-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
A Research Agenda for Malaria Eradication: Health Systems and Operational Research
Health systems research and development is needed to support the global malaria eradication agenda. In this paper, we (the malERA Consultative Group on Health Systems and Operational Research) focus on the health systems needs of the elimination phase of malaria eradication and consider groupings of countries at different stages along the pathway to elimination. We examine the difference between the last attempt at eradication of malaria and more recent initiatives, and consider the changing health system challenges as countries make progress towards elimination. We review recent technological and theoretical developments related to health systems and the renewed commitment to strengthening health systems for universal access and greater equity. Finally, we identify a number of needs for research and development, including tools for analyzing and improving effective coverage and strengthening decision making and discuss the relevance of these needs at all levels of the health system from the community to the international level.
Published in the journal: A Research Agenda for Malaria Eradication: Health Systems and Operational Research. PLoS Med 8(1): e32767. doi:10.1371/journal.pmed.1000397
Category: Review
doi: https://doi.org/10.1371/journal.pmed.1000397Summary
Health systems research and development is needed to support the global malaria eradication agenda. In this paper, we (the malERA Consultative Group on Health Systems and Operational Research) focus on the health systems needs of the elimination phase of malaria eradication and consider groupings of countries at different stages along the pathway to elimination. We examine the difference between the last attempt at eradication of malaria and more recent initiatives, and consider the changing health system challenges as countries make progress towards elimination. We review recent technological and theoretical developments related to health systems and the renewed commitment to strengthening health systems for universal access and greater equity. Finally, we identify a number of needs for research and development, including tools for analyzing and improving effective coverage and strengthening decision making and discuss the relevance of these needs at all levels of the health system from the community to the international level.
Introduction
The last attempt at (global) eradication of malaria, which lasted from 1955 to approximately 1969, depended on vertical operations (centrally organized activities not linked to subnational administrative levels and/or communities). These operations—largely indoor residual spraying—often bypassed health systems, because it was assumed that they could be run most efficiently with minimal collaboration with general health services, which were often poorly developed in endemic areas. In the later phases of the first eradication era, it became clear that some form of chemotherapy was needed to reduce transmission, and that good surveillance was essential for achieving and maintaining malaria-free status in a given area. Increased attention was then given to integration with existing health services and to using malaria eradication strategically to build rudimentary health services in remote areas [1],[2].
Here, we examine the health systems research and development that is necessary to support a global malaria eradication agenda. We do not address broader macroeconomic and health system development needs, even though addressing them would be beneficial to all agendas. We focus on the elimination phase of the eradication agenda and considers groupings of countries at different stages along the pathway to elimination.
On the basis of previous experiences with malaria and other diseases for which eradication has been attempted, we use standard definitions for control, elimination, and eradication throughout this article (Box 1) [3]. Importantly, these definitions emphasize the need for continued interventions for both malaria control and elimination.
Box 1. Definitions of Control, Elimination, and Related Concepts [3]
Control: Reduction of disease incidence, prevalence, morbidity, or mortality to a locally acceptable level as a result of deliberate efforts; continued intervention measures are required to maintain control.
Elimination of disease: Reduction to zero of the incidence of a specified disease in a defined geographic area as a result of deliberate efforts; continued intervention measures are required.
Elimination of infection: Reduction to zero of the incidence of infection caused by a specific agent in a defined geographic area as a result of deliberate efforts; continued measures to prevent reestablishment are required.
Eradication: Permanent reduction to zero of the worldwide incidence of infection caused by a specific agent as a result of deliberate efforts; intervention measures are no longer needed.
Extinction: The specific infectious agent no longer exists in nature or the laboratory.
The Health System
In 2000, The World Health Organization (WHO) articulated a comprehensive definition of health systems that is now widely adopted. A health system “consists of all organizations, people and actions whose primary intent is to promote, restore or maintain health” [4] with goals of “improving health and health equity in ways that are responsive, financially fair and make the best, or most efficient, use of available resources.” In 2007, WHO developed a conceptual framework comprising six “health system building blocks” that has also been widely adopted (Box 2) [5].
Box 2. The Six Health System Building Blocks [5]
-
Governance: (including leadership) ensuring strategic policy frameworks combined with effective oversight, coalition building, accountability, transparency, regulations, incentives, and attention to system design
-
Health workforce: responsive, fair, and efficient given available resources and circumstances, and available in sufficient numbers
-
Health financing: raising adequate funds for health in ways that ensure people can use needed services and are protected from financial catastrophe or impoverishment associated with having to pay for them
-
Health technologies: including medical products, vaccines, diagnostics, and other technologies of assured quality, safety, efficacy, and cost-effectiveness
-
Health information: ensuring the production, analysis, dissemination, and use of reliable and timely information on health determinants, health systems performance, and health status
-
Service delivery: including effective, safe, and quality personal and nonpersonal health interventions that are provided to those in need, when and where needed (including infrastructure), with a minimal waste of resources
This framework has now been further elaborated [6] to include the role of people, not just at the centre of the system as mediators and beneficiaries, but as key actors in driving the system itself. Thus, the framework includes the participation of people as individuals and in civil society organizations and stakeholder networks, which influence each of the building blocks. Placing people and their institutions at the centre of this framework emphasizes WHO's renewed commitment to the principles and values of primary health care—fairness, social justice, participation, and intersectoral collaboration (see Figure 1).
