-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Non-Specialist Psychosocial Interventions for Children and Adolescents with Intellectual Disability or Lower-Functioning Autism Spectrum Disorders: A Systematic Review
Background:
The development of effective treatments for use by non-specialists is listed among the top research priorities for improving the lives of people with mental illness worldwide. The purpose of this review is to appraise which interventions for children with intellectual disabilities or lower-functioning autism spectrum disorders delivered by non-specialist care providers in community settings produce benefits when compared to either a no-treatment control group or treatment-as-usual comparator.Methods and Findings:
We systematically searched electronic databases through 24 June 2013 to locate prospective controlled studies of psychosocial interventions delivered by non-specialist providers to children with intellectual disabilities or lower-functioning autism spectrum disorders. We screened 234 full papers, of which 34 articles describing 29 studies involving 1,305 participants were included. A majority of the studies included children exclusively with a diagnosis of lower-functioning autism spectrum disorders (15 of 29, 52%). Fifteen of twenty-nine studies (52%) were randomized controlled trials and just under half of all effect sizes (29 of 59, 49%) were greater than 0.50, of which 18 (62%) were statistically significant. For behavior analytic interventions, the best outcomes were shown for development and daily skills; cognitive rehabilitation, training, and support interventions were found to be most effective for improving developmental outcomes, and parent training interventions to be most effective for improving developmental, behavioral, and family outcomes. We also conducted additional subgroup analyses using harvest plots. Limitations include the studies' potential for performance bias and that few were conducted in lower - and middle-income countries.Conclusions:
The findings of this review support the delivery of psychosocial interventions by non-specialist providers to children who have intellectual disabilities or lower-functioning autism spectrum disorders. Given the scarcity of specialists in many low-resource settings, including many lower - and middle-income countries, these findings may provide guidance for scale-up efforts for improving outcomes for children with developmental disorders or lower-functioning autism spectrum disorders.Protocol Registration:
PROSPERO CRD42012002641
Please see later in the article for the Editors' Summary
Published in the journal: Non-Specialist Psychosocial Interventions for Children and Adolescents with Intellectual Disability or Lower-Functioning Autism Spectrum Disorders: A Systematic Review. PLoS Med 10(12): e32767. doi:10.1371/journal.pmed.1001572
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001572Summary
Background:
The development of effective treatments for use by non-specialists is listed among the top research priorities for improving the lives of people with mental illness worldwide. The purpose of this review is to appraise which interventions for children with intellectual disabilities or lower-functioning autism spectrum disorders delivered by non-specialist care providers in community settings produce benefits when compared to either a no-treatment control group or treatment-as-usual comparator.Methods and Findings:
We systematically searched electronic databases through 24 June 2013 to locate prospective controlled studies of psychosocial interventions delivered by non-specialist providers to children with intellectual disabilities or lower-functioning autism spectrum disorders. We screened 234 full papers, of which 34 articles describing 29 studies involving 1,305 participants were included. A majority of the studies included children exclusively with a diagnosis of lower-functioning autism spectrum disorders (15 of 29, 52%). Fifteen of twenty-nine studies (52%) were randomized controlled trials and just under half of all effect sizes (29 of 59, 49%) were greater than 0.50, of which 18 (62%) were statistically significant. For behavior analytic interventions, the best outcomes were shown for development and daily skills; cognitive rehabilitation, training, and support interventions were found to be most effective for improving developmental outcomes, and parent training interventions to be most effective for improving developmental, behavioral, and family outcomes. We also conducted additional subgroup analyses using harvest plots. Limitations include the studies' potential for performance bias and that few were conducted in lower - and middle-income countries.Conclusions:
The findings of this review support the delivery of psychosocial interventions by non-specialist providers to children who have intellectual disabilities or lower-functioning autism spectrum disorders. Given the scarcity of specialists in many low-resource settings, including many lower - and middle-income countries, these findings may provide guidance for scale-up efforts for improving outcomes for children with developmental disorders or lower-functioning autism spectrum disorders.Protocol Registration:
PROSPERO CRD42012002641
Please see later in the article for the Editors' SummaryIntroduction
Developmental disorder is an umbrella term covering disorders such as intellectual disability/mental retardation as well as pervasive developmental disorders including autism spectrum disorders. Developmental disorders usually have a childhood onset, impairment or delay in functions related to central nervous system maturation, and a steady course that persists into adulthood. Intellectual disability, or mental retardation, is defined as “a condition of arrested or incomplete development of the mind, which is especially characterized by impairment of skills manifested during the developmental period, which contribute to the overall level of intelligence, i.e., cognitive, language, motor, and social abilities” [1]. Autism spectrum disorders (also called pervasive developmental disorders), such as autism, Asperger syndrome, childhood disintegrative disorder, and atypical autism, comprise a range of conditions characterized by a varied mixture of impaired capacity for reciprocal socio-communicative interaction and a restricted, stereotyped, repetitive repertoire of interests and activities. The level of intellectual functioning for individuals with autism spectrum disorders is extremely variable, extending from profound impairment to superior nonverbal cognitive skills. It is estimated that up to 50% of individuals with an autism spectrum disorder also have an intellectual disability [2].
Neurodevelopmental disorders, including intellectual disability and autism spectrum disorders, affect children worldwide, might be a more prevalent condition in lower - and middle-income countries (LMICs) compared to higher-income countries (HICs) [3], and account for more than 0.4% of all disability-adjusted life years [4]. Although most of the children and families affected by neurodevelopmental disorders live in developing countries, nearly all research, preventative efforts, and services are directed towards individuals living in the world's wealthiest countries [5]. International evidence has shown that 75% to 85% of individuals with mental disorders in some LMICs do not receive any treatment services [6], and the lack of services prevents children from realizing a high quality of life and increases the burden on families [4]. The World Health Organization's Atlas: Global Resources for Persons with Intellectual Disabilities [7] provides more evidence of these disparities by showing that available resources are proportional to a country's income. In LMICs significantly fewer resources are available to dedicate to providing mental health services, and specialized human resources to deliver interventions are often either not available or available at a much lower rate than in HICs [5],[7]–[11]. Additional barriers to increased service provision for childhood mental disorders in LMICs include the lack of evidence on effective treatments delivered in these settings and a limited capacity for identifying children with developmental disorders [9],[12].
The development of effective treatments for use by non-specialists (e.g., mental health care providers who are not psychiatrists, psychologists, or psychiatric nurse practitioners) is listed among the top research priorities for improving the lives of people with mental illness worldwide [13]. Task shifting approaches that build the capacities of a range of care providers in community settings have been successfully adopted and can be instrumental for increasing access to care for individuals with a range of mental disorders in low-resource settings [14],[15]. Evidence on the effectiveness of provision of psychosocial interventions for intellectual disabilities and autism spectrum disorders by non-specialist providers in HICs is emerging [16].
Previous systematic reviews on psychosocial interventions for intellectual disabilities and autism and other pervasive developmental disorders conducted in LMICs identified few relevant papers, and many of the studies had significant methodological shortcomings [17]–[19]. Thus, formulating practice guidance based solely on the findings from studies conducted in LMICs, which would provide the results with the best ecological validity, is difficult to accomplish at this time. Hence, there is a need to conduct a review that includes psychosocial interventions conducted in HICs that might be feasibly adapted for implementation in LMICs. The purpose of this review is to provide an appraisal of which interventions for children and adolescents with intellectual disabilities or lower-functioning autism spectrum disorders delivered by non-specialist care providers in community settings produce benefits in development, daily skills, school performance, behavior, or family outcomes when compared to either a no-treatment control group or treatment-as-usual comparator.
Methods
Selection Criteria
We included studies in our review meeting the following inclusion criteria. First, the study contained participants with neurodevelopmental disorders who, on average, had a full scale IQ<70 and were, on average, under the age of 18 y. Second, the study used a prospective controlled study design, specifically, a study design comparing a treatment to a control condition, regardless of randomization. We included non-randomized controlled studies because we thought we might have difficulty locating a large pool of randomized controlled trials from which to build recommendations, and because we wanted to locate all studies with high ecological validity (e.g., studies conducted in similar contexts and under similar conditions regardless of randomization). Third, the study involved a psychosocial intervention. For this review, psychosocial intervention was defined as a therapy, education, training, or support aimed at improving behavior, general overall development, or specific life skills without the use of psychopharmacologic agents. Fourth, an individual who was not a specialist provided the psychosocial intervention or parent education to the child or parents, respectively. Stated differently, we included only studies in which a non-specialist (e.g., teacher, aide, parent, general practitioner, nurse practitioner, or local clinician) provided the direct intervention sessions to the child or conducted the parent education sessions. For this review, we considered psychiatrists, psychiatric nurse practitioners, psychologists, speech and language pathologists, occupational therapists, and physical therapists, among others, to be specialist providers. Fifth, the study was published in English, French, or Spanish. Included and excluded studies were collected following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [20].
Search Methods
We conducted an electronic database search of African Index Medicus, AFRO Library, the Cochrane Central Register of Controlled Trials, Cumulative Index to Nursing and Allied Health, Embase, Western Pacific Region Index Medicus, Literatura Latino-Americana e do Caribe em Ciências da Saúde, Medline, and PsycINFO through 24 June 2013 using the search strategies shown in Texts S1, S2, S3, S4, S5. Because some of our inclusion criteria, mainly the inclusion of non-randomized studies, have the potential to increase bias, we decided not to search gray literature, which has also been considered to potentially introduce additional bias by not providing a representative sample of studies, by containing studies of lower quality, and by having more favorable results being provided more readily [21]. All titles and abstracts were initially screened by one author in order to exclude clearly irrelevant articles, and two authors, working independently and in duplicate, screened full papers of potentially relevant articles and determined which studies met all inclusion criteria. After the database search, we examined the reference lists of ten recent reviews of psychosocial interventions for individuals with developmental disabilities [17]–[19],[22]–[28] for possible studies that were not located in the database search.
Variable Definitions and Coding
We coded 16 variables related to research methods, participant characteristics, treatment characteristics, and study results. All variables and effect size estimates were coded independently by two abstractors, and all discrepancies were resolved through mediation.
We coded four variables related to the participants of each study. First, we coded child diagnosis by indicating whether (a) all participants had a diagnosis of a lower-functioning autism spectrum disorder, (b) all participants had intellectual disability without an autism spectrum disorder, or (c) there was a mixture of participants with diagnoses of intellectual disability with an autism spectrum disorder and participants with intellectual disability without an autism spectrum disorder. Second, we coded the sample size by recording the total number of participants in the study and the number of participants in the treatment and comparison groups. Third, we calculated the mean age of the participants and provided a standard deviation and/or range when possible. Fourth, we estimated the participant's skill level by recording the mean (and standard deviation) of an IQ or developmental quotient (DQ) when it was provided in the study report or by calculating a DQ by dividing the mean mental age by mean chronological age and multiplying by 100. When only a range was reported, e.g., IQ<70, the range was recorded and reported instead of a mean and standard deviation.
We coded five variables related to the research study design and methods. First, we coded whether the study used a randomized controlled trial or quasi-experimental research design. Second, we identified the country in which the study occurred (i.e., study location). Third, within the study location, we coded whether the study occurred in a country classified by the World Bank in July 2012 as Lower Income (gross national income <US$1,025), Lower-Middle Income (US$1,026–US$4,035), Upper-Middle Income (US$4,036–US$12,475), or High Income (US$12,476 or more). Fourth, for outcomes, we classified the measures reported in each study into one of five categories: (a) development (e.g., standardized tests of IQ, developmental progress, or language; measures of cognitive processes), (b) daily skills (e.g., adaptive behavior), (c) school performance (e.g., reading ability, literacy skills), (d) behavior (e.g., problem behavior, symptoms of behavioral disorders such as hyperactivity and inattention), or (e) family (e.g., parental stress, parental sense of competence, parenting skills). Fifth, we evaluated risk of bias using an adaptation of the Cochrane Collaboration's Risk of Bias Tool [29] to assess eight items: sequence generation, allocation concealment, performance bias, detection bias, attrition, selective outcome reporting, protection against contamination, and baseline imbalance. The adaptations to the Cochrane Collaboration's Risk of Bias Tool were made to accommodate our decision to include non-randomized trials and are consistent with emerging recommendations of the Cochrane Collaboration's Non-Randomised Studies Methods Group [30],[31].
We coded two variables related to study results and findings. First, for the effect size, we calculated the standardized mean difference between the posttreatment means of the treatment and comparison groups using Cohen's d for each outcome category, using effect size calculators based on the formulae provided in Lipsey and Wilson [32] housed on the Campbell Collaboration website (http://www.campbellcollaboration.org/resources/effect_size_input.php). Cohen's d [33] is an effect size reported as standard deviations (i.e., d = 1.0 is a one-standard-deviation difference between treatment and control) that is calculated by dividing the difference in mean outcome between groups by the standard deviation of outcomes among participants. Classic guidelines [33] for interpreting the magnitude of effect for Cohen's d suggest that an effect size <0.20 indicates no effect, 0.20–0.50 indicates a small effect, 0.50–0.80 indicates a medium effect, and >0.80 indicates a large effect. We have chosen to combine the medium and large effects in our interpretation of the magnitude of effect to reflect that many clinically significant effects can be found in effect sizes less than 0.80 but greater than 0.50. The statistical significance of effect sizes was determined by examination of the 95% CI when available. For outcomes for which effect sizes were averaged, statistical significance is indicated only if the 95% CI for all measures indicated statistical significance. When more than one outcome was included in a single study for one of our outcome categories (e.g., two separate family measures such as parent stress and quality of life), we calculated an unweighted mean of all variables within the outcome category and provided the range of effect size estimates instead of the standard deviation and 95% confidence intervals. We chose to present our effect size estimates for studies with multiple measures within one outcome category using this method because measures of the same construct within one sample are likely to be highly correlated, which can have significant impacts on mean calculations that are used to produce more standard estimates that include standard deviations and confidence intervals [34]. When multiple treatment groups receiving similar interventions were reported in one study, we averaged the posttreatment means and standard deviations for all treatment groups and compared this to the posttreatment scores from the control group. We considered synthesizing results statistically using methods such as meta-analysis, including multiple regression techniques, but decided against such analyses given the small number of studies that were ultimately located, and our decision to include randomized and non-randomized trials. Second, in addition to the effect size, we coded and reported the results of statistical significance testing, as reported in the study article, including, when available, a description of differential effects.
