Exp Allergy 38 1875 1881
35. KimHBKangMJLeeSYJinHSKimJH 2008 Combined effect of tumour necrosis factor-alpha and interleukin-13 polymorphisms on bronchial hyperresponsiveness in Korean children with asthma. Clin Exp Allergy 38 774 780
36. Yamaguchi-KabataYNakazonoKTakahashiASaitoSHosonoN 2008 Japanese population structure, based on SNP genotypes from 7003 individuals compared to other ethnic groups: effects on population-based association studies. Am J Hum Genet 83 445 456
37. DevlinBRoederK 1999 Genomic control for association studies. Biometrics 55 997 1004
38. PetittiD 2000 Meta-Analysis, Decision Analysis, and Cost-Effective Analysis Second Edition Second Edition Oxford university pres
39. ChenWLiangLAbecasisGR 2009 GWAS GUI: graphical browser for the results of whole-genome association studies with high-dimensional phenotypes. Bioinformatics 25 284 285
40. PruimRJWelchRPSannaSTeslovichTMChinesPS 2010 LocusZoom: regional visualization of genome-wide association scan results. Bioinformatics 26 2336 2337
41. PurcellSChernySSShamPC 2003 Genetic Power Calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics 19 149 150
42. WickhamH 2009 ggplot2: elegant graphics for data analysis Springer New York
Štítky
Genetika Reprodukčná medicína
Článek Pervasive Sign Epistasis between Conjugative Plasmids and Drug-Resistance Chromosomal MutationsČlánek Stress-Induced PARP Activation Mediates Recruitment of Mi-2 to Promote Heat Shock Gene ExpressionČlánek Histone Crosstalk Directed by H2B Ubiquitination Is Required for Chromatin Boundary IntegrityČlánek A Functional Variant at a Prostate Cancer Predisposition Locus at 8q24 Is Associated with ExpressionČlánek Replication and Explorations of High-Order Epistasis Using a Large Advanced Intercross Line PedigreeČlánek Expression of Tumor Suppressor in Spermatogonia Facilitates Meiotic Progression in Male Germ Cells
Článok vyšiel v časopisePLOS Genetics
Najčítanejšie tento týždeň
2011 Číslo 7- Gynekologové a odborníci na reprodukční medicínu se sejdou na prvním virtuálním summitu
- Je „freeze-all“ pro všechny? Odborníci na fertilitu diskutovali na virtuálním summitu
-
Všetky články tohto čísla
- Gene-Based Tests of Association
- The Demoiselle of X-Inactivation: 50 Years Old and As Trendy and Mesmerising As Ever
- Variants in and Underlie Natural Variation in Translation Termination Efficiency in
- SHH1, a Homeodomain Protein Required for DNA Methylation, As Well As RDR2, RDM4, and Chromatin Remodeling Factors, Associate with RNA Polymerase IV
- Genome-Wide Association Study Identifies as a Susceptibility Gene for Pediatric Asthma in Asian Populations
- Pervasive Sign Epistasis between Conjugative Plasmids and Drug-Resistance Chromosomal Mutations
- Genetic Anticipation Is Associated with Telomere Shortening in Hereditary Breast Cancer
- Identification of a Mutation Associated with Fatal Foal Immunodeficiency Syndrome in the Fell and Dales Pony
- Stress-Induced PARP Activation Mediates Recruitment of Mi-2 to Promote Heat Shock Gene Expression
- An Epigenetic Switch Involving Overlapping Fur and DNA Methylation Optimizes Expression of a Type VI Secretion Gene Cluster
- Recombination and Population Structure in
- A Rice Plastidial Nucleotide Sugar Epimerase Is Involved in Galactolipid Biosynthesis and Improves Photosynthetic Efficiency
- A Role for Phosphatidic Acid in the Formation of “Supersized” Lipid Droplets
- Colon Stem Cell and Crypt Dynamics Exposed by Cell Lineage Reconstruction
- Loss of the BMP Antagonist, SMOC-1, Causes Ophthalmo-Acromelic (Waardenburg Anophthalmia) Syndrome in Humans and Mice
- Interactions between Glucocorticoid Treatment and Cis-Regulatory Polymorphisms Contribute to Cellular Response Phenotypes
- Translation Reinitiation Relies on the Interaction between eIF3a/TIF32 and Progressively Folded -Acting mRNA Elements Preceding Short uORFs