Fig. 1. Health system building blocks [7]. ![Health system building blocks <em class="ref">[<b>7</b>]</em>.](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image/e79ac3c5a987901ceafcf895f30a9779.png)
Image credit: Fusión Creativa. Currently, three revolutions are under way that will transform health systems: the biotechnology revolution, the communications and information technology revolution, and the systems thinking. Systems thinking is a holistic approach to analysis that focuses on the emergent behaviour of complex systems. It analyzes how a system's constituent parts interrelate and how systems work over time and within the context of larger systems. Applied to problem solving, systems thinking addresses the dynamic, mainly nonlinear linkages, interactions, and behaviours among the elements of the entire system. Systems thinking as developed and used for other complex systems is now being applied in health systems [7] and is essential for understanding what works, for whom, to what extent, and under what circumstances. It also helps predict and mitigate possible unintended consequences of particular actions and to exploit synergies from concerted action in the system. The promotion and application of systems thinking will be very timely as the malaria eradication agenda develops.
Health Systems for Malaria Control, Elimination, and Eradication
The Global Malaria Action Plan (GMAP) was launched in 2008 by the Roll Back Malaria partnership against a background of greatly increased investment in research and development for malaria-control technologies since 1999 and extraordinary increases in funding for malaria control through national and global financing mechanisms since 2002 [8]. The GMAP includes three phases. The first phase—scaling-up for impact—aims to rapidly reach universal coverage for all populations at risk with locally appropriate malaria-control interventions, supported by strengthened health systems. The second phase—sustained control—aims to prevent the resurgence of malaria by maintaining universal intervention coverage until countries enter the elimination stage. In the final phase—elimination and eradication—it is estimated that more than 20 lower burden countries around the world will be poised to eliminate malaria.
There is currently a broad global consensus on malaria-control strategies, and almost all malaria-endemic countries now have national malaria programmes in line with GMAP. Malaria indicators (both for coverage and health impact) are moving in the right direction in many countries [9]. However, progress in most endemic countries is slower than it could be, given the available financial resources. Among the main reasons for the suboptimal pace are constraints to the delivery of essential malaria interventions at effective coverage levels and quality to populations in need [9]–[11]. There is no doubt that success in moving towards eradication will be heavily dependent on health systems [12],[13].
Some of the health system challenges in a country facing a huge malaria burden and in a country on the brink of phasing out the disease are similar, but such countries also pose different health system challenges. For example, quality case management is needed in all phases. In contrast to most other diseases for which elimination is being considered, the symptoms of malaria are nonspecific. Furthermore, treatment needs to start soon after symptoms appear both to prevent the development of severe disease and death and, particularly in areas where malaria prevalence is low, to help reduce transmission. The capacity to diagnose and provide early and effective treatment is therefore needed wherever there is a malaria risk. Achieving this capacity requires quality coverage of general health services and is an important systemic challenge for any antimalaria programme.
By contrast, although survey data can be useful for gauging progress in highly endemic areas, disease surveillance becomes increasingly important as the disease burden is lowered. Highly sensitive and dynamic surveillance becomes the crucial element in the pre-elimination phase and after [14]. Again, this capacity can only be achieved by a solid articulation between a specialized programme and functional general health services.
Finally, although the integration (or at least coordination) of malaria vector control and other preventive interventions with other health programmes can be synergistic and efficient in many settings, such integration becomes less efficient as progress makes malaria an increasingly focal and epidemic disease. Thus, malaria preventive interventions can sometimes be managed independently from general health services but these operations nevertheless depend on fundamental health system elements such as policy and governance, human resources, financing, supplies, and monitoring.
Much progress has been made in recent years towards understanding health systems better and the importance of strengthening them. The result is that global health initiatives are providing increased funding for national health systems to accelerate progress on universal access to essential health interventions, including malaria interventions. New initiatives such as the Task Force on Innovative Financing for Health Systems [15], and initiatives from the Global Fund to Fight Aids, Tuberculosis and Malaria (GFATM), Global Alliance for Vaccines and Immunization (GAVI), WHO, World Bank Joint Platform for Health Systems Strengthening, and President Obama's Global Health Initiative are evidence of the growing momentum in favour of health system strengthening. At the same time, there is also an increased emphasis on health systems research. During the last attempt at malaria eradication, research, including health systems research, was neglected because it was assumed that rapid, uniform spraying operations would lead to eradication. More recent successful malaria disease and control programmes have been notable for including research as a critical element [2],[11],[16].
Health Systems Effectiveness
As an original approach to understanding health system impediments to sustaining malaria interventions at coverage levels sufficient to reduce malaria morbidity and mortality to very low levels, and to achieve and maintain malaria-free status, we introduce the concept of health systems effectiveness. We used this concept and a framework for analyzing constraints to scale-up (see below) as “stepping stones” during our development of a health systems research and development agenda.
Malaria control and elimination depend in equal measure on high-performance health systems that can deliver malaria interventions at high and equitable levels of quality and with effective coverage. In this context, effective coverage goes beyond the usual notion of population access to include provider compliant delivery, patient adherence, and individual benefit from the intervention [17]. Effective coverage requires the concerted strength of all the health system building blocks. When effective coverage levels are inadequate or inequitable, the reasons are nearly always interacting failures across the building blocks. To pinpoint where system interventions and strengthening will be effective and efficient, programme managers need to be able to diagnose those problems and their determinants and interactions.