We coded five intervention characteristic variables. First, we determined the type of psychosocial intervention, which we categorized into three categories: (a) behavior analytic interventions, (b) cognitive rehabilitation, training, and support, or (c) parent training interventions. Second, the first author created a summary of intervention methods, which is reported as the intervention description. Included in this description, at a minimum, is an indication of whether the treatment was delivered in an individual or group format (if group, the number of participants per group is provided), the location where the treatment or training sessions were conducted, and whether the intervention contained a parent component (behavior analytic and cognitive rehabilitation only). Third, we coded a variable describing who provided the treatment to the child or the training to the parents (intervention agent, training, and supervision). Within this variable, when provided in the study report, we quantified the amount of training and supervision received by the treatment provider or parent trainer prior to and/or during the course of each study. Fourth, we quantified the intervention density by recording, if provided, the duration of each session, the number of sessions per week, and the number of weeks of treatment. Fifth, we calculated the total hours of therapy each participant received, on average, using the intervention density data we collected.
Harvest Plots
To examine differential treatment effects across different variables of interest (e.g., study location, participant characteristics, treatment location, treatment/training provider, treatment density), we chose to construct graphical representations of the effect size using harvest plots [35],[36]. A harvest plot is a graphical display of treatment effects plotted across multiple variables, allowing for visual analysis of differential treatment effects. We chose to use harvest plots to analyze and synthesize the evidence because we determined that meta-analytic methods were not appropriate because of the large variability in intervention techniques and outcome variables.
In each harvest plot we have grouped the marks (the rectangles representing study effects) on the horizontal axis according to effect size estimates corresponding to Cohen's guidelines [33] (no effect, effect size <0.20; small effect, effect size = 0.20–0.49; and medium to large effect, effect size >0.50). The marks are grouped on the vertical axis by the type of psychosocial intervention (behavior analytic interventions; cognitive rehabilitation, training, and support; and parent training) that was used in each study. The heights of the marks represent the research methodology used in the study, with the taller marks indicating studies using randomized controlled trials and the shorter marks indicating studies using quasi-experimental designs. Statistical significance (determined by examination of the 95% CI when available) is indicated in the harvest plots for each study outcome by an asterisk above the mark. The marks are also color-coded by outcome category (black = development, gray = daily skills, white = school performance, vertical stripes = behavior, and horizontal stripes = family). We have indicated participant diagnostic categories for each study using black bars that are placed above the marks. Participant diagnostic characteristics (i.e., all participants had intellectual disability, all participants had lower-functioning autism spectrum disorder, or the study contained a mixture of participants with both intellectual disability and lower-functioning autism spectrum disorder) are indicated above each mark. Finally, all harvests plots contain multiple panels, which are labeled above each plot (e.g., comparison of results between outcomes, comparison between levels of cognitive impairment).
Results
Search Results
We located 20,806 records; 17,501 records remained after deduplication. Two hundred thirty-four articles remained after the first author screened the titles and abstracts. The first and second authors examined the 234 full papers independently, and in duplicate, for inclusion in this review. Our database search located 34 articles describing 29 studies that met all inclusion criteria. The primary reasons for exclusion are provided in Text S6 and are shown in the PRISMA flow diagram of Figure 1. No additional studies were located in the hand search of previous reviews. We have used study as the unit of analysis for all results to ensure that studies reported in multiple articles are not weighted more heavily than those presented in one article.
Fig. 1. Study inclusion decision tree (using PRISMA flow diagram <em class="ref">[20]</em>). ![Study inclusion decision tree (using PRISMA flow diagram <em class="ref">[20]</em>).](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image/835c144777118ef2ef6b61541f09ddb7.png)
Participant Characteristics
Table 1 presents the participant characteristics of the 1,305 participants across the 29 studies included in this review. The mean age of the participants ranged from 0.4 y (about 5 mo) to 15.8 y. A majority of the studies (19 of 29, 66%) had samples with a mean age less than 6 y; nine of 29 (31%) studies had a mean age of participants older than 6 y (a mean age was not able to be obtained for one study, 3%). Across studies, a majority of the studies included children exclusively with a diagnosis of a lower-functioning autism spectrum disorder (15 of 29, 52%); six of 29 (21%) studies included a mixture of participants with intellectual disability or lower-functioning autism spectrum disorder, and eight of 29 studies (28%) included participants who had intellectual disability without an autism spectrum disorder. Sixteen of 29 studies (55%) had IQ or DQ estimates between 50 and 69, and five of 29 (17%) studies had participants with IQ or DQ estimates below 50 (a mean IQ or DQ could not be obtained for eight of 29 studies, 28%).
Tab. 1. Included studies and participant characteristics. 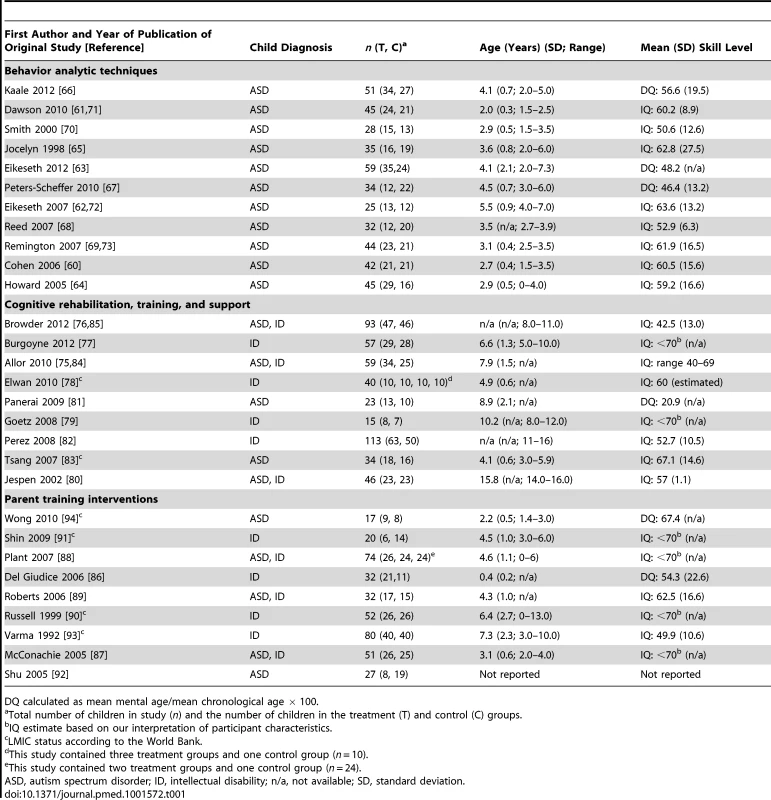
DQ calculated as mean mental age/mean chronological age × 100. Intervention Characteristics
Tables 2–4 provide information on the intervention characteristics across types of psychosocial intervention for studies using behavior analytic techniques; cognitive rehabilitation, training, and support; and parent training interventions, respectively. The treatment agents (e.g., therapists) typically delivered interventions with multiple hours of treatment per week (range 1 to 40 h per week). Treatment duration for the behavior analytic studies and cognitive rehabilitation, training, and support studies was often long, lasting, in many cases, over 100 wk (range 3 to 156 wk); the duration of parent training interventions was typically much shorter, with most lasting between 8 and 12 wk. As seen in the intervention description, a variety of methods and curricula were used across studies. Given that the behavior analytic and cognitive rehabilitation, training, and support studies had higher weekly treatment densities and longer treatment durations, it is not surprising that the number of total contact hours was higher in these studies (range 18 to 6,240 h) than in studies of parent training interventions (range 5 to 52 h). Table 5 provides an overview of the intervention agents, with training and supervision requirements, across all studies. There were multiple types of non-specialist providers including teachers (n = 12), aides (n = 10), and community therapists/clinicians (n = 6). A majority of the studies reported that training and/or ongoing supervision of the non-specialist providers occurred, albeit often with little specificity. When reported, the frequency and duration of training and supervision varied highly across studies from “ongoing on-the-job training” to over 40 h of initial training before beginning to deliver treatment.
Tab. 2. Intervention description, intervention density, and total hours of intervention for behavior analytic intervention studies. 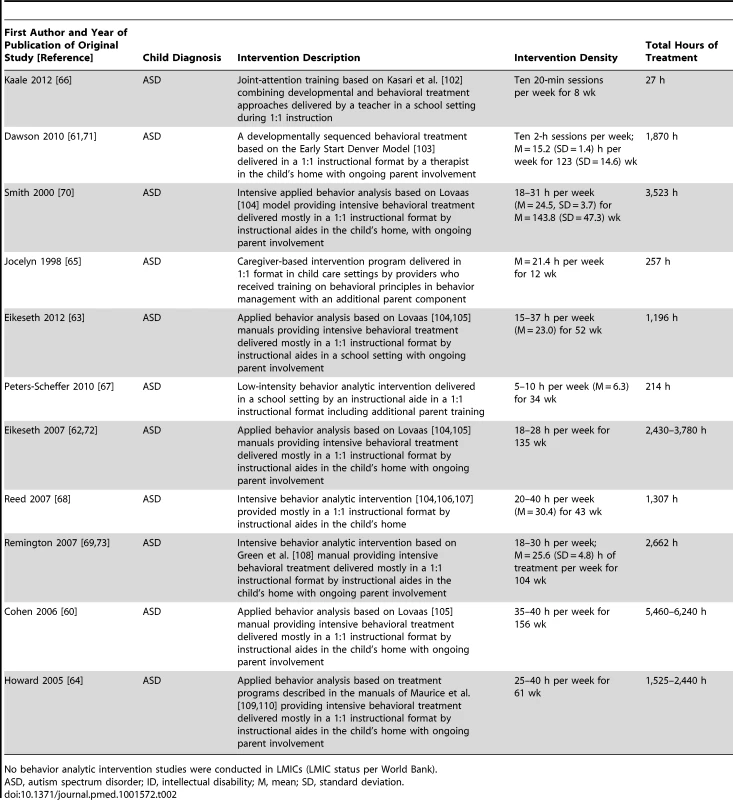
No behavior analytic intervention studies were conducted in LMICs (LMIC status per World Bank). Tab. 3. Intervention description, intervention density, and total hours of intervention for cognitive rehabilitation, training, and support intervention studies. 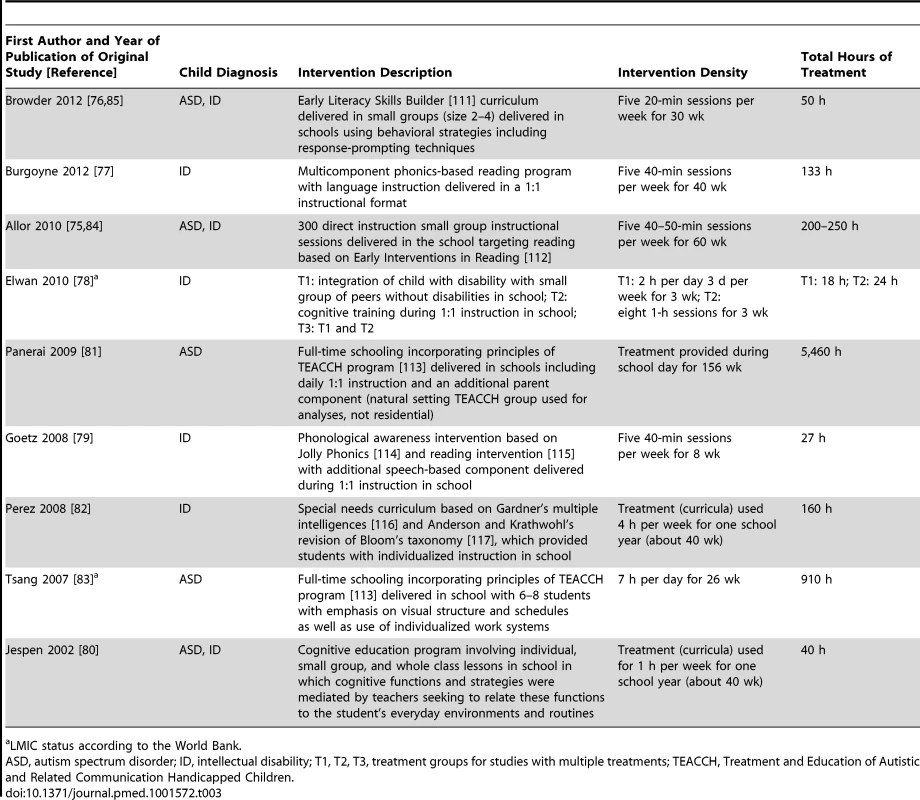
a LMIC status according to the World Bank. Tab. 4. Intervention description, intervention density, and total hours of intervention for parent training intervention studies. 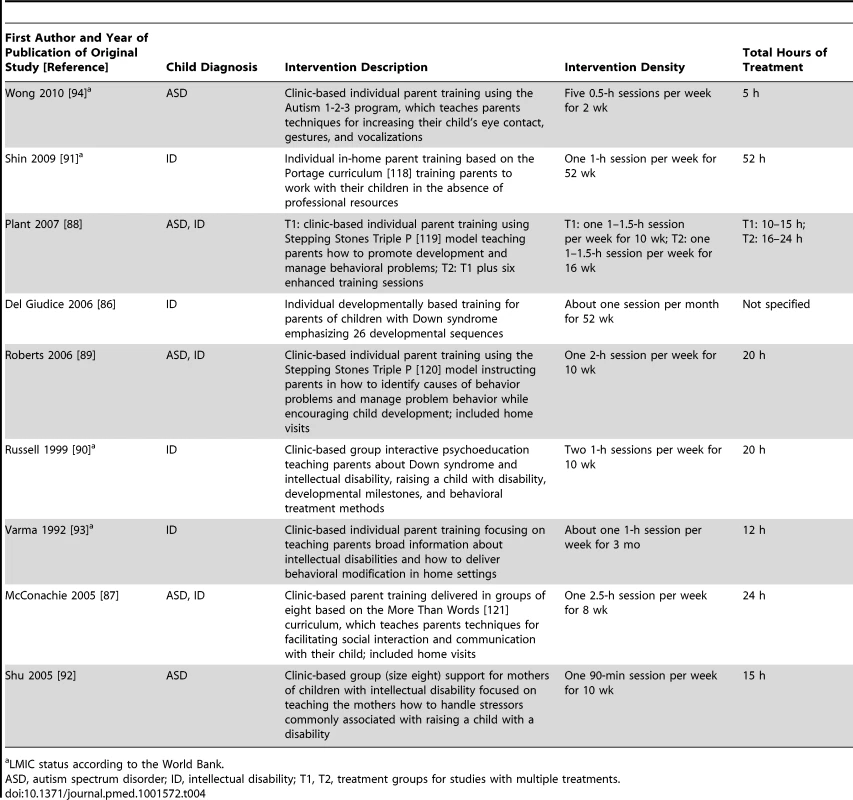
a LMIC status according to the World Bank. Tab. 5. Intervention agent and training and supervision for included studies. 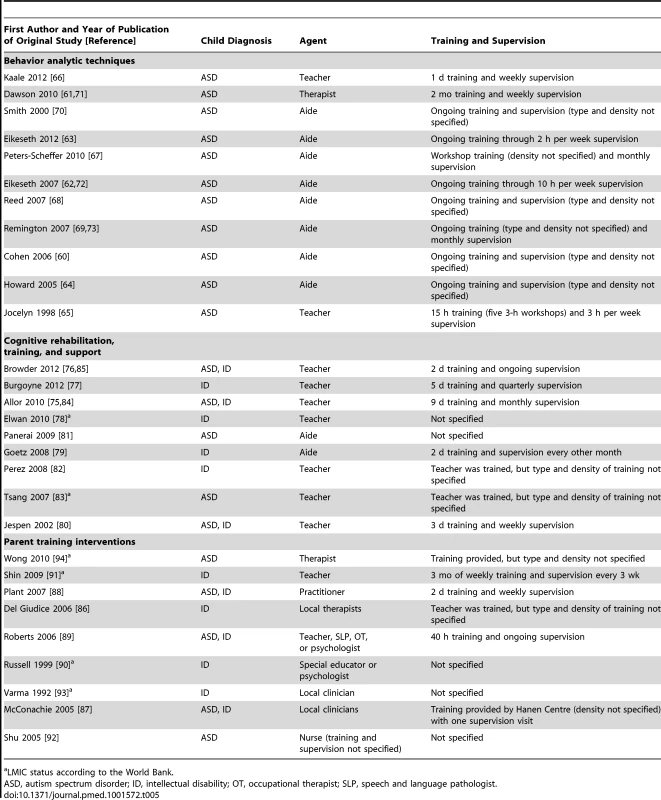
a LMIC status according to the World Bank. Research Characteristics
Tables 6–8 show the research characteristics for studies using behavior analytic techniques; cognitive rehabilitation, training, and support; and parent training interventions, respectively. Just over half of the studies (15 of 29, 52%) used randomized controlled trial designs; prospective controlled study designs were used in 14 studies. Western Europe (12 of 29, 41%) and North America (United States and Canada; eight of 29, 28%) were the most common locations of the research studies included in this review. Of the remaining nine studies, six (21%) were conducted in Asia, two (7%) in Australia, and one (3%) in Africa. Six studies (21%) were conducted in countries classified by the World Bank as LMICs; each of these studies was conducted in a country classified as Lower-Middle Income. A majority of the studies conducted in LMICs examined parent training interventions. There was great variability with respect to the number and types of outcomes measured across studies. Within our outcome categories, some studies measured only one outcome category, while other studies measured up to four outcome categories (no study measured all five outcome categories). Developmental and daily skill outcomes were measured more frequently in psychosocial interventions utilizing behavior analytic techniques and cognitive rehabilitation, while family outcomes were measured more frequently in parent training programs. There was also great variability with respect to the measurement instruments used within each outcome category. For instance, developmental outcomes were measured using a number of different standardized assessments (e.g., developmental outcomes were measured using developmental assessments [37]–[39], standardized IQ tests [38],[40]–[47], and standardized language tests [48]–[58]), while daily skills were mostly measured using a single measure (i.e., Vineland Adaptive Behavior Scale [59]). Additional details on the measures and assessments used in each study by outcome type can be found in Table S1.