- DAF-12 Regulates a Connected Network of Genes to Ensure Robust Developmental Decisions
- Adult Circadian Behavior in Requires Developmental Expression of , But Not
- Histone Crosstalk Directed by H2B Ubiquitination Is Required for Chromatin Boundary Integrity
- Proteins in the Nutrient-Sensing and DNA Damage Checkpoint Pathways Cooperate to Restrain Mitotic Progression following DNA Damage
- Complex Evolutionary Events at a Tandem Cluster of Genes Resulting in a Single-Locus Genetic Incompatibility
- () and Its Regulated Homeodomain Gene Mediate Abscisic Acid Response in
- A Functional Variant at a Prostate Cancer Predisposition Locus at 8q24 Is Associated with Expression
- LGI2 Truncation Causes a Remitting Focal Epilepsy in Dogs
- Adaptations to Endosymbiosis in a Cnidarian-Dinoflagellate Association: Differential Gene Expression and Specific Gene Duplications
- The Translation Initiation Factor eIF4E Regulates the Sex-Specific Expression of the Master Switch Gene in
- Somatic Genetics Empowers the Mouse for Modeling and Interrogating Developmental and Disease Processes
- Molecular Mechanisms Generating and Stabilizing Terminal 22q13 Deletions in 44 Subjects with Phelan/McDermid Syndrome
- Replication and Explorations of High-Order Epistasis Using a Large Advanced Intercross Line Pedigree
- Mechanisms of Chromosome Number Evolution in Yeast
- Regulatory Cross-Talk Links Chromosome II Replication and Segregation
- Ancestral Genes Can Control the Ability of Horizontally Acquired Loci to Confer New Traits
- Expression of Tumor Suppressor in Spermatogonia Facilitates Meiotic Progression in Male Germ Cells
- Rare and Common Regulatory Variation in Population-Scale Sequenced Human Genomes
- The Epistatic Relationship between BRCA2 and the Other RAD51 Mediators in Homologous Recombination
- Identification of Novel Genetic Markers Associated with Clinical Phenotypes of Systemic Sclerosis through a Genome-Wide Association Strategy
- NatF Contributes to an Evolutionary Shift in Protein N-Terminal Acetylation and Is Important for Normal Chromosome Segregation
- Araucan and Caupolican Integrate Intrinsic and Signalling Inputs for the Acquisition by Muscle Progenitors of the Lateral Transverse Fate
- Pathologic and Phenotypic Alterations in a Mouse Expressing a Connexin47 Missense Mutation That Causes Pelizaeus-Merzbacher–Like Disease in Humans
- Recombinant Inbred Line Genotypes Reveal Inter-Strain Incompatibility and the Evolution of Recombination
- Epistatic Relationships in the BRCA1-BRCA2 Pathway
- Genome-Wide Association Study Identifies Novel Restless Legs Syndrome Susceptibility Loci on 2p14 and 16q12.1
- Genetic Loci Associated with Plasma Phospholipid n-3 Fatty Acids: A Meta-Analysis of Genome-Wide Association Studies from the CHARGE Consortium
- Fine Mapping of Five Loci Associated with Low-Density Lipoprotein Cholesterol Detects Variants That Double the Explained Heritability
- CHD1 Remodels Chromatin and Influences Transient DNA Methylation at the Clock Gene
- Nonlinear Fitness Landscape of a Molecular Pathway
- Genome-Wide Scan Identifies , , and as Novel Risk Loci for Systemic Sclerosis
- Quantitative and Qualitative Stem Rust Resistance Factors in Barley Are Associated with Transcriptional Suppression of Defense Regulons
- A Systematic Screen for Tube Morphogenesis and Branching Genes in the Tracheal System
- PLOS Genetics
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Genome-Wide Association Study Identifies Novel Restless Legs Syndrome Susceptibility Loci on 2p14 and 16q12.1
- Loss of the BMP Antagonist, SMOC-1, Causes Ophthalmo-Acromelic (Waardenburg Anophthalmia) Syndrome in Humans and Mice
- Gene-Based Tests of Association
- Genome-Wide Association Study Identifies as a Susceptibility Gene for Pediatric Asthma in Asian Populations
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