Figure 2 provides a graphical representation of the systems effectiveness framework and shows how an initially high intervention efficacy translates into low effectiveness in the real world because of system-specific issues of suboptimal intervention access, inadequate programme targeting because of diagnostic shortcomings, incomplete provider compliance, and client adherence.
Fig. 2. Graphical representation of the systems effectiveness framework. 
How interventions lose traction in health systems: example of artemisinin-based combination therapy (ACT) antimalarial treatment in Rufiji Demographic Surveillance Area Tanzania in 2006. Source: INDEPTH INESS Project. Systems Effectiveness Module, Swiss Tropical and Public Health Institute with data from Ifakara Health Institute and US Centers for Disease Control and Prevention based on [45]–[47]. Image credit: Fusión Creativa. District health system observatories are being established in Burkina Faso, Ghana, Mozambique, and Tanzania to determine their respective health systems' effectiveness in delivering artemisinin-based combination therapies (ACTs) [18], and research projects are starting to use the health systems effectiveness framework to analyze the determinants of coverage [19]. However, the results of these research projects have yet to be translated into strategically targeted health system–strengthening interventions and programme corrections.
A final stepping stone we used to develop the research agenda outlined in this paper is the framework for analyzing constraints to scale-up, developed for the Commission for Macroeconomics and Health [20]. This framework illustrates how barriers to expanding coverage of essential health services operate at all levels of the health system, from communities and households, through to cross-sectoral and sociopolitical levels, and thus suggests that interventions to address these barriers may need to operate at multiple levels.
Towards a Systems Research and Development Agenda
The health systems research and development agenda that our group has developed derives from the ideas and concepts discussed above and proposes the creation of a set of tools for applying the systems effectiveness framework for malaria elimination and control in different health system settings. The agenda is organized both across health system levels (community, facility, district, national, regional/global, and intersectorial; more details of these levels are given later) and health system building blocks (see Box 2), but, importantly it also takes account of “country groupings.” These groupings are relevant to the phases defined in the GMAP and we discuss them here in some detail before presenting our research and development agenda in full.
We suggest that the following grouping of countries is used to identify the most relevant health system research agendas for individual countries.
Group 1 includes countries where most of the population lives in areas where malaria elimination is considered impossible with existing tools. Currently, most of these countries are scaling up malaria-control efforts and some are entering the sustained control phase. This group includes most countries of sub-Saharan Africa and Papua New Guinea. In these countries, which have large areas with very intense malaria transmission, it is generally assumed that malaria elimination will only be possible though the large-scale application of new tools, which are still to be developed. Most likely such new tools will need to be applied in combination with existing ones, and the health system requirements for the effective delivery of these tools will probably be similar to those of current malaria-control interventions. Therefore, although undertaking systems research from the perspective of elimination is likely to be unproductive in group 1 countries, addressing current health system constraints on malaria control will almost certainly prove crucial for any future elimination efforts.
Group 2 includes countries with focal malaria, where a large part of the population lives in malaria-free areas, and where research aimed at health system strengthening is likely to play a crucial role in interrupting transmission in many of the existing foci. Many of these countries have diverse and complex health system challenges. This group includes most of the malaria-endemic countries in South and Central America, middle South Asia, and Southeast Asia. In sub-Saharan Africa, it includes southern Africa, the Horn, and the northern part of Sudan. It corresponds closely to the GMAP group designated as “control: low contribution to global deaths” [9], but includes additional countries such as Bangladesh, India, Indonesia, and Nepal.
Group 3 includes countries that are elimination ready. This group is almost identical to the “pre-elimination and elimination” countries in the World Malaria Report [9] and includes Argentina, Mexico, most of the countries of the Middle East and Central Asia, Central China, and possibly Sri Lanka, Vanuatu, and the Solomon Islands. In these countries, health system issues are generally not a crucial impediment to elimination, not necessarily because the health systems are exceptionally strong but often because the country's malaria problem has always been relatively easy to tackle with existing technologies due to intrinsic biologic (e.g., vectorial capacity or efficiency) or socioeconomic and development (e.g., improved housing) factors. However, review of the road to elimination in these countries with the identification of crucial health system determinants could provide valuable lessons, so international collaborations/global initiatives should focus on learning from past experiences rather than undertaking direct support or capacity strengthening.
This grouping of countries is intended to be specific to the malaria eradication health systems research agenda. A comprehensive listing of countries by these groupings has been avoided because many countries have areas belonging to more than one of these categories; this heterogeneity by itself presents policy and implementation challenges. Furthermore, the boundaries between groups are imprecise, and some countries could move from one group to another within few years.
What Goals and Needs Should the malERA Health Systems Research and Development Agenda Include?
From our discussions, we propose that the malERA health systems research and development agenda should consider the critical/transformational and conditional/situation goals and needs described in detail in Table 1. Some of these goals and needs are also partly covered in other papers in this series. For example, the need for tools to reduce unacceptably and avoidably low effective coverage of essential malaria interventions and malaria surveillance is also partly covered by the Monitoring and Evaluation and Surveillance malERA consultative group [21], the need for decision support tools to remove policy decision uncertainty for when to commit to transitioning from control to elimination is also covered in part by the malERA Consultative Groups on Modeling and Cross-Cutting Issues [22],[23], and the need for a tool to determine the kind and mix of integrated interventions that are cost-effective in differing epidemiologic and health system contexts is covered in part by the malERA Consultative Group on Modeling [22].