Tab. 6. Research design, results, and effect sizes for behavior analytic intervention studies. 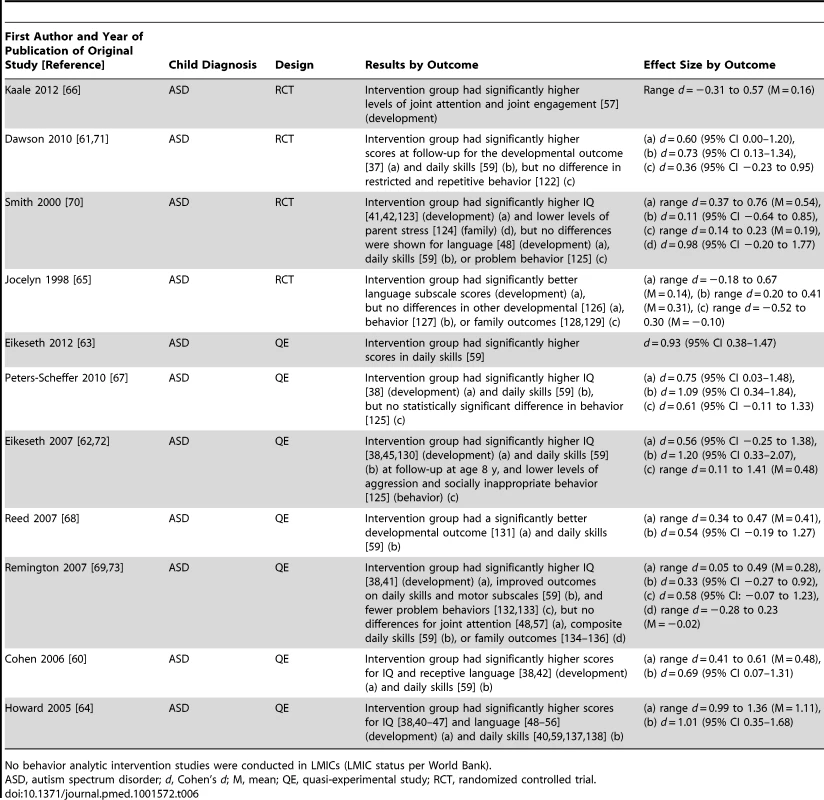
No behavior analytic intervention studies were conducted in LMICs (LMIC status per World Bank). Tab. 7. Research design, results, and effect sizes for cognitive rehabilitation, training, and support intervention studies. 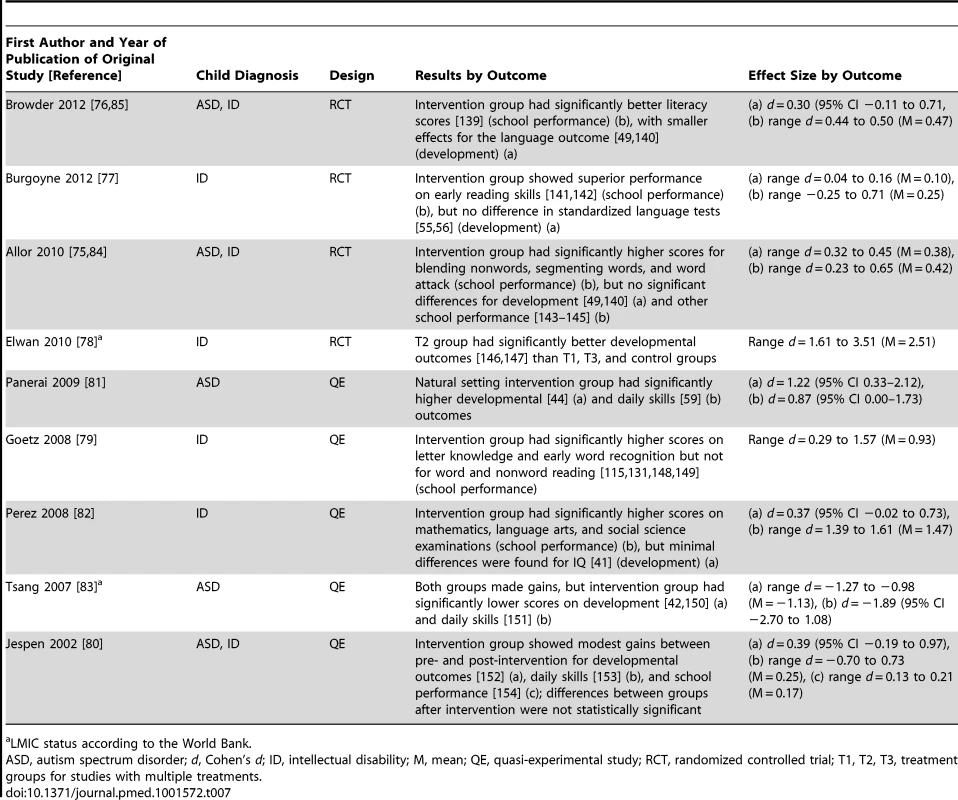
a LMIC status according to the World Bank. Tab. 8. Research design, results, and effect sizes for parent training intervention studies. 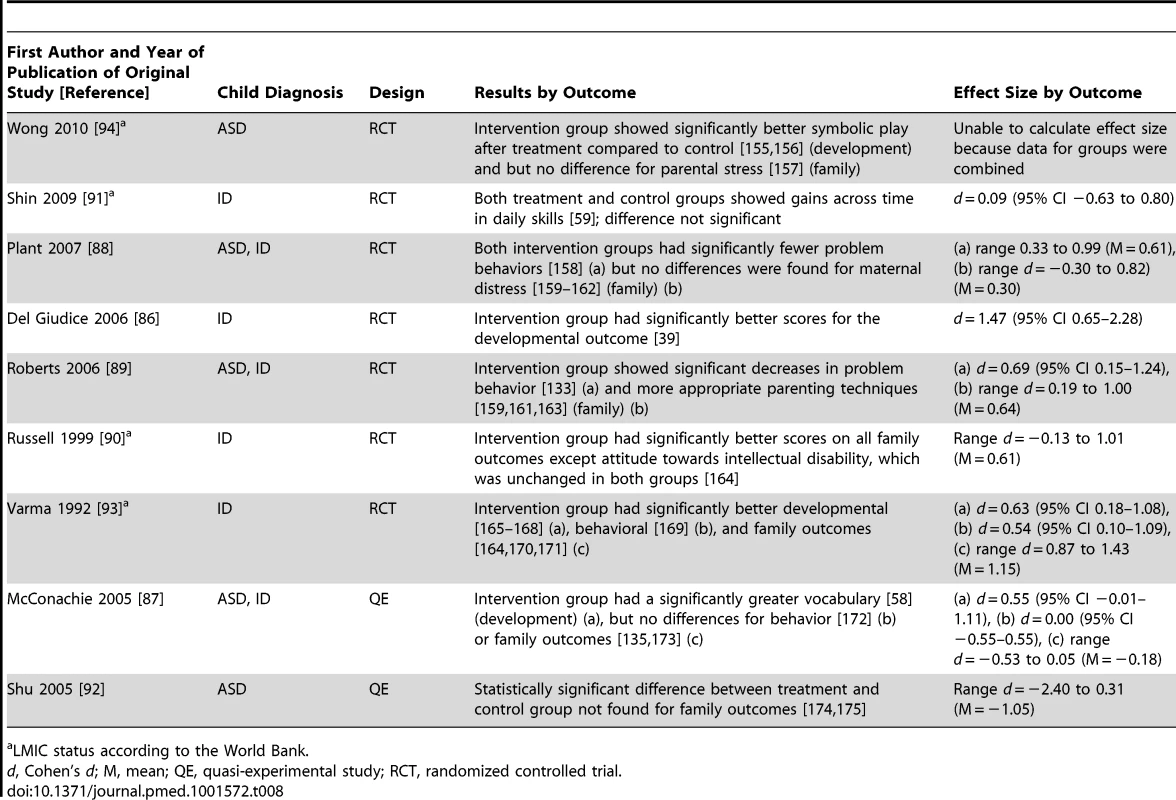
a LMIC status according to the World Bank. Two independent raters assessed eight potential biases in all studies, which are shown as an average across all studies in Figure 2 and for each study by indicator in Figure S1. As seen in Figures 2 and S1, performance bias was a risk in all studies included in the review. This is likely due to the nature of psychosocial interventions, which involve interaction between providers and either the children with disabilities or the parents of the children. Given that many of the studies had low risk of detection bias, it is unclear what effect the high risk of performance bias might have had on the results. There was moderate risk of selection bias, most likely due to our inclusion of non-randomized studies. There was also moderate risk of contamination bias, which was due to the high risk of contamination in many of the behavior analytic studies that used eclectic comparison groups that potentially included elements of the behavioral treatments.
Fig. 2. Risk of bias graph. 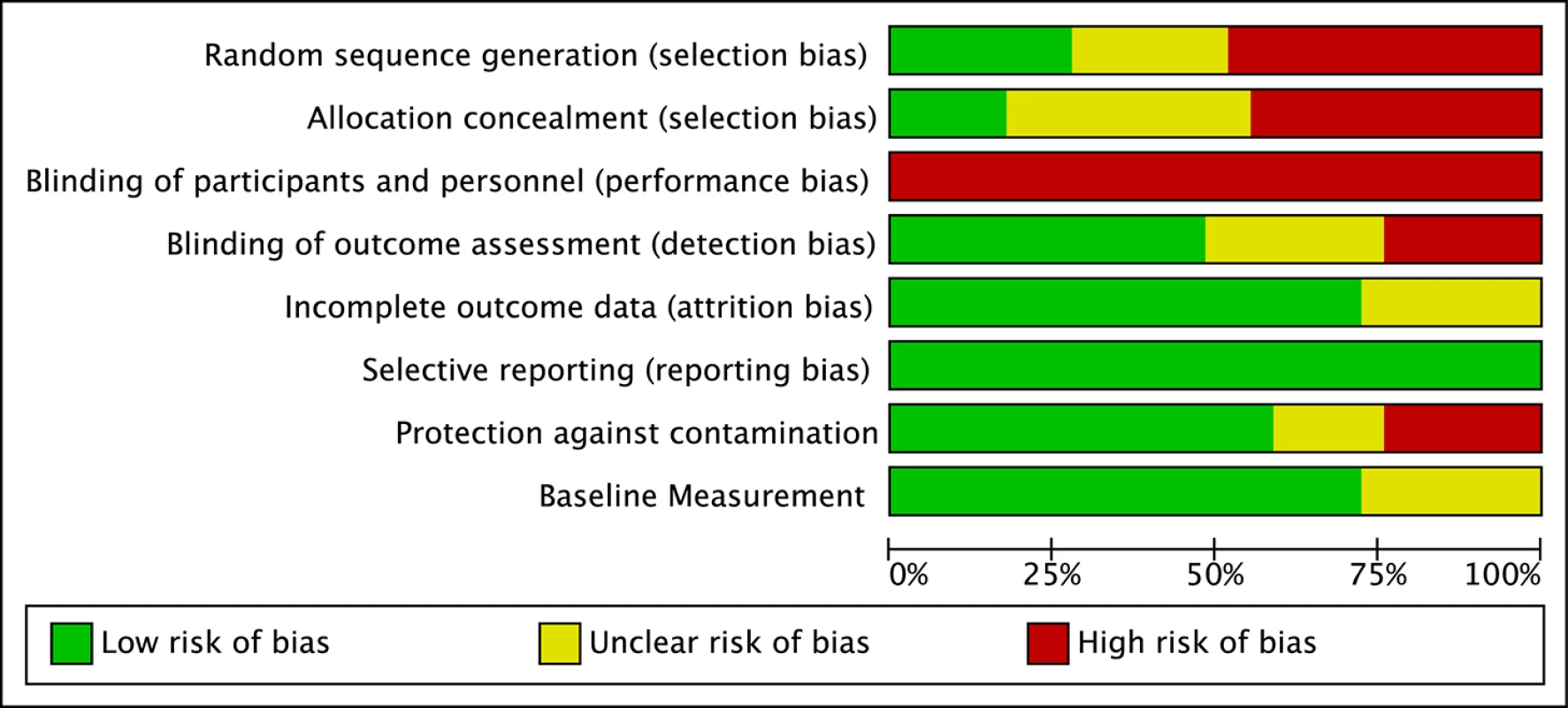
Review authors' judgments about each risk of bias item, presented as percentages across all included studies. Intervention Characteristics and Treatment Effects
Across studies there was a large range of effect size estimates, from a low of −1.89 to a high of 2.51. A large majority of the effect size estimates were positive (45 of 59, 76%), with just under half (29 of 59, 49%) being greater than 0.50, the threshold we took to suggest clinical significance. Eighteen of these 29 effect size estimates greater than 0.50 were statistically significant across intervention types. As shown in Figure 3, for the behavior analytic interventions, the best outcomes shown were for development and daily skills. For the studies of cognitive rehabilitation, training, and support, shown in Figure 4, the best outcomes were for developmental outcomes in children with intellectual disabilities between 6 and 11 y of age. For the parent training interventions, shown in Figure 5, the best outcomes were found for developmental, behavioral, and family outcomes. More detailed analyses, including subgroup analyses by type of intervention, are presented below.
Fig. 3. Harvest plot matrix of effect size estimates by outcome category for behavior analytic studies. 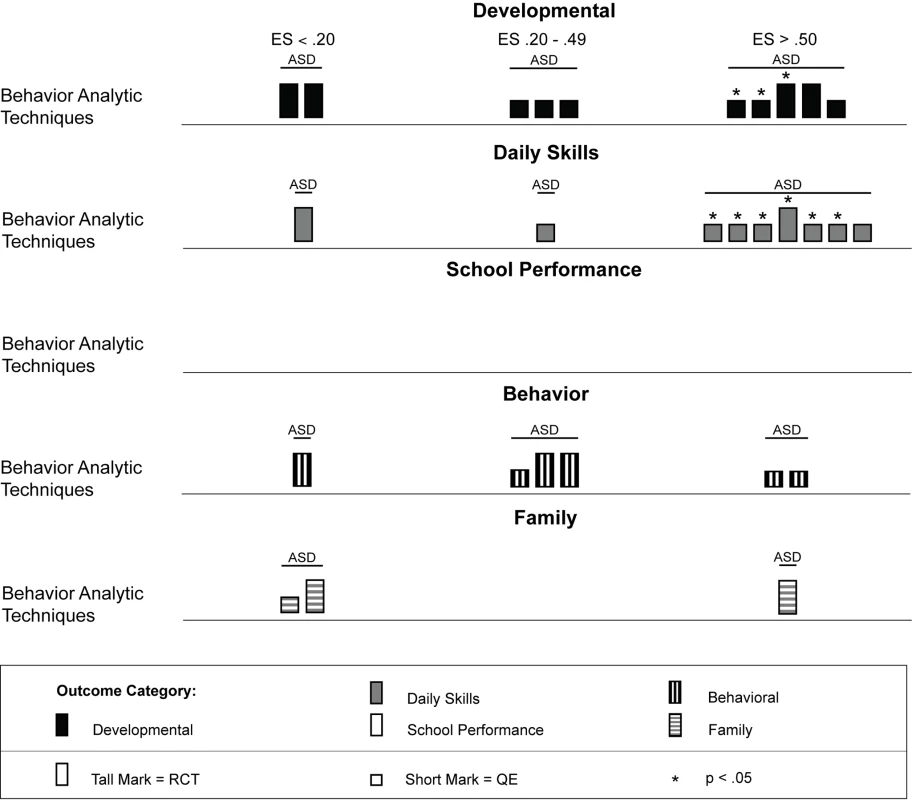
ASD, autism spectrum disorders; ES, effect size; QE, quasi-experimental study; RCT, randomized controlled trial. Fig. 4. Harvest plot matrix of effect size estimates by outcome category for cognitive rehabilitation, training, and support studies. 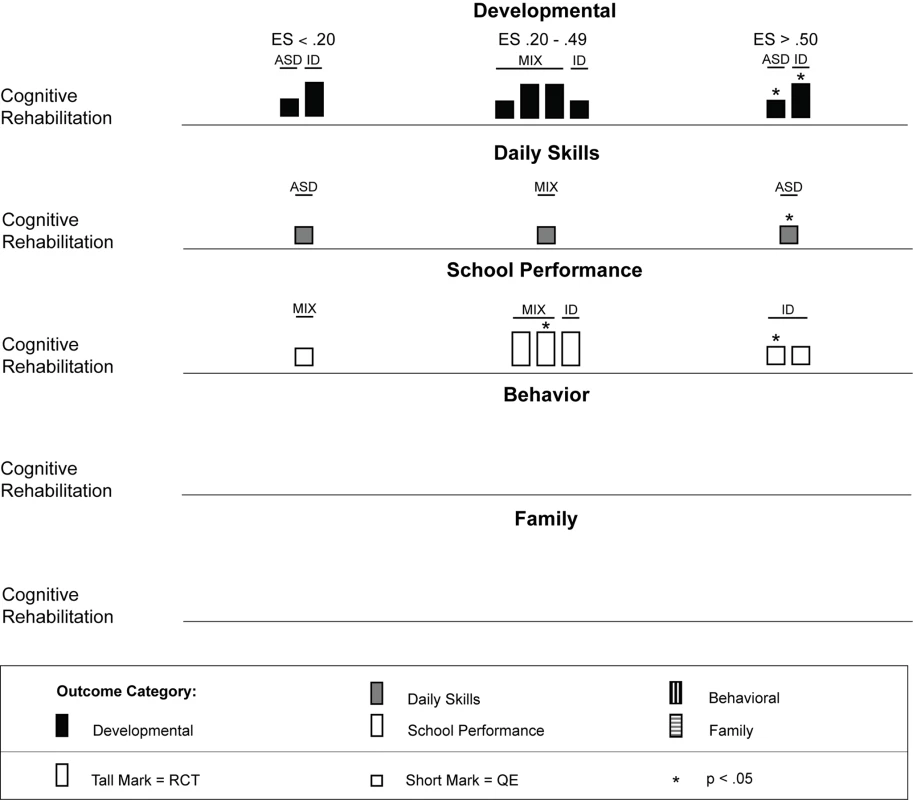
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; MIX, autism spectrum disorders and intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. Fig. 5. Harvest plot matrix of effect size estimates by outcome category for parent training interventions. 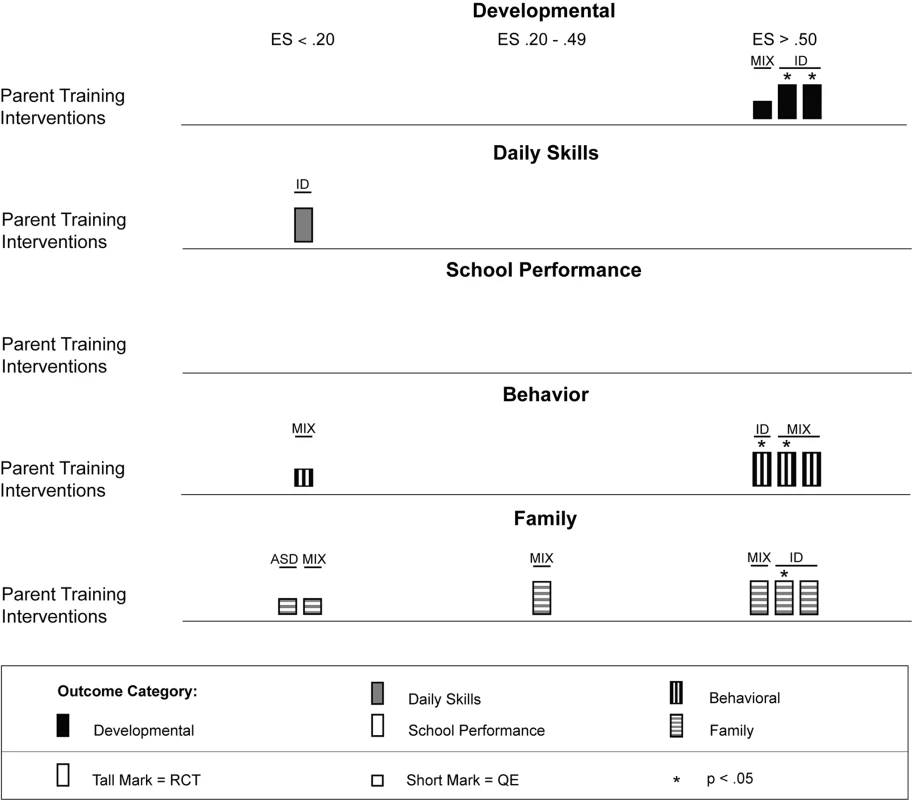
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; MIX, autism spectrum disorders and intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. Psychosocial interventions delivered using behavior analytic techniques
Fourteen articles representing 11 studies [60]–[73] described psychosocial interventions provided by non-specialist providers that used treatments based on the science of applied behavior analysis [74]. Table 2 provides descriptions of the intervention techniques and intervention density for each study, and Table 6 provides descriptions of the research characteristics and outcomes for each behavior analytic study. As shown in Table 6, four of 11 studies [61],[65],[66],[70] were randomized controlled trials, and zero studies were conducted in LMICs. As described in Table 1, these studies included 440 children with lower-functioning autism spectrum disorders who were, on average, under the age of 6 y at the onset of treatment. As shown in Figure 3, effect size estimates for the behavior analytic psychosocial interventions were generally robust, especially for daily skills, for which seven of nine (78%) effect size estimates were greater than 0.50, with six of seven effect size estimates greater than 0.50 having statistical significance. However, only one study with a large statistically significant effect size was a randomized controlled trial [61]. Mixed results were shown for developmental and behavioral outcomes, although two randomized controlled trials [61],[70] showed large effects for developmental outcomes, of which one was statistically significant. Only a few studies measured family outcomes, and no study of behavior analytic interventions examined school performance, even though three studies were conducted in a school setting [63],[66],[67].
The results from the comparison of mean participant age shown in Figure 6 suggests that behavior analytic techniques appear to be most effective for children under 3 y old, where four of seven effect size estimates >0.50 were found in randomized controlled trials [61],[70]. Five of seven (71%) effect size estimates for children under 3 y old were statistically significant, including two of four (50%) estimates from randomized controlled trials. Strong effects were also shown for children who were between 3 and 6 y old, although effect size estimates for three outcomes were <0.20. As shown in Figure 7, no behavior analytic studies included participants at pretreatment who were, on average, older than 6 y old.