Tab. 1. Categorization of the malERA health systems research goals and approaches. 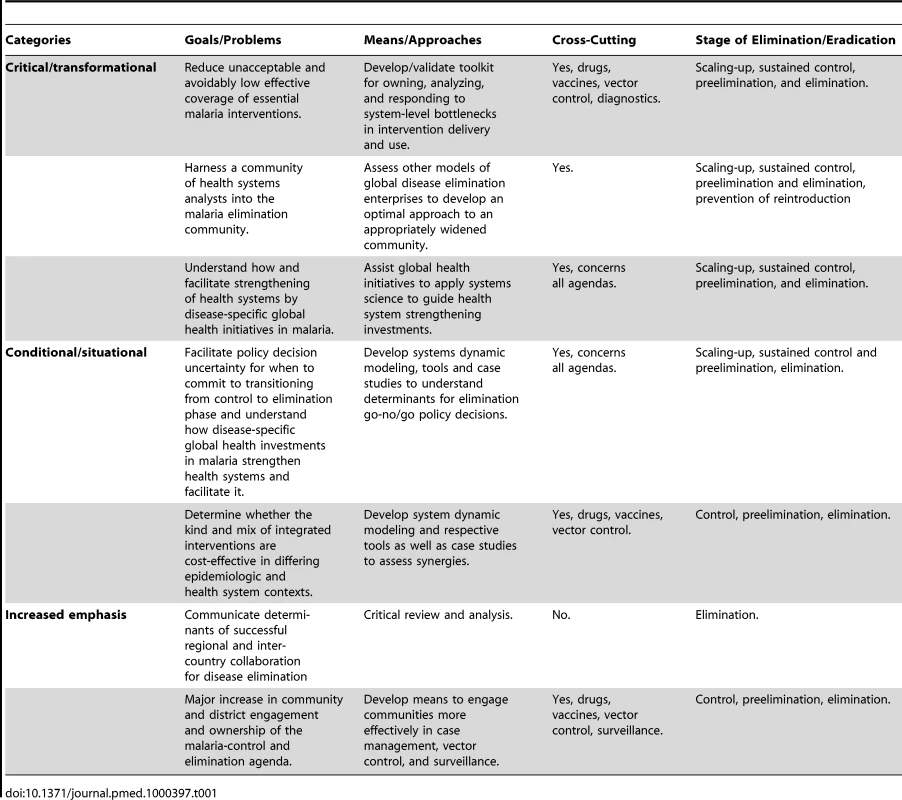
What Research Questions Must Be Asked to Satisfy Health Systems Needs and Goals?
The research questions that emerge from this above analysis are presented in Table 2 in a matrix of health system levels and health system building blocks. Below, we discuss these questions in greater detail arranged by health system organizational level. As in Table 2, when no country grouping is specified, the discussion refers to both group 1 and group 2 countries.
Tab. 2. Matrix of health systems research and development needs. 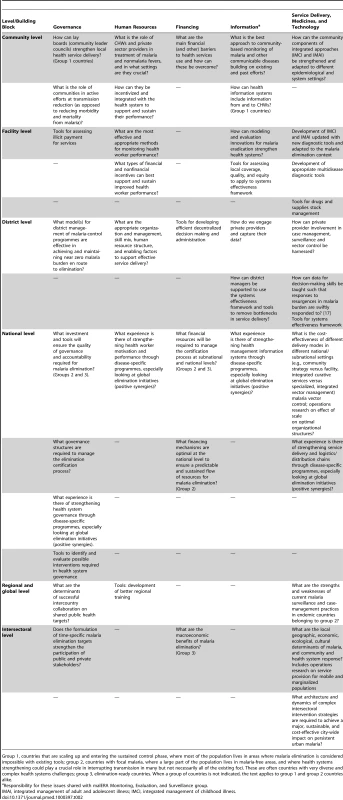
Group 1, countries that are scaling up and entering the sustained control phase, where most of the population lives in areas where malaria elimination is considered impossible with existing tools; group 2, countries with focal malaria, where a large part of the population lives in malaria-free areas, and where health systems strengthening could play a crucial role in interrupting transmission in many but not necessarily all of the existing foci. These are often countries with very diverse and complex health systems challenges; group 3, elimination-ready countries. When a group of countries is not indicated, the text applies to group 1 and group 2 countries alike. Community Level
Past experience indicates that fixed health facilities cannot reach all those in need, and that extending the reach of services is essential to achieve universal and equitable coverage with interventions for malaria and other diseases. Community health workers (CHWs) and home management of fevers (which has been well documented in Africa) offer possible approaches. Several examples of CHW initiatives are emerging from countries as varied as India, Sri Lanka, Ethiopia, and Uganda [24],[25]. More needs to be done to capture and share the experience gained from these programmes, and to ensure that opportunities are taken to evaluate the effectiveness of different approaches to designing and implementing CHW programmes.
A range of community-level factors affects the ability of health systems to reach the population effectively, particularly groups that are located far from formal health facilities and/or are mobile. Some of these factors reflect the conventional barriers to access—financial, physical/geographic, and social [26], but a better understanding is needed of how community-level factors influence use in particular settings, and how they can be addressed in the context of malaria-control and elimination measures.