Fig. 6. Harvest plot matrix comparison of effects by mean age of participants for children under 6 y old. 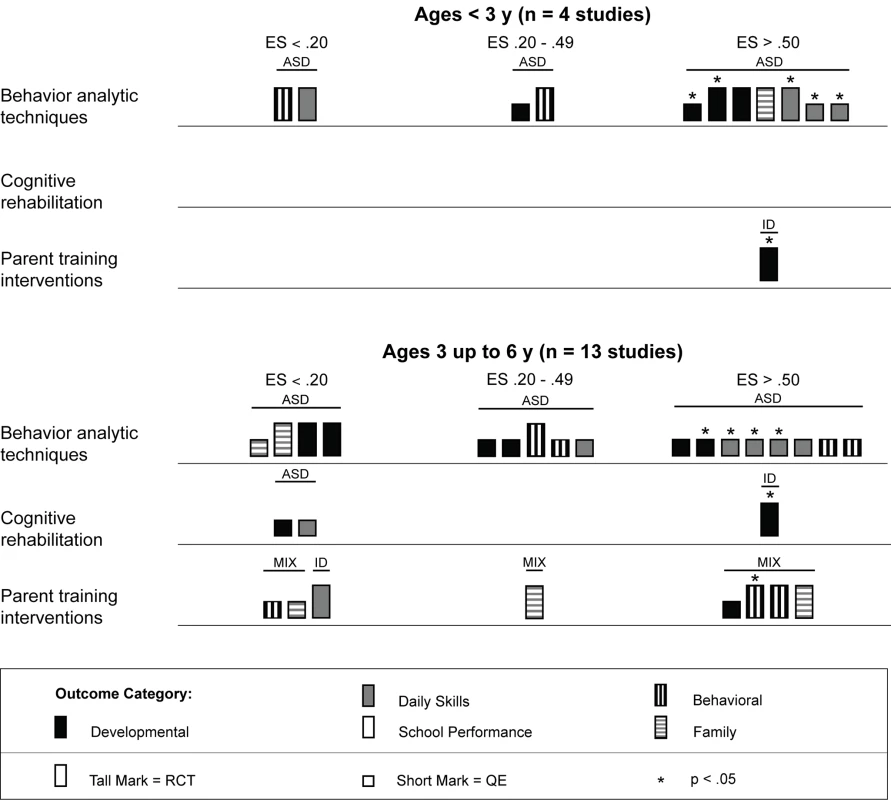
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; MIX, autism spectrum disorders and intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. Fig. 7. Harvest plot matrix comparison of effects by mean age of participants for children 6 y and older. 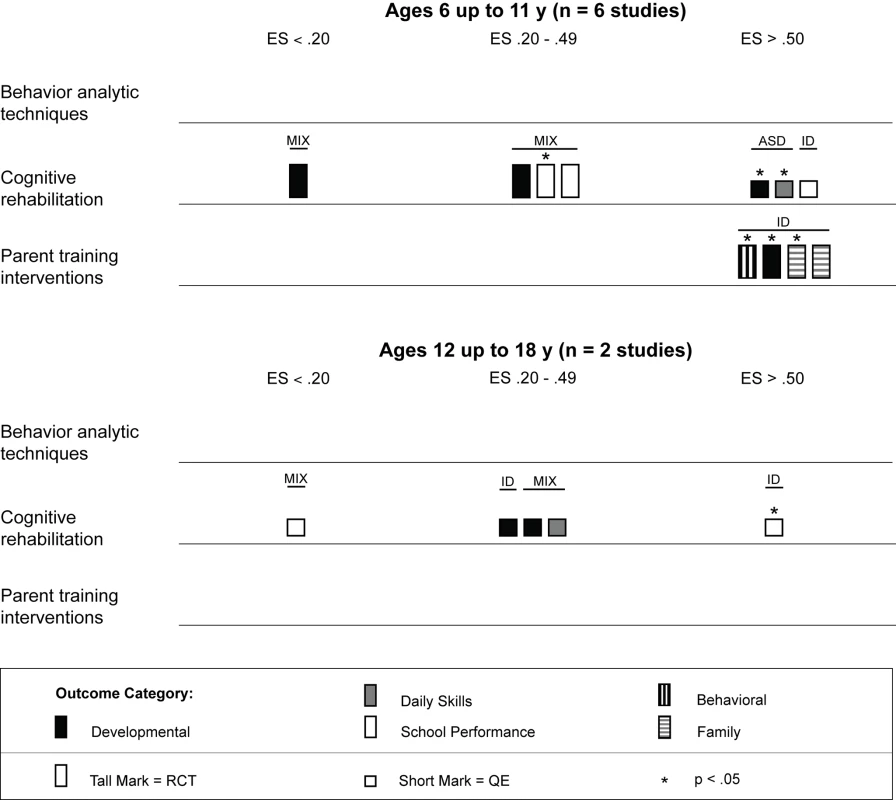
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; MIX, autism spectrum disorders and intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. As shown in Figure 8, behavior analytic interventions seem quite effective for individuals with moderate to severe intellectual impairment; all effect size estimates from Eikeseth et al. [63] and Peters-Scheffer et al. [67] were greater than 0.50, with three of four (75%) estimates having statistical significance. For individuals with milder intellectual impairment, the behavior analytic interventions seemed effective at improving daily skills and developmental outcomes, which had, respectively, four and two effect size estimates greater than 0.50 that were statistically significant.
Fig. 8. Harvest plot matrix comparison of effects by severity of intellectual disability. 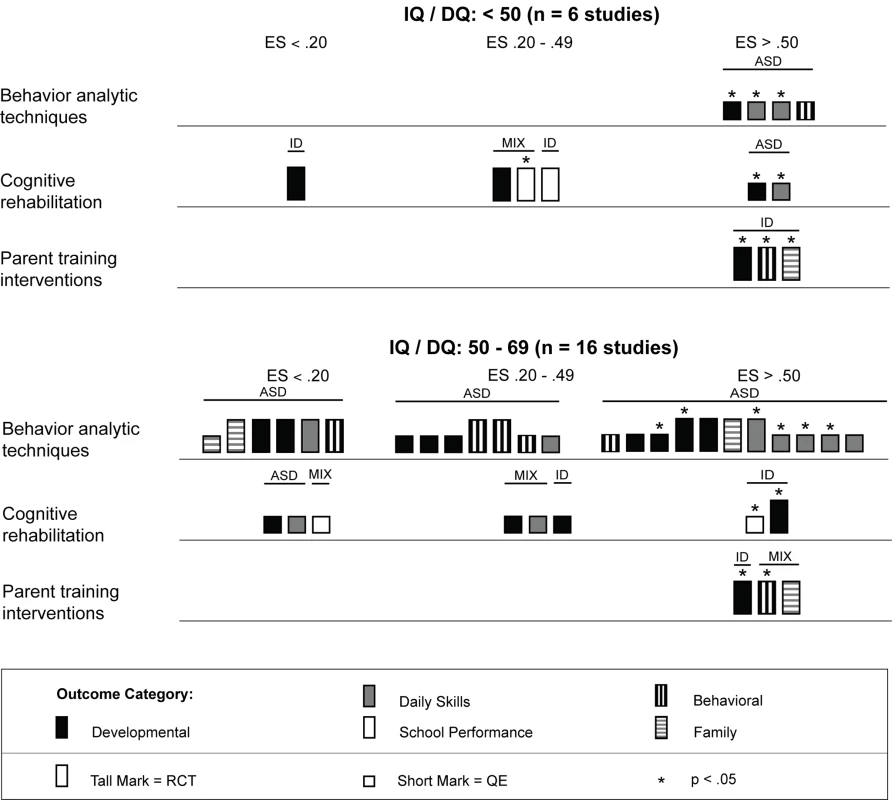
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; MIX, autism spectrum disorders and intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. Figure 9 shows that behavior analytic interventions provided in schools had mixed effects; four of eight (50%) effect size estimates showed strong effects (three of four were statistically significant), and four of eight (50%) effect size estimates showed weak or no effects. For interventions conducted in a home setting, 11 of 20 (55%) effect size estimates were greater than 0.50, with six of the 11 (55%) estimates having statistical significance. In home and school settings, daily skills outcomes showed the most promising effects. Differential effects for other outcomes across settings showed inconclusive results (e.g., behavioral and family outcomes).
Fig. 9. Harvest plot matrix comparison of effects by intervention setting. 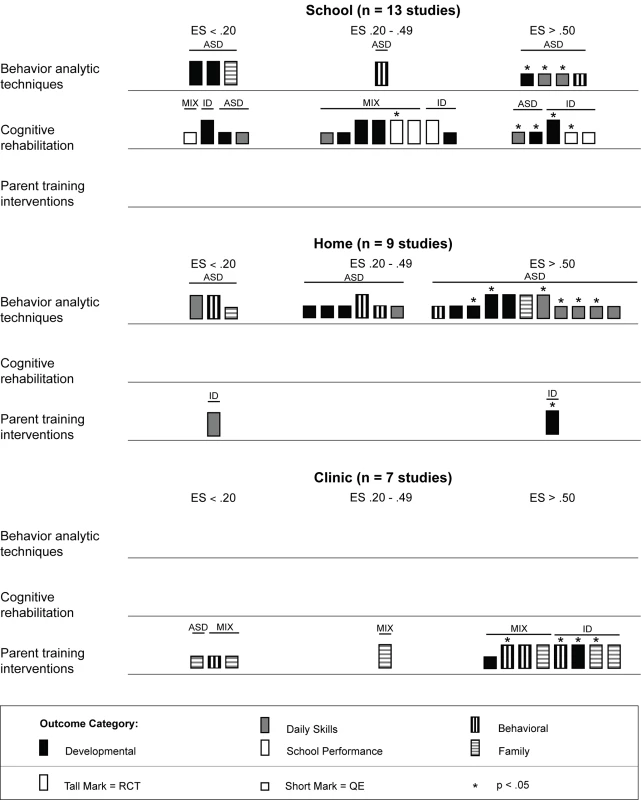
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; MIX, autism spectrum disorders and intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. As shown in Table 2, the majority of behavior analytic studies involved intensive amounts of treatment; nine of 11 (82%) studies provided children with more than 10 h of treatment per week, with durations frequently lasting at least 52 wk. Many of these interventions also had significant amounts of treatment provider supervision, with some studies employing complex multilevel supervision arrangements with intensive training requirements [64],[70]. That the majority of behavior analytic studies involved intense amounts of treatment is also depicted in Figure 10, in which a majority of the effect size estimates in the plot are contained in the second panel (the panel showing studies with >10 h of treatment per week). However, the majority of these estimates came from studies that did not use random assignment to groups, and only seven of 12 (58%) effects were statistically significant. Additionally, there were no comparisons of intervention intensity in any of the studies included in this review; thus, it is not possible to conclude a true relation between treatment density and outcome. Overall, the effects for the high-intensity interventions were somewhat mixed, whereas the outcomes for the interventions with fewer than 10 h of treatment per week showed some promising outcomes. Jocelyn et al. [65] found significant improvement in standardized language scores, but not other developmental outcomes, using an intervention with moderate weekly density (mean = 21 h) with a shorter duration than most behavior analytic treatments (12 wk). Two studies examined interventions with densities lower than 10 h per week, with Kaale et al. [66] finding mixed results (significant increases in some but not all aspects of joint attention), and Peters-Scheffer et al. [67] finding strong effects for IQ, daily skills, and behavior, with effect sizes for all exceeding d = 0.60.
Fig. 10. Harvest plot matrix comparison of effect by treatment density. 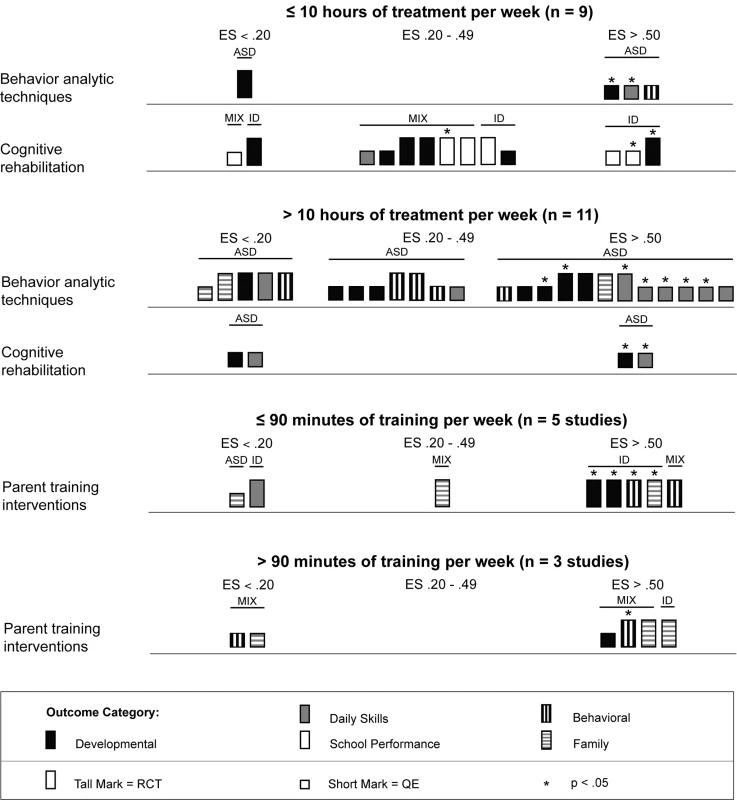
ASD, autism spectrum disorders; ES, effect size; ID, intellectual disability; QE, quasi-experimental study; RCT, randomized controlled trial. Psychosocial interventions delivered using cognitive rehabilitation, training, and support
We located 11 articles representing nine studies [75]–[85] involving 480 children with intellectual disabilities or lower-functioning autism spectrum disorders in which non-specialist providers delivered cognitive rehabilitation, training, and support interventions. Table 3 provides descriptions of the intervention techniques and intervention density for each study, and Table 7 provides descriptions of the research characteristics and outcomes for each cognitive rehabilitation, training, and support study. Four of nine (44%) studies [75]–[78] were randomized controlled trials, and two studies were conducted in LMICs [78],[83]. All studies occurred in school settings, with some focusing on specific curricular areas [75]–[77] and others incorporating curricular approaches to whole day instruction [81],[82]. As shown in Table 5, both teachers and aides, with different training and supervisory requirements across studies, delivered interventions. All outcomes addressed using cognitive rehabilitative strategies showed mixed effects, but, as illustrated in Figure 4, developmental and school performance outcomes showed the strongest effects (although only one of the four effect size estimates >0.50, which was statistically significant, was from a study that used a randomized controlled trial design [78]).
As shown across tables, the cognitive rehabilitation studies included participants older than 4 y with a mixture of diagnostic history with all levels of intellectual disability. Overall, the cognitive rehabilitation studies had the highest mean participant chronological ages; no studies had a mean age less than 3 y, and seven of nine (78%) studies had mean chronological ages older than 6 y. The cognitive rehabilitation category had the only studies with adolescents in this review [80],[82]. As shown in Figures 6 and 7, the results of the studies were mixed across age ranges, with no range showing superior effects over another. Likewise, as shown in Figure 8, the results were also mixed with respect to level of cognitive impairment. Given the small number of studies, compounded by the variability in intervention methods and intervention density, it is difficult to ascertain a true relation between cognitive ability and intervention success.
Intervention density was directly related to the overall approach, with focal content interventions having relatively low densities of about 2 h per week and whole day curricular approaches typically having densities in excess of 30 h per week. As shown in Figure 10, there is not clear evidence that greater intervention density was related to greater intervention effects, with 50% or fewer estimates for both density categories (≤10 h per week and >10 h per week) having effect size estimates greater than 0.50.
Psychosocial interventions delivered using parent training
We located nine studies [86]–[94] involving 368 children with intellectual disabilities or lower-functioning autism spectrum disorders in which the child's parents received a parent training intervention delivered by a non-specialist provider. Table 4 provides descriptions of the intervention techniques and intervention density for each study, and Table 8 provides descriptions of the research characteristics and outcomes for each parent training intervention study. Seven of nine studies were randomized controlled trials, and four studies, all randomized controlled trials, were conducted in LMICs [90],[91],[93],[94]. Most studies we located examined parent training interventions that were focused on teaching parents how to provide therapy services to their child; one study [92] focused mostly on improving parental well-being. As shown in Figure 5, the strongest effects were shown in developmental, behavioral, and family outcomes, with each outcome having three effect size estimates greater than 0.50, with many of these outcomes shown in randomized controlled trials [86],[88]–[90],[93], and with five of nine of the effect size estimates, all from randomized controlled trials, having statistical significance. As shown in Figures 6 and 7, the parent training interventions were most effective for parents of primary-school-aged children, where all four effect size estimates, three of which were statistically significant and all of which were from randomized controlled trials, were >0.50 [90],[93].
As described across tables and shown across figures, studies of parent training interventions typically included samples that were exclusively children with intellectual disability or studies that were a mixture of children with intellectual disability and lower-functioning autism spectrum disorders. The strongest effects were shown for individuals with intellectual disability without autism (five of six effect size estimates >0.50). Given the lack of specificity of child developmental level (five studies did not report a specific level; see Table 1 and Figure 8), we were unable to draw conclusions about whether parent training interventions were more or less effective for children with mild or more severe levels of intellectual impairment. Likewise, since seven of nine (78%) studies were conducted in clinical settings, comparison of clinic-based and home-based parent training programs was not possible (see Table 5 and Figure 9).
Compared to the behavior analytic interventions, the parent training interventions had much lower intervention densities, typically one or two 60 - to 120-min sessions per week for 8 to 16 wk (see Table 4). As shown in Figure 10, five of eight (63%) effect size estimates, four of which were statistically significant, and three of six (50%) effect size estimates, one of which was statistically significant, were greater than 0.50 for the lower-density (≤90 min per week) and higher-density (>90 min per week) categories, respectively. All effect size estimates for the lower-density category came from randomized controlled trials, and three of four large effect size estimates for the higher-density category came from randomized controlled trials. Although it does not appear that increased density was systematically related to greater effects, it should be noted that these programs were often provided in conjunction with, not replacing, the child's typical school or early intervention programming, which complicates our ability to draw definitive conclusions.
Discussion
Summary of Main Findings
This review shows that there is a range of psychosocial interventions for individuals with intellectual disabilities or lower-functioning autism spectrum disorders that can be provided by non-specialist service providers. Overall, the outcomes of the studies included in this review show that non-specialist providers can deliver effective treatments to children with intellectual disabilities or lower-functioning autism spectrum disorders. As stated earlier, there was a large range of effect size estimates, from a low of −1.89 to a high of 2.51; a large majority of the effect size estimates were positive (45 of 59, 76%), with just under half (29 of 59, 49%) being greater than 0.50, likely indicating clinically significant effects. Eighteen of the 29 effect size estimates greater than 0.50 were statistically significant across intervention types. For the behavior analytic interventions, the best outcomes were shown for development and daily skills, especially for children with more severe levels of cognitive impairment at treatment onset. Cognitive rehabilitation, training, and support were found to be most effective for improving developmental outcomes in children with intellectual disabilities between 6 and 11 y of age, with mixed effects shown for daily skills and school performance. Finally, we found parent training interventions to be most effective for improving developmental, behavioral, and family outcomes when training was conducted in clinical settings. The strongest evidence from randomized controlled trials was found for parent training interventions, which had seven randomized controlled trials. For the parent training interventions, eight of nine effect size estimates greater than 0.50 were found for developmental, behavioral, and family outcomes, with five of the eight estimates from randomized controlled trials having statistical significance. Although our methods preclude a formal sensitivity analysis, examination of the tall marks in Figures 3–5 (which are representative of studies conducted using a randomized controlled trial design) shows the greatest amount of evidence for developmental and family outcomes for behavior analytic and parent training interventions, and robust findings for behavioral outcomes for parent training interventions. It is also noteworthy that the greatest percentage of studies with randomized controlled trials involved parent training interventions, where seven of nine (78%) studies were conducted using this design. Collectively, our review shows that beneficial effects can be realized when non-specialist providers deliver psychosocial interventions to children with intellectual disabilities or lower-functioning autism spectrum disorders.
Relevance of Findings to Low-Resource Settings
The generation of evidence to inform practices in low-resource contexts, and specifically in LMICs, was part of the rationale for this review. We considered many factors during the scoping of the review to ensure that the results could be applied to LMICs, based on previous work by the World Health Organization's Department of Mental Health and Substance Abuse in developing evidence-based recommendations for LMICs [11],[95]. First, we only included studies that reported the outcomes of interventions delivered by non-specialist providers in community-based settings to increase the directness of evidence. All studies about interventions delivered by members of a research team or by specialists were excluded. In addition, by making explicit the information concerning a number of feasibility and contextual issues—including (a) the number of hours of training required to learn treatment techniques, (b) the requirements for supervision of treatment providers, (c) the intensity of interventions, and (d) the professional and education backgrounds of the people delivering the intervention—we allow readers to assess the applicability of the evidence about the various psychosocial interventions to the specific context.
Our findings that psychosocial interventions can be effective when delivered by non-specialist providers have much relevance for improving access to care for children and adolescents with intellectual disabilities or lower-functioning autism spectrum disorders who live in both HICs and LMICs, but they are especially useful in low-resource settings. These findings have the potential to facilitate an increase in access to psychosocial interventions for persons with developmental disorders by promoting task shifting and human resource development approaches. Within this context, the findings from our review that are likely to be most relevant are those from the studies that provided therapies with lower treatment density (e.g., psychosocial interventions requiring less than 10 h per week of direct therapy, or parent training interventions that met for 90 min or less per week). Two behavior analytic studies [66],[67] and nine cognitive rehabilitation, training, and support studies [75]–[80],[82] had treatment densities under 10 h per week (see Figure 10). Generally, the effects shown in these studies were weaker than our overall findings, the exception being the study by Peters-Scheffer et al. [67], which delivered 5 to 10 h of applied behavior analysis on top of standard care, and Elwan and el Din [78], Goetz et al. [79], and Perez and Beltran [82], which all showed very strong effects in development or school performance using inclusion and cognitive training, phonological awareness, and individualized instruction, respectively. Five parent training studies [86],[88],[91]–[93] had treatment densities of less than 90 min per week, with three of five studies showing strong effects [86],[88],[93]. It is also important to note that many of the studies providing high treatment densities involved significant supervision of the treatment providers that was often done by highly trained professionals (e.g., specialists such as psychiatrists and psychologists). The regularity, duration, and density of supervision were not reported in enough detail and with enough consistency for us to draw conclusions about the possible effects on outcome, but Reichow and Wolery [96] found supervisor training to have a significant relation to outcome in a review of early intensive behavioral intervention for young children with autism spectrum disorders. In addition to the training and supervision needs, it is also important to take into account that providing care to children with developmental disorders can be psychologically demanding, and appropriate support mechanisms for non-specialist care providers also need to be established. Uncovering these variables has important and practical implications regarding the feasibility of scaling up these interventions in low-resource settings. A recent review of the most promising procedures used to train paraprofessionals to work with individuals with autism spectrum disorders identified only a small number of studies, and reported the lack of clear training effects [16]. The review suggested that performance feedback can be a potentially effective and efficient means of on-the-job training that requires further research. E-health approaches(i.e., the transfer of health resources and health care by electronic means, including specifically the delivery of information and capacity building to health care providers through the Internet and telecommunications) have the potential to be instrumental in allowing appropriate training and supervision of non-specialist professionals even when resources and the availability of specialists are limited [97].
Relation of Findings to Other Reviews
To our knowledge, this is the first review of psychosocial interventions delivered by non-specialist providers for children with intellectual disabilities or lower-functioning autism spectrum disorders. Therefore, direct comparisons with extant reviews are not possible. However, there have been reviews of psychosocial interventions for children with autism and other neurodevelopmental disorders delivered by specialist providers. Three relevant recent reviews [17]–[19] focused specifically on studies conducted in LMICs. They showed that a small number of studies have been conducted examining psychosocial interventions for children with intellectual disabilities or autism spectrum disorders in LMICs, with overall positive effects being shown for the interventions. An extant review on the effectiveness of interventions for child and adolescent mental health problems in primary care showed that there is some evidence that treatment by non-specialist primary health care and community staff is effective, although the number of studies included was limited [98]. Strong findings were shown in our review for behavior analytic techniques, which are supported by many recent reviews [28],[99],[100]. There have been fewer reviews of what we categorized as cognitive rehabilitation, training, and support; thus, placing our findings in the context of other reviews is difficult. Finally, as with our overall positive findings for parent training interventions, there are a number of reviews suggesting parents are able to learn the skills necessary to deliver therapies to their children and that the children show beneficial effects from these interventions [24],[25]. The findings of our review thus complement the findings of other reviews and have strong relevance for improving care for children with developmental disorders or lower-functioning autism spectrum disorders living in low-resource settings. Collectively, we feel that the findings of our review are well in line with the findings across reviews and that our focus on non-specialist providers allows our review to remain unique and one on which future reviews can build.
Future Directions and Research
Although we located many studies, further research is needed to increase the knowledge of the effects of interventions for children with intellectual disabilities or lower-functioning autism spectrum disorders delivered by non-specialist providers to better inform strategies for service and human resource development. First, future studies should aim to use true experimental designs (randomized controlled trials) with high ecological validity to increase confidence in the effects of this class of interventions. Second, research looking at the effectiveness of capacity building strategies (including distance learning and e-health approaches for training and supervision) in improving non-specialists' ability to deliver psychosocial interventions, and at the quality of care received by children with developmental disorders, is needed. Third, research is needed on delivery strategies and resource requirements for providing psychosocial interventions for developmental disorders in low-resource settings as part of existing primary health care systems. Fourth, research on mediators and moderators of treatment effects is needed to identify the active and necessary components of treatment models [26]. Finally, research in all of these areas conducted specifically in LMICs will be most valuable in informing future care for persons with intellectual disabilities and lower-functioning autism spectrum disorders in areas with limited resources.
Limitations
Although we took many steps, including protocol registry and use of the PRISMA checklist [20] (see Checklist S1), to ensure our review process limited potential sources of bias, no review is without limitation. One limiting factor of all systematic reviews is the quality of the included studies. The inclusion of non-randomized trials in and of itself introduces potential bias [31], and thus must be considered a limitation, although recent work has suggested non-randomized studies with high ecological validity can be an important and valid source of evidence [101]. The inclusion of both randomized and non-randomized trials and the variability of intervention techniques and outcomes precluded synthesizing studies statistically, which can also be seen as a limitation. Instead, we chose to present graphical depictions of effect using harvest plots, which highlighted that there was strong support from randomized controlled trials for parent training interventions to improve developmental, behavioral, and family outcomes. With respect to other risks of bias, as shown in Figures 2 and S1, no study was free of all risks of bias, which has potential impacts on the conclusions reached in this review. Of particular concern is the risk of performance bias, which, by the nature of psychosocial interventions, was high across all studies and must be considered a limitation and taken into consideration when interpreting the findings of this review. Another potential limitation is that most of the studies were conducted in North America or Europe, in HICs. Our stated purpose was to develop recommendations for LMICs, and the lack of ecological validity renders this difficult. It should be noted that almost half of the parent training studies were conducted using randomized controlled trials in LMICs, which might provide the most relevant findings from which to draw conclusions. It should also be noted that many of the non-specialist providers do in fact receive training, e.g., a teacher typically attends a college or university education program and often obtains licensure. However, many of these individuals might not have received the often extensive amounts of training to develop the skills to provide treatments to individuals with intellectual disabilities or lower-functioning autism spectrum disorders that specialist receive. We also cannot rule out the possibility of publication bias, as it was beyond the scope of this project to locate studies published in gray material. We tried to counter this with an extensive search across numerous global and localized databases. Finally, we limited the participant population to individuals who had an intellectual disability, which might limit the generalizability of our results to other populations of individuals with other developmental disorders, including those with higher-functioning autism spectrum disorders.
Conclusion
The findings of this review support the delivery of psychosocial interventions by non-specialist providers to children who have intellectual disabilities or lower-functioning autism spectrum disorders. For the behavior analytic interventions, the best outcomes were shown for development and daily skills; cognitive rehabilitation, training, and support were found to be most effective for improving developmental outcomes, and parent training interventions to be most effective for improving developmental, behavioral, and family outcomes. We also conducted additional subgroup analyses using harvest plots. Given the scarcity of specialists in many low-resource settings, including many LMICs, these findings may provide guidance for scale-up efforts for improving outcomes for children with developmental disorders or lower-functioning autism spectrum disorders.
Supporting Information
Zdroje
1. World Health Organization (1992) The international classification of diseases. Geneva: World Health Organization.
2. TotsikaV, HastingsR, EmersonE, LancasterG, BerridgeD (2011) A population-based investigation of behavioral and emotional problems and maternal mental health: associations with autism spectrum disorder and intellectual disability. J Child Psychol Psychiatry 52 : 91–99.
3. MaulikPK, MascarenhasMN, MathersCD, DuaT, SaxenaS (2011) Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil 32 : 419–436.
4. MurrayPJL, VosT, LozanoR, NaghaviM, FlaxmanAD, et al. (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 : 2197–2223.
5. KielingC, Baker-HenninghamH, BelferM, ContiG, ErtemI, et al. (2011) Child and adolescent mental health worldwide: evidence for action. Lancet 378 : 1515–1525.
6. DemyttenaereK, BruffaertsR, Posada-VillaJ, GasquetI, KovessV, et al. (2004) Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 291 : 2581–2590.
7. World Health Organization (2007) Atlas: global resources for persons with intellectual disabilities. Geneva: World Health Organization.
8. EatonJ, McCayL, SemrauM, ChatterjeeS, BainganaF, et al. (2011) Scale up of services for mental health in low-income and middle-income countries. Lancet 378 : 1592–1603.
9. PatelV, GoelDS, DesaiR (2009) Scaling up services for mental and neurological disorders in low-resource settings. Int Health 1 : 37.
10. World Health Organization (2011) Mental health atlas 2011. Geneva: World Health Organization.
11. DuaT, BarbuiC, ClarkN, FleischmannA, PoznyakV, et al. (2011) Evidence-based guidelines for mental, neurological, and substance use disorders in low - and middle-income countries: Summary of WHO recommendations. PLoS Med 8: e1001122 doi:10.1371/journal.pmed.1001122
12. PatelV, KielingC, MaulikPK, DivanG (2013) Improving access to care for children with mental disorders: a global perspective. Arch Dis Child 98 : 323–327.
13. CollinsPY, PatelV, JoestleSS, MarchD, InselTR, et al. (2011) Grand challenges in global mental health. Nature 475 : 27–30.
14. FlisherAJ, SorsdahlK, HatherillS, ChehilS (2010) Packages of care for attention-deficit hyperactivity disorder in low - and middle-income countries. PLoS Med 7: e1000235 doi:10.1371/journal.pmed.1000235
15. RahmanA, MalikA, SikanderS, RobertsC, CreedF (2008) Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet 372 : 902–909.