In the past, some community health programmes failed because they did not recognize the need to compensate CHWs for time spent delivering services, and because they were not sufficiently linked into and supported by the health systems' “higher” levels [27],[28]. There is a rich literature on CHW systems that should be exploited, but given rapid changes—such as the greatly improved levels of education and the proliferation of private providers in many areas—continued experimentation with different approaches is needed to sustain CHW performance and motivation, including different forms of health facility support (for example, supervision). Better ways of integrating CHWs' results into health information and surveillance systems and ensuring that they receive information from these systems also need investigating. Furthermore, as malaria transmission falls and countries enter the elimination phase, it will become critical that malaria surveillance systems improve their coverage to include data from whichever services are used by people at risk [21]. Finally, diagnostic and other tools for use at the community level that are implemented as part of integrated strategies for managing illness, such as the Integrated Management of Childhood Illness (IMCI) and Integrated Management of Adult and Adolescent Illness (IMAI) strategies, have the potential to create quantum leaps in service and need to be adapted through research to the changing malaria epidemiological context. Unfortunately, few, if any, of these strategies are being systematically promoted in malaria risk areas in category 2 countries.
Facility Level
The health facility is the main point of contact with the health system for many people with fever, although private and informal providers are also important in many settings. It is also the focal point for collection, and ideally, use of data gathered through routine health management information systems. Many health systems face the challenge of ensuring that health workers are present in health facilities, have the required training and knowledge, are equipped with the relevant drugs and other supplies, and are motivated to use these resources to provide high-quality and responsive care that follows national policies and standards.
New research is needed on how best to improve health worker performance [29],[30]. A range of potential policy interventions has been suggested, including the traditional approaches of training and supervision, performance-based pay, bottom-up approaches using community accountability structures, and interventions addressing the mindset of health workers [31]. Other than training, the evidence about what works best and in what contexts is very limited, and deserves urgent attention.
Critically, interventions to improve health worker performance need to recognize the interconnectedness of the different health system building blocks. The design of pay-for-performance schemes, for example, involves questions of how best to govern such arrangements and the role of the community in these schemes, what the form and level of payments to health workers should be, and the source of funding, how to use the health information system to measure performance, how to ensure that complementary inputs such as training and supplies are coordinated and sustained, and how to avoid the risk that incentives may distort targets and divert attention from nontargeted services. Research on health worker performance should be multidisciplinary, therefore, and needs to recognize the complexity of possible interventions.
Research that focuses on developing new tools for assessing coverage, quality, and equity at the facility level that can be used to monitor health facility performance and analyze system effectiveness is also needed. Such tools are essential to identify bottlenecks that may impede malaria elimination efforts. In the context of malaria elimination activities, the development of surveillance systems and the development of ways to monitor their performance require highest attention.
In some settings, a significant amount of treatment seeking for fever takes place outside public sector facilities, through private health providers, pharmacies, and shops. The engagement of such providers has mainly been done in limited malaria intervention projects rather than in programmes, and most of the literature concerns the pre-artemisinin-based combination therapy–rapid diagnostic test (ACT-RDT) era [32]. More research is therefore needed on approaches to quality assurance that will ensure that these facilities/providers adhere to guidelines [33], and are covered by systems for gathering surveillance data.
District Level
The district is the initial coordination hub for delivering services and commodities to people (through health facilities and community programmes). The district is therefore the focal point for priority setting, resource allocation, financial administration, supply chain management, accountability for health worker performance, engagement of the private sector, surveillance and response, and monitoring, evaluation, and information management.
Some of the critical bottlenecks in malaria-control operations currently stem from weaknesses at the district level for the above operations. These bottlenecks result in inequitable or irrational financial distribution, frequent stock-outs, poor-quality services, and inefficient disease-control operations. The enhancement of district-level system operations will therefore contribute significantly to reducing effectiveness losses for interventions, and increase the cost-effectiveness of programmes. Although there has been substantial investment in district-strengthening approaches and tools, these have not been as productive as they could be for a variety of reasons, such as insufficient decentralization and lack of information feedback. Innovations in information, communication, and decision-support tools (biometrics, bar coding, mobile phones and texting, computerized logistics systems, server-based data systems, among others) have the potential to improve district health systems in a cost-effective manner.
The systems challenges at the district level are common to group 1 and 2 countries. However, in group 1 countries they may be almost universal in rural areas, whereas in group 2 countries, systems challenges may only be considerable in the most malaria-endemic areas where deep poverty, difficult terrain, and various social barriers converge. Thus, district-strengthening efforts need to be more targeted in group 2 than in group 1 countries. Furthermore, in group 1 countries, the primary challenge is to enable the health system to achieve universal coverage of malaria-control interventions and to optimize their use (thereby reducing effectiveness losses), whereas in group 2 countries and in group 1 countries where the malaria burden has decreased, the challenge at the district level is increasingly to enable the system to respond to the technical demands of elimination. This challenge requires a greater focus on real-time information management and response and so, in these settings, research data that is relevant to developing decision-making skills will be critical.
National Level
Ultimately, the decision to embark on malaria elimination rests at the national level even if malaria elimination applies to only a region of the country. Such decisions must be based on operational and technical feasibility, as well as regional economic and political considerations [34].
Group 2 countries are more likely to have had some historical or more recent regional experiences with malaria elimination, and may see elimination as a “completeness exercise” or as an entry point to strengthening the systems response to address the health needs of neglected areas or population groups [35]. In some group 1 countries, elimination may be possible in specific areas. Generally, elimination targets for provinces, regions, or other administrative units that are highly developed and already close to malaria-free status may be sensible and justified from a regional viewpoint but of little importance from a national health perspective (e.g., Zanzibar in Tanzania, Goa in India). By contrast, national elimination targets—provided they are realistic—may provide strategic leverage for improving health equity at the national level.
The overriding research questions at the national level must be directed towards defining the best possible arrangements for governance, structural and functional organization between the system and malaria-specific programmes, and must be directed towards determining the implications of malaria elimination for cross-border political dialogue and arrangements with neighbouring countries. Models for financial sustainability also need to be established. These issues will be relevant in group 1, 2, and 3 countries, and through all the phases of disease control, elimination, certification, and prevention of reintroduction. An analytical review of past elimination programmes for other diseases—both successes and failures—with these questions in mind would be helpful. A recently published review provides useful information on interactions between global health initiatives and country health systems [36], but there are obvious differences between initiatives for reducing major disease burdens and elimination activities, which aim at small burdens.
Regional/Global Level
WHO recently revised its guidelines on malaria elimination and certification, emphasizing the need for regional intercountry collaboration [37]. In recent years, cross-border collaboration for malaria control has been inefficient in contrast to, for example, collaboration on polio elimination. Therefore, experiences from these successful intercountry collaborations and malaria-control initiatives should be mapped to provide a better evidence base for strengthening the intercountry collaboration needed to achieve national elimination targets.
An issue that will and should be addressed is subnational elimination. While any country is free to certify any area as malaria-free, WHO needs data on the achievement and maintenance of subnational areas of malaria elimination to develop guidance so that countries are spared the embarrassment of declaring an area malaria-free only to have transmission be detected soon after.
In addition, the current malaria surveillance and case-management practices of a sample of countries should be investigated and mapped by health systems research groups that are external to and independent of the malaria-control/elimination programme (see [21]).
Intersectoral Collaboration
The engagement of sectors other than health is sometimes but not always important for malaria control and elimination. The importance of intersectoral collaboration is determined by the extent to which other sectors are responsible for causing a local malaria problem through environmental change or population movement, and by whether a particular sector, such as education, plays a crucial role in achieving elimination. There is an extensive literature on the influence of development projects on malaria (e.g., [38]) and on integrating health considerations in programme planning (e.g., [39],[40]). Serious difficulties can be expected where population movements related to natural and man-made disasters and conflict occur, in situations where “spontaneous” population movements related to traditional economies (for example, nomadism, transhumance) occur, and in urban areas where a multitude of actors make it difficult to identify the most important partners, where there is often less social cohesion, and where indoor residual spraying is often not possible.
Situations such as these have proven resilient to malaria control and elimination efforts over several decades. Mobile populations that are exposed to malaria, especially in or near forested areas in Latin America and South and Southeast Asia, often belong to ethnic minority groups and are subjected to various political and economic pressures. Interdisciplinary research (geographical, ecological, economic, social) and trials of different service delivery modes have proven useful in, for example, the Amazon, Thailand, and Vietnam [41]–[43]. Such research is needed in many more areas to validate for local adaptations of approaches in specific settings.
Urban malaria is a specific problem on the Indian subcontinent [44] where it needs to be investigated in all its dimensions from entomology to basic human ecology, and from household and industrial politics to local, municipal, and national level politics.
Concluding Remarks
In our discussions and in this article we have identified and characterized the major health systems needs relevant to the elimination of malaria and have articulated key research questions that need to be addressed at various health systems levels. In Box 3, we present the summary of the research and development agenda for health systems and operational research that resulted from our discussions. With malaria elimination on the agenda, one important, generic question needs to be addressed through health systems research. To what extent does an explicit target of malaria elimination motivate other sectors to participate in malaria control? If research evidence shows that such an explicit target is a potent motivator of other sectors, then ministries of health might be more inclined to be highly vocal and explicit about elimination targets and about the possible consequences of not meeting these targets.
Box 3. Summary of the Research and Development Agenda for Health Systems and Operational Research
Overarching issue:
Development and validation of a tool kit for the national and subnational level, comparable to rapid assessment procedures, allowing (i) effectiveness decay analysis for identifying bottlenecks for effective coverage of malaria interventions and (ii) decisions on the degree of integration of interventions into existing and strengthened health systems.
Priority health systems research questions:
-
At the health facility level, how can health worker performance and compliance with best practice be monitored, enhanced, and sustained?
-
At the district level, what are the factors impeding greater application of existing tools and approaches to district health system strengthening including surveillance?
-
At the national level, what experience is there of strengthening health system components using disease-specific programmes?
-
At the regional/global level, what are the strengths and weaknesses of current malaria surveillance and patient management practices in malaria-endemic countries and what are the likely determinants of success of intercountry collaboration for disease elimination?