16. RispoliM, NeelyL, LangR, GanzJB (2011) Training paraprofessionals to implement interventions for people with autism spectrum disorders: a systematic review. Dev Neurorhabil 14 : 378–388.
17. HastingsRP, RobertsonJ, YasamyMT (2012) Interventions for children with pervasive developmental disorders in low and middle income countries. J Appl Res Intellect Disabil 25 : 119–134.
18. EinfeldSL, StancliffeRJ, GrayKM, SofronoffK, RiceL, et al. (2012) Interventions provided by parents for children with intellectual disabilities in low and middle income countries. J Appl Res Intellect Disabil 25 : 135–142.
19. RobertsonJ, EmersonE, HattonC, YasamyMT (2012) Efficacy of community-based rehabilitation for children with or at significant risk of intellectual disabilities in low-and middle-income countries: a review. J Appl Res Intellect Disabil 25 : 143–154.
20. MoherD, LiberatiA, TetzlaffJ, AltmanDG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097 doi:10.1371/journal.pmed.1000097
21. Sterne JAC, Egger M, Moher D (2008) Addressing reporting biases. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Chichester (UK): John Wiley & Sons. pp. 297–333.
22. DiggleTTJ, McConachieHHR (2002) Parent-mediated early intervention for young children with autism spectrum disorder. Cochrane Database Syst Rev 2002: CD003496.
23. GreyIM, HastingsRP (2005) Evidence-based practices in intellectual disability and behaviour disorders. Curr Opin Psychiatry 18 : 469–475.
24. MatsonJL, MahanS, LoVulloSV (2009) Parent training: a review of methods for children with developmental disabilities. Res Dev Disabil 30 : 961–968.
25. McConachieH, DiggleT (2007) Parent implemented early intervention for young children with autism spectrum disorder: a systematic review. J Eval Clin Pract 13 : 120–129.
26. OdomSL, BoydBA, HallLJ, HumeK (2010) Evaluation of comprehensive treatment models for individuals with autism spectrum disorders. J Autism Dev Disord 40 : 425–436.
27. ReichowB (2012) Overview of reviews: early intensive behavioral interventions for children with autism spectrum disorders. J Autism Dev Disord 42 : 512–520.
28. RogersSJ, VismaraLA (2008) Evidence-based comprehensive treatments for early autism. J Clin Child Adolesc Psychol 37 : 8–38.
29. Higgins JPT, Altman DG (2008) Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Chichester (UK): John Wiley & Sons.
30. Reeves BC, Deeks JJ, Higgins JPT, Wells GA (2008) Including non-randomized studies. In: Higgins JPT, Green S, editors. Cochrane handbook of systematic reviews of interventions. Chichester (UK): John Wiley & Sons.
31. ReevesBC, HigginsJPT, RamsayC, SheaB, TugwellP, et al. (2013) An introduction to methodological issues when including non-randomised studies in systematic reviews on the effects of interventions. Res Synth Methods 4 : 1–11.
32. Lipsey MW, Wilson DB (2001) Practical meta-analysis. Thousand Oaks (California): Sage.
33. Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edition. Hillsdale (New Jersey): Lawrence Erlbaum Associates.
34. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2009) Introduction to meta-analysis. Chichester (UK): John Wiley & Sons.
35. CrowtherM, AvenellA, MacLennanG, MowattG (2011) A further use for the harvest plot: a novel method for the presentation of data syntheses. Res Synth Methods 2 : 79–83.
36. OgilivieD, FayterD, PetticrewM, SowdenA, ThomasS, et al. (2008) The harvest plot: a method for synthesizing evidence about the differential effects of interventions. BMC Med Res Methodol 25 : 8.
37. Mullen EM (1995) Mullen scales of early learning: AGS edition. Circle Pines (Minnesota): American Guidance Service.
38. Bayley N (1993) Bayley scales of infant development, 2nd edition. San Antonio (Texas): The Psychological Corporation.
39. Brunet O, L'ezine I (1955) Echelle de developpement psychomoteur de la premiere enfance. Clamart (France): Editions Scientifiques et Psychotechniques.
40. Alpern G, Boll T, Shearer M (1986) Developmental profile II (DP-II). Los Angeles (California): Western Psychological Services.
41. Thorndike RL, Hagen EP, Sattler JM (1986) The Stanford-Binet intelligence scale, 4th edition. Chicago (Illinois): Riverside.
42. Stutsman R (1948) Merrill Palmer scale of mental tests. Wood Dale (Illinois): Stoelting.
43. Elliott C (1990) The DAS administration and scoring manual. San Antonio (Texas): The Psychological Corporation.
44. Schopler E, Reichler RJ, Bashford A, Lansing MD, Marcus LM (1990) The psychoeducational profile–revised (PEP-R). Austin (Texas): PRO-ED.
45. Wechsler D (1989) Wechsler preschool and primary scale of intelligence–revised. San Antonio (Texas): The Psychological Corporation.
46. Voress JK, Maddox T (1998) Developmental assessment of young children. Austin (Texas): PRO-ED.
47. Roid G, Miller L (1997) Leiter international performance scale–revised. Wood Dale (Illinois): Stoelting.
48. Reynell JK, Gruber GP (1990) Reynell developmental language scales. Los Angeles (California): Western Psychological Services.
49. Dunn LM, Dunn DM (1997) Peabody picture vocabulary test, 3rd edition. Circle Pines (Minnesota): American Guidance Service.
50. Rossetti L (1990) The Rossetti Infant-Toddler Language Scale: a measure of communication and interaction. East Moline (Illinois): Linguisystems.
51. Bzoch K, League R (1991) Receptive expressive emergent language scales–revised (REEL-2). Austin (Texas): PRO-ED.
52. Zimmerman IL, Steiner VG, Pond RE (1992) The preschool language scale–3. San Antonio (Texas): The Psychological Corporation.
53. Provence S, Eriksen J, Vater S, Palmeri S (1985) Infant toddler developmental assessment. Chicago (Illinois): Riverside Publishing.
54. Hendrick D, Prather E, Tobin A (1984) Sequenced inventory of communication development–revised edition. Seattle (Washington): University of Washington Press.
55. Brownell R (2000) Expressive one-word picture vocabulary test. Novato (California): Academic Therapy.
56. Brownell R (2000) Receptive one-word picture vocabulary test. Novato (California): Academic Therapy.
57. Mundy P, Hogan A, Dohering P (1996) A preliminary manual for the abridged Early Social Communication Scales. Coral Gables (Florida): University of Miami.
58. Fenson L, Dale PS, Reznick JS, Bates E, Thal D (1993) MacArthur Communicative Development Inventories: user's guide and technical manual. San Diego: Singular Publishing Group.
59. Sparrow SS, Balla DA, Cicchetti DV (1984) The Vineland adaptive behavior scales–interview edition. Circle Pines (Minnesota): American Guidance Service.
60. CohenH, Amerine-DickensM, SmithT (2006) Early intensive behavioral treatment: replication of the UCLA model in a community setting. J Dev Behav Pediatr 27: S145–S155.
61. DawsonG, RogersS, MunsonJ, SmithM, WinterJ, et al. (2010) Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics 125: e17–e23.
62. EikesethS, SmithT, JahrE, EldevikS (2007) Outcome for children with autism who began intensive behavioral treatment between ages 4 and 7: a comparison controlled study. Behav Modif 31 : 264–278.
63. EikesethS, KlintwallL, JahrE, KarlssonP (2012) Outcome for children with autism receiving early and intensive behavioral intervention in mainstream preschool and kindergarten settings. Res Autism Spectr Disord 6 : 829–835.
64. HowardJS, SparkmanCR, CohenHG, GreenG, StanislawH (2005) A comparison of intensive behavior analytic and eclectic treatments for young children with autism. Res Dev Disabil 26 : 359–383.
65. JocelynLJ, CasiroOG, BeattieD, BowJ, KneiszJ (1998) Treatment of children with autism: a randomized controlled trial to evaluate a caregiver-based intervention program in community day-care centers. J Dev Behav Pediatr 19 : 326–334.
66. KaaleA, SmithL, SponheimE (2012) A randomized controlled trial of preschool-based joint attention intervention for children with autism. J Child Psychol Psychiatry 53 : 97–105.
67. Peters-SchefferN, DiddenR, MuldersM, KorziliusH (2010) Low intensity behavioral treatment supplementing preschool services for young children with autism spectrum disorders and severe to mild intellectual disability. Res Dev Disabil 31 : 1678–1684.
68. ReedP, OsborneLA, CornessM (2007) Brief report: relative effectiveness of different home-based behavioral approaches to early teaching intervention. J Autism Dev Disord 37 : 1815–1821.
69. RemingtonB, HastingsRP, KovshoffH, degli EspinosaF, JahrE, et al. (2007) Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 112 : 418–438.
70. SmithT, GroenAD, WynnJW (2000) Randomized trial of intensive early intervention for children with pervasive developmental disorder. Am J Ment Retard 105 : 269–285.
71. DawsonG, JonesEJH, MerkleK, VenemaK, LowyR, et al. (2012) Early behavioral intervention is associated with normalized brain activity in young children with autism. J Am Acad Child Adolesc Psychiatry 51 : 1150–1159.
72. EikesethS, SmithT, JahrE, EldevikS (2002) Intensive behavioral treatment at school for 4 - to 7-year-old children with autism: a 1-year comparison controlled study. Behav Modif 26 : 49–68.
73. GrindleCF, HastingsRP, SavilleM, HughesJC, HuxleyK, et al. (2012) Outcomes of a behavioral education model for children with autism in a mainstream school setting. Behav Modif 36 : 298–319.
74. BaerDM, WolfMM, RisleyTR (1968) Some current dimensions of applied behavior analysis. J Appl Behav Anal 1 : 91–97.
75. AllorJH, MathesPG, RobertsJ, CheathamJP, ChamplinTM (2010) Comprehensive reading instruction for students with intellectual disabilities: findings from the first three years of a longitudinal study. Psychol Sch 47 : 445–466.
76. BrowderD, Ahlgrim-DelzellL, FlowersC, BakerJ (2012) An evaluation of a multicomponent early literacy program for students with severe developmental disabilities. Remedial Spec Educ 33 : 237–246.
77. BurgoyneK, DuffFJ, ClarkePJ, BuckleyS, SnowlingMJ, et al. (2012) Efficacy of a reading and language intervention for children with Down syndrome: a randomized controlled trial. J Child Psychol Psychiatry 53 : 1044–1053.
78. ElwanF, el DinMN (2010) Impact of integration and a cognitive training program on basic cognitive processes among Egyptian preschoolers with Down syndrome. Dev Disabil Bull 38 : 1–19.
79. GoetzK, HulmeC, BrigstockeS, CarrollJM, NasirL, et al. (2008) Training reading and phoneme awareness skills in children with Down syndrome. Read Writ 21 : 395–412.
80. JepsenRH, VonThadenK (2002) The effect of cognitive education on the performance of students with neurological developmental disabilities. Neurorehabil 17 : 201–209.
81. PaneraiS, ZingaleM, TrubiaG, FinocchiaroM, ZuccarelloR, et al. (2009) Special education versus inclusive education: the role of the TEACCH Program. J Autism Dev Disord 39 : 874–882.
82. PerezLF, BeltranJAJA (2008) A Spanish intervention programme for students with special education needs: effects on intellectual capacity and academic achievement. Eur J Spec Needs Educ 23 : 147–156.
83. TsangSK, ShekDT, LamLL, TangFL, CheungPM (2007) Brief report: application of the TEACCH program on Chinese pre-school children with autism—does culture make a difference? J Autism Dev Disord 37 : 390–396.
84. AllorJH, MathesPG, RobertsJ, JonesFG, ChamplinTM (2010) Teaching students with moderate intellectual disabilities to read: an experimental examination of a comprehensive reading intervention. Educ Train Autism Dev Disabil 45 : 3–22.
85. BrowderDM, Ahlgrim-DelzellL, CourtadeG, GibbsSL, FlowersC (2008) Evaluation of the effectiveness of an early literacy program for students with significant developmental disabilities. Except Child 75 : 33–52.
86. Del GiudiceE, TitomanlioL, BrognaG, BonaccorsoA, RomanoA, et al. (2006) Early intervention for children with Down syndrome in Southern Italy: the role of parent-implemented developmental training. Infants Young Child 19 : 50–58.
87. McConachieH, RandleV, HammalD, Le CouteurA (2005) A controlled trial of a training course for parents of children with suspected autism spectrum disorder. J Pediatrics 147 : 335–340.
88. PlantKM, SandersMR (2007) Reducing problem behavior during care-giving in families of preschool-aged children with developmental disabilities. Res Dev Disabil 28 : 362–385.
89. RobertsC, MazzucchelliT, StudmanL, SandersMR (2006) Behavioral family intervention for children with developmental disabilities and behavioral problems. J Clin Child Adolesc Psychol 35 : 180–193.
90. RussellPS, al JohnJK, LakshmananJL (1999) Family intervention for intellectually disabled children. Randomised controlled trial. Br J Psychiatry 174 : 254–258.
91. ShinJ, NhanN, LeeS, CrittendenK, FloryM, et al. (2009) The effects of a home-based intervention for young children with intellectual disabilities in Vietnam. J Intellect Disabil Res 53 : 339–352.
92. ShuBC, LungFW (2005) The effect of support group on the mental health and quality of life for mothers with autistic children. J Intellect Disabil Res 49 : 47–53.
93. VarmaVK, VermaSK, KapoorP (1992) Evaluation of a home care programme for the mentally retarded children through training of the mother. Indian J Med Res 96 : 29–36.
94. WongVC, KwanQK (2010) Randomized controlled trial for early intervention for autism: a pilot study of the Autism 1-2-3 project. J Autism Dev Disord 40 : 677–688.
95. BarbuiC, DuaT, van OmmerenM, YasamyMT, FleischmanA, et al. (2010) Challenges in developing evidence-based recommendations using the GRADE apprach: the case of mental, neurological, and substance use disorders. PLoS Med 7: e1000322 doi:10.1371/journal.pmed.1000322
96. ReichowB, WoleryM (2009) Comprehensive synthesis of early intensive behavioral interventions for young children with autism based on the UCLA young autism project model. J Autism Dev Disord 39 : 23–41.