These research questions need to be defined locally but are of relevance to all programmes engaged in control or elimination
Zdroje
1. GramicciG
BealesPF
1988 The recent history of malaria control and eradication.
WernsdorferWH
McGregorSI
Principles and practice of malariology Edinburgh Churchill Livingstone 1335 1420
2. NájeraJA
2001 Malaria control: Achievements, problems and strategies. Parassitologia 43 1 89
3. DowdleWR
HopkinsDR
1997 The eradication of infectious diseases, Dahlem Workshop Report. Chichester John Wiley & Sons
4. WHO 2000 World health report 2000 – Health systems: Improving performance. Geneva World Health Organization
5. WHO 2007 Everybody's business: Strengthening health systems to improve health outcomes: WHO's Framework for Action. Geneva World Health Organization
6. WHO 2008 World health report 2008 – Primary health care: More than ever. Geneva World Health Organization
7. de SavignyD
AdamT
2009 Health systems thinking for health systems strengthening. Geneva World Health Organization
8. Roll Back Malaria Partnership 2008 The Global Malaria Action Plan. For a Malaria Free World. RBM: Geneva. Available: http://www.rollbackmalaria.org/gmap/
9. WHO 2009 World malaria report 2009. Geneva World Health Organization
10. BryceJ
TerreriN
VictoraCG
MasonE
DaelmansB
2006 Countdown to 2015: Tracking intervention coverage for child survival. Lancet 368 1067 1076
11. WebsterJ
HillJ
LinesJ
HansonK
2007 Delivery systems for insecticide treated and untreated mosquito nets in Africa: Categorization and outcomes achieved. Health Pol Plan 22 277 293
12. TannerM
de SavignyD
2008 Malaria eradication back on the table. Bull WHO 86 82 83
13. MillsA
RasheedF
TollmanS
2006 Health system strengthening.
JamisonDT
BremanJG
MeashamAR
AlleyneG
AlleyneG
Disease control priorities in developing countries, 2nd edition New York Oxford University Press and World Bank
14. HayS
SmithD
SnowR
2008 Measuring malaria endemicity from intense to interrupted transmission. Lancet Infect Dis 8 369 378
15. International Health Partnership 2010 Leaders commit new finance to tackle women's and children's health in the developing world. Available: http://www.internationalhealthpartnership.net/en/taskforce. 25 June 2010
16. AlilioMS
BygbjergIC
BremanJG
2004 Are multilateral malaria research and control programs the most successful? Lessons from the past 100 years in Africa. Am J Trop Med Hyg 71 268 278
17. LozanoR
SolizP
GakidouE
Abbott-KlafterJ
FeehanDM
2006 Benchmarking of performance of Mexican states with effective coverage. Lancet 368 1729 1741
18. INDEPTH Network Effectiveness and Safety Studies Project (INESS). Available: http://www.indepth-network.org/iness/index.php
19. BeerN
AliAS
de SavignyD
Al-MafazyAW
RamsanM
2010 System effectiveness of a targeted free mass distribution of long lasting insecticidal nets in Zanzibar, Tanzania. Malar J 9 173
20. WHO 2001 Commission on Macroeconomics and Health. Geneva World Health Organization
21. The malERA Consultative Group on Monitoring, Evaluation, and Surveillance 2011 A research agenda for malaria eradication: Monitoring, evaluation and surveillance. PLoS Med 8 e1000400 doi:10.1371/journal.pmed.1000400
22. The malERA Consultative Group on Modeling 2011 A research agenda for malaria eradication: Modeling. PLoS Med 8 e1000403 doi:10.1371/journal.pmed.1000403
23. The malERA Consultative Group on Integration Strategies 2011 A research agenda for malaria eradication: cross cutting issues for eradication. PLoS Med 8 e1000404 doi:10.1371/journal.pmed.1000404
24. HainesA
SandersD
LehmannU
RoweAK
LawnJE
2007 Achieving child survival goals: Potential contribution of community health workers. Lancet 369 2121 2131
25. StaedkeSG
MwebazaN
KamyaMR
ClarkTD
DorseyG
2009 Home management of malaria with artemether-lumefantrine compared with standard care in urban Ugandan children: A randomised controlled trial. Lancet 373 1623 1631
26. HetzelMW
ObristB
LengelerC
MsechuJJ
NathanR
2008 Obstacles to prompt and effective malaria treatment lead to low community-coverage in two rural districts of Tanzania. BMC Public Health 8 317
27. SegallM
2003 District health systems in a neoliberal world: A review of five key policy areas. Int J Health Plan Manag 18 S5 S26
28. WaltG
2005 Commentary: lay health workers in primary and community health care. Int J Epidemiol 34 1251
29. RoweAK
de SavignyD
LanataCF
VictoraCG
2006 How can we achieve and maintain high-quality performance of health workers in low-resource settings? The Lancet 366 1026 1035
30. RoweAK
OnikpoF
LamaM
DemingMS
2010 The rise and fall of supervision in a project designed to strengthen supervision of Integrated Management of Childhood Illness in Benin. Health Pol Plan 25 125 134
31. MaestadO
SchellenbergJ
HansonK
2009 A research agenda for improving health worker performance. London London School of Hygiene & Tropical Medicine
32. GoodmanC
BriegerW
UnwinA
MillsA
MeekS
2007 Medicine sellers and malaria treatment in sub-Saharan Africa: What do they do and how can their practice be improved? Am J Trop Med Hyg 77 203 218
33. AdeyiO
AtunR
2009 Innovating for impact: The Affordable Medicines Facility-malaria (AMFm). Nat Med 15 991
34. FeachemRGA
The Malaria Elimination Group 2009 Shrinking the malaria map: a guide on malaria elimination for policy makers. San Francisco University of California, San Francisco
35. WHOEMRO
2007 Malaria in Morocco: Relentless efforts towards the goal of elimination. Geneva: WHO EMRO. Available: http://www.emro.who.int/publications/Book_Details.asp?ID=813. Accessed 25 June 2010
36. WHO Maximizing Positive Synergies Collaborative Group 2009 An assessment of interactions between global health initiatives and country health systems. Lancet 373 2137 2169
37. WHOGMP
2007 Malaria elimination. A field manual for low and moderate endemic countries. Geneva World Health Organization
38. Service MW 1991 Agricultural development and arthropod-borne diseases: A review. Revista de Saúde Pública 25 165 178
39. BirleyMH
GomesM
DavyA
1997 Health aspects of environmental assessment. Environmental Assessment Sourcebook Update 18. Washington (D.C.) Environmental Division, World Bank
40. WHO 1982 Manual on environmental management for mosquito control, with special emphasis on malaria vectors. WHO Offset Publication number 66. Geneva World Health Organization
41. PeetersGK
XuanXN
VanBW
DucTN
RiberaJM
2010 Low perception of malaria risk among the Ra-glai ethnic minority in south-central Vietnam: Implications for forest malaria control. Malar J 9 23
42. SawyerD
1993 Economic and social consequences of malaria in new colonization projects in Brazil. Soc Sci Med 37 1131 1136
43. Singhanetra-RenardA
1986 Population movement, socio-economic behavior and the transmission of malaria in northern Thailand. Southeast Asian J Trop Med Public Health 17 396 405
44. RaoR
1984 The anophelines of India. New Delhi Malaria Research Centre, India Council of Medical Research
45. TannerM
1990 Von der Tropenmedizin zur Medizin in den Tropen - Prioritäten bei der Bekämpfung übertragbarer Erkrankungen [From tropical medicine to medicine in the tropics – priorities in the control of communicable diseases]. Therapeut Umschau 47 856 863
46. VlassoffC
TannerM
1992 The relevance of rapid assessment to health research and interventions. Health Pol Plan 7 1 9
47. TugwellP
de SavignyD
HawkerG
RobinsonV
2006 Applying clinical epidemiological methods to health equity: The equity effectiveness loop. Br Med J 332 358 361
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2011 Číslo 1- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- A Simple Novel Method for Determining Mortality Rates in HIV Treatment Programs Worldwide
- Setting Implementation Research Priorities to Reduce Preterm Births and Stillbirths at the Community Level
- A Research Agenda for Malaria Eradication: Monitoring, Evaluation, and Surveillance
- A Research Agenda for Malaria Eradication: Cross-Cutting Issues for Eradication
- A Research Agenda to Underpin Malaria Eradication
- Correcting Mortality for Loss to Follow-Up: A Nomogram Applied to Antiretroviral Treatment Programmes in Sub-Saharan Africa
- The Impact of eHealth on the Quality and Safety of Health Care: A Systematic Overview
- Setting Research Priorities to Reduce Almost One Million Deaths from Birth Asphyxia by 2015
- Predicting Live Birth, Preterm Delivery, and Low Birth Weight in Infants Born from In Vitro Fertilisation: A Prospective Study of 144,018 Treatment Cycles
- Some Lessons for the Future from the Global Malaria Eradication Programme (1955–1969)
- A Research Agenda for Malaria Eradication: Basic Science and Enabling Technologies
- A Research Agenda for Malaria Eradication: Vector Control
- The Role of Research in Viral Disease Eradication and Elimination Programs: Lessons for Malaria Eradication
- The Influence of Distance and Level of Care on Delivery Place in Rural Zambia: A Study of Linked National Data in a Geographic Information System
- Using the Delphi Technique to Determine Which Outcomes to Measure in Clinical Trials: Recommendations for the Future Based on a Systematic Review of Existing Studies
- Development of a Standardized Screening Rule for Tuberculosis in People Living with HIV in Resource-Constrained Settings: Individual Participant Data Meta-analysis of Observational Studies
- WHO/PLoS Collection “No Health Without Research”: A Call for Papers
- Estimates of Pandemic Influenza Vaccine Effectiveness in Europe, 2009–2010: Results of Influenza Monitoring Vaccine Effectiveness in Europe (I-MOVE) Multicentre Case-Control Study
- A Research Agenda for Malaria Eradication: Vaccines
- A Research Agenda for Malaria Eradication: Health Systems and Operational Research
- A Research Agenda for Malaria Eradication: Diagnoses and Diagnostics
- A Research Agenda for Malaria Eradication: Drugs
- A Research Agenda for Malaria Eradication: Modeling
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- The Impact of eHealth on the Quality and Safety of Health Care: A Systematic Overview
- A Research Agenda for Malaria Eradication: Cross-Cutting Issues for Eradication
- Estimates of Pandemic Influenza Vaccine Effectiveness in Europe, 2009–2010: Results of Influenza Monitoring Vaccine Effectiveness in Europe (I-MOVE) Multicentre Case-Control Study
- Using the Delphi Technique to Determine Which Outcomes to Measure in Clinical Trials: Recommendations for the Future Based on a Systematic Review of Existing Studies
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