97. BoisvertM, LangR, AndrianopoulosM, BoscardinML (2010) Telepractice in the assessment and treatment of individuals with autism spectrum disorders. Dev Neurorhabil 13 : 423–432.
98. BowerP, GarraldaE, KramerT, HarringtonR, SibbaldB (2001) The teatment of child and adolescent mental health problems in primary care: a systematic review. Fam Pract 18 : 373–382.
99. ReichowB, BartonEE, BoydBA, HumeK (2012) Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). Cochrane Database Syst Rev 2012: CD009260.
100. EldevikS, HastingsRP, HughesJC, JahrE, EikesethS, et al. (2009) Meta-analysis of Early Intensive Behavioral Intervention for children with autism. J Clin Child Adolesc Psychol 38 : 439–450.
101. SchunemannHJ, TugwellP, ReevesBC, EklEA, SantessoN, et al. (2013) Non-randomized studies as a source of complementary, sequential, or replacement evidence for randomized controlled trials in systematic reviews on the effects of interventions. Res Synth Methods 4 : 49–62.
102. KasariC, FreemanS, PaparellaT (2006) Joint attention and symbolic play in young children with autism: a randomized controlled intervention study. J Child Psychol Psychiatry 47 : 611–620.
103. Rogers SJ, Dawson G (2009) Early Start Denver Model for young children with autism. New York: Guilford.
104. Lovaas OI (1981) Teaching developmentally disabled children: the me book. Baltimore: University Park.
105. Lovaas OI (2003) Teaching individuals with developmental delays: basic intervention techniques. Austin (Texas): PRO-ED.
106. GreerRD (1997) The comprehensive application of behavior analysis to schooling (CABAS[R]). Behav Soc Issues 7 : 59–63.
107. SundbergML, MichaelJ (2001) The benefits of Skinner's analysis of verbal behavior for children with autism. Behav Modif 25 : 698–724.
108. GreenG, BrennanLC, FeinD (2002) Intensive behavioral treatment for a toddler at high risk for autism. Behav Modif 26 : 69–102.
109. Maurice C, Green G, Luce S (1996) Behavioral intervention for young children with autism: a manual for parents and professionals. Austin (Texas): PRO-ED.
110. Maurice C, Green G, Foxx RM (2001) Making a difference: behavioral intervention for autism. Austin (Texas): PRO-ED.
111. Browder D, Gibbs S, Ahlgrim-Delzell L, Courtade G, Lee A (2007) Early literacy skills builder. Verona (Wisconsin): Attainment Company.
112. Mathes PG, Torgensen JK (2005) Early interventions in reading. Columbus (Ohio): SRA/McGraw-Hill.
113. Mesibov GB, Shea VS, Schopler E (2005) The TEACCH approach to autism spectrum disorders. New York: Springer.
114. Lloyd S (1998) The phonics handbook, 3rd edition. Chigwell (UK): Jolly Learning.
115. HatcherPJ, HulmeC, EllisAW (1994) Ameliorating early reading failure by integrating teaching of reading and phonological skills: the phonological linkage hypothesis. Child Dev 65 : 820–827.
116. Gardner H (1983) Frames of mind: the theory of multiple intelligences. New York: Basic Books.
117. Anderson LW, Krathwohl DRE (2001) A taxonomy for learning, teaching, and assessing: a revision of Bloom's taxonomy of educational objectives. New York: Longman.
118. CESA 5 (2003) Portage guide birth to six: activities and routines for preschoolers. Portage (Wisconsin): CESA 5.
119. SandersMR (1999) Triple P–Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev 2 : 71–90.
120. Sanders MR, Mazzucchelli TG, Studman LJ (2003) Practitioner's manual for standard Stepping Stones Triple P. Brisbane (Australia): Triple P International.
121. Sussman F (1999) More than words: helping parents promote communication and social skills in children with autism spectrum disorder. Toronto: Hanen Centre.
122. Bodfish JW, Symons FJ, Lewis MH (1998) The Repetitive Behavior Scale: a test manual. Morgantown (North Carolina): Western Carolina Research Reports.
123. Bayley N (1969) Bayley scales of infant development. New York: Psychological Corporation.
124. Smith T (1990) Family Satisfaction Questionnaire [unpublished instrument]. Pullman (Washington): Washington State University Department of Psychology.
125. Achenbach TM (1991) Integrative guide for the Child Behavior Checklist L/4-18 YSR, and Teacher Report Form profiles. Burlington (Vermont): University of Vermont Department of Psychiatry.
126. Schafer DS, Moersch MS (1981) Developmental programming for infants and young children. Ann Arbor (Michigan): University of Michigan Press.
127. KrugDA, ArickJ, AlmondP (1980) Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. J Child Psychol Psychiatry 21 : 221–229.
128. SkinnerHA, SteinhauerPD, Santa-BarbaraJ (1983) The family assessment measure. Can J Commun Ment Health 2 : 91–105.
129. MacKayC, CoxT, BurrowsG, LazzeriniT (1978) An inventory for the measurement of self-reported stress and arousal. Br J Soc Clin Psychol 17 : 283–284.
130. Wechsler D (1974) Wechsler intelligence test for children–revised. San Antonio (Texas): The Psychological Corporation.
131. Elliot CD, Smith P, McCulloch K (1996) British ability scales, 2nd edition. London: NFER-Nelson.
132. TasseM, AmanMG, HammerD, RojahnJ (1996) The Nisonger Child Behavior Rating Form: age and gender effects and norms. Res Dev Disabil 7 : 59–75.
133. Einfeld SL, Tonge BJ (2002) Manual for the Developmental Behaviour Checklist, 2nd edition. Melbourne (Australia): University of New South Wales School of Psychiatry.
134. ZigmondAS, SnaithPR (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 63 : 361–370.
135. FriedrichWN, GreenbergMT, CrnicK (1983) A short form of the Questionnaire on Resources and Stress. Am J Ment Defic 88 : 41–48.
136. Behr SK, Murphy DL, Summers JA (1992) User's manual: Kansas Inventory of Parental Perceptions (KIPP). Lawrence (Kansas): University of Kansas Beach Center on Families and Disability.
137. Frankenburg WK (1996) Denver II. Denver Developmental Materials. Denver (Colorado): Denver Developmental Materials.
138. Project RHISE (1979) Rockford Infant Development Evaluation Scales. Bensenville (Illinois): Scholastic Testing Services.
139. Ahlgrim-Delzell L, Browder DM, Flowers C, Baker JN (2008) The nonverbal literacy assessment [abstract]. National Association of School Psychologists 2008 Annual Convention; February 2008; New Orleans, Louisiana, US.
140. Williams KT (1997) Expressive vocabulary test. Circle Pines (Minnesota): American Guidance Service.
141. Hulme C, Stothard SE, Clarke P, Bowyer-Crane C, Harrington A, et al.. (2009) York assessment of reading for comprehension: early reading. London: GL Assessment.
142. Renfrew C (1997) Action picture test. Milton Keynes (UK): Speechmark.
143. Woodcock RW (1991) Woodcock language proficiency battery–revised. Rolling Meadows (Illinois): Riverside Publishing.
144. Wagner R, Torgesen J, Rashotte C (1999) Comprehensive test of phonological processing. Austin (Texas): PRO-ED.
145. Torgesen JK, Wagner RK, Rashotte CA (1999) The test of word reading efficiency. Austin (Texas): PRO-ED.
146. Kaufman AS, Kaufman NL (1983) Kaufman assessment battery for children, interpretative. Circle Pines (Minnesota): American Guidance Service.
147. McCarthy DA (1972) Manual for the McCarthy scales of children's abilities. New York: The Psychological Corporation.
148. CarrollJM, SnowlingMJ (2001) The effects of global similarity between stimuli on children's judgment of rime and alliteration. Appl Psycholinguist 22 : 327–342.
149. Clay M (1985) The early detection of reading difficulties, 3rd edition. Tadworth (UK): Heinemann.
150. ShekDTL, TsangSKM, LamLL, TangFLY, CheungPMP (2005) Psychometric properties of the Chinese version of the Psycho-Educational Profile-Revised (CPEP-R). J Autism Dev Disord 35 : 37–44.
151. Kwok J, Shek DTL, Tse J, Chan S (1989) Hong Kong based adaptive behavior scale. Hong Kong: City Polytechnic of Hong Kong Department of Applied Social Studies.
152. Das JP, Naglieri JA (1997) Cognitive assessment system (CAS). Itasca (Illinois): Riverside Publishing Company.
153. Nihira K, Foster R, Shellhaas M, Leland H (1975) AAMD adaptive behavior scale–revised. Washington (District of Columbia): American Association on Mental Deficiency.
154. Woodcock RW, Mather N (1989) Woodcock-Johnson psychoeducational battery–revised. Allen (Texas): DLM Teaching Resources.
155. Lowe M, Costello A (1988) Symbolic play test manual, 2nd edition. London: NFER-Nelson.
156. FreemanBJ, RitvoER, YokotaA, RitvoA (1986) A scale for rating symptoms of patients with the syndrome of autism in real life settings. J Am Acad Child Psychiatry 25 : 130–136.
157. Abidin R (1995) Parenting stress index: professional manual. Odessa (Florida): Psychological Assessment Resources.
158. Eyberg SM, Pincus D (1999) Eyberg child behavior inventory and Sutter-Eyberg student behavior inventory-revised: professional manual. Odessa (Florida): Psychological Assessment Resources.
159. ArnoldDS, O'LearySG, WolffLS, AckerMM (1993) The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess 5 : 137–144.
160. Gibaud-Wallston J, Wandersman LP (1978) Development and utility of the Parenting Sense of Competency Scale [abstract]. 86th Annual Convention of the American Psychological Association; September 1978; Toronto, Ontario, Canada.
161. Lovibond SH, Lovibond PF (1995) Manual for the depression anxiety stress scales, 2nd edition. Sydney (Australia): Psychology Foundation of Australia.
162. SharpleyCF, RogersHJ (1984) Preliminary validation of the abbreviated Spanier Dyadic Adjustment Scale: some psychometric data regarding a screening test of marital adjustment. Educ Psychol Meas 44 : 1045–1049.
163. Sanders MR, Waugh L, Tully L, Hynes K (1996) The revised family observation schedule, 3rd edition. Brisbane (Australia): Parenting and Family Support Centre.
164. BhattiRS, ChanabasavannaSM, PrabhuLR (1985) A tool to study of parents towards the management of mentally retarded children. Child Psychiatry Q 18 : 1–8.
165. Malin AJ (1969) Malin's intellegence scale for Indian children. Nagpur (India): Child Guidance Center.
166. VermaSK, PershadD, KaushaiP (1972) Gessell's drawing tests as a measure of intelligence in the mentally retarded children. Indian J Ment Retard 5 : 64–68.
167. Verma SK, Pershad D, Randhawa AA (1979) A normative study of children's performance tests of intelligence. Chandigarh (India): Postgraduate Institute of Medical Education and Research.
168. Malin AJ (1968) Vineland social maturity scale: Indian adaptation. Nagpur (India): Child Guidance Center.
169. BhatVK, SinahAK (1978) A rating scale for child behavior: validation of the Hindi version. Indian J Clin Psychol 5 : 25–28.
170. BhatVK, GaubaS (1978) A marital adjustment questionnaire in Hindi. Indian J Clin Psychol 5 : 29–32.
171. PaiS, KapurRL (1981) The burden on the family of a psychiatric patient: development of an interview schedule. Br J Psychiatry 138 : 332–335.
172. RichmondN, GrahamP (1971) A behavioral screening questionnaire for use with three-year-old children: preliminary findings. J Child Psychol Psychiatry 12 : 5–33.
173. JudsonSL, BurdenRL (1980) Towards a tailored measure of parental attitudes: an approach to the evaluation of one aspect of intervention projects with parents of handicapped children. Child Care Health Dev 6 : 47–55.
174. ChengTA, WilliamsP (1986) The design and development of a screening questionnaire (CHQ) for use in community studies of mental disorders in Taiwan. Psychol Med 16 : 415–422.
175. YaoG, ChungCW, YuCF, WangJD (2002) Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J Formos Med Assoc 101 : 342–351.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2013 Číslo 12- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Metabolit živočišné stravy produkovaný střevní mikroflórou zvyšuje riziko závažných kardiovaskulárních příhod
-
Všetky články tohto čísla
- Editors' Wishes for an Illuminated Season and an Open New Year
- Artemisinin Combination Therapy: A Good Antimalarial, but Is the Dose Right?
- Early HIV Infection in the United States: A Virus's Eye View
- Financial Conflicts of Interest and Reporting Bias Regarding the Association between Sugar-Sweetened Beverages and Weight Gain: A Systematic Review of Systematic Reviews
- Investigating the Intersection of Policing and Public Health
- Improving Treatment of Children with Autism Spectrum Disorder in Low- and Middle-Income Countries: The Role of Non-specialist Care Providers
- Data Sharing in a Humanitarian Organization: The Experience of Médecins Sans Frontières
- Why Growing Retractions Are (Mostly) a Good Sign
- Challenges in Addressing Plagiarism in Education
- Experiences with Policing among People Who Inject Drugs in Bangkok, Thailand: A Qualitative Study
- Non-Specialist Psychosocial Interventions for Children and Adolescents with Intellectual Disability or Lower-Functioning Autism Spectrum Disorders: A Systematic Review
- Malaria and Severe Anemia: Thinking beyond
- Financing Essential HIV Services: A New Economic Agenda
- Timing and Completeness of Trial Results Posted at ClinicalTrials.gov and Published in Journals
- Circulating Mitochondrial DNA in Patients in the ICU as a Marker of Mortality: Derivation and Validation
- The Effect of Dosing Regimens on the Antimalarial Efficacy of Dihydroartemisinin-Piperaquine: A Pooled Analysis of Individual Patient Data
- Major Burden of Severe Anemia from Non-Falciparum Malaria Species in Southern Papua: A Hospital-Based Surveillance Study
- HIV-1 Transmission during Early Infection in Men Who Have Sex with Men: A Phylodynamic Analysis
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Artemisinin Combination Therapy: A Good Antimalarial, but Is the Dose Right?
- Circulating Mitochondrial DNA in Patients in the ICU as a Marker of Mortality: Derivation and Validation
- Timing and Completeness of Trial Results Posted at ClinicalTrials.gov and Published in Journals
- Malaria and Severe Anemia: Thinking beyond
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



