-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Monitoring and Evaluating Progress towards Universal Health Coverage in India
article has not abstract
Published in the journal: Monitoring and Evaluating Progress towards Universal Health Coverage in India. PLoS Med 11(9): e32767. doi:10.1371/journal.pmed.1001697
Category: Collection Review
doi: https://doi.org/10.1371/journal.pmed.1001697Summary
article has not abstract
This paper is part of the PLOS Universal Health Coverage Collection. This is the summary of the India country case study. The full paper is available as Supporting Information file Text S1.
Background
Universal Health Coverage (UHC) is gaining in importance across the world. WHO defines UHC as “ensuring that all people can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship” [1]. While many countries have achieved UHC to a large extent, others are still on the path; India being one such country.
Universal Health Coverage: The Policy Context in India
UHC is not a new concept in India. The Bhore committee (1946) had recommended that India should have a health system that “is designed to provide [a full range of health care] for everyone who wishes to use it. ….everyone who uses the new service is assured of ready access to whichever of its branches he or she needs” [2]. However, since then the government has steadily diluted its promise of universal health care. In 1983, it only promised access to “universal provision of comprehensive primary health care services” [3] and in 2002, UHC became reduced to access to “universal immunisation services” [4]. The government's flagship programme National Rural Health Mission (NRHM), launched in 2005, did include strengthening health services, but there was no mention of universal provision of health services [5]. It was only in 2011, when the government of India commissioned a High Level Expert Group (HLEG) that UHC once again entered the lexicon of health policy makers. The HLEG report recommended that India should achieve UHC by 2022 by increasing government finances and by strengthening provision of government health services [6]. This report was accepted by the Planning Commission and is the focus of the health chapter of its 12th five-year plan [7].
Monitoring and Evaluation for UHC
The Ministry of Health (MoH) has a digitised health management information system (HMIS) that collects data every month from all the government health facilities across the country. However, the HMIS has a major weakness; it does not collect information from the private health sector. Since the private sector is the main provider of many health services in India, the HMIS reports are incomplete. Thus policy makers and managers are unable to determine the true health status of the citizens of the country.
To understand the extent to which people are covered by various health services, the policy maker then relies on periodic household surveys administered by independent agencies [8],[9]. Outpatient and inpatient services and health expenditure are captured through the decennial morbidity surveys [10]. Infant mortality rates and occasionally the maternal mortality ratio can be obtained through annual Sample Registration Surveys [11]. Some states have recently started an annual health survey [12].
Progress towards UHC in India
Given the paucity of routine and disaggregated data, it is difficult to assess the status of UHC in India. We used data from household surveys done in 2004, 2005, and 2009 to calculate the population, service, and financial coverage. We selected indicators on the basis of their availability across these surveys. In 2009, only 53% of pregnant women had received three check-ups and only 61% of infants were fully immunised. Disaggregating by socio-economic parameters, shows that only 27% of pregnant women belonging to the poorest quintile had received a full antenatal check-up. Nearly 50% of all women who had an antenatal check-up had to make direct out-of-pocket (OOP) payments for their examination.
Among patients who fell ill, more than 80% sought care at a formal health facility. Similarly more than 70% of women had delivered at a health facility in 2009. However, among the poorest quintile this figure was only 55%. Also, most of the patients or women had to make OOP payments to receive these services (Figure 1).
Fig. 1. Service and financial coverage for outpatient and natal services in India (2004). 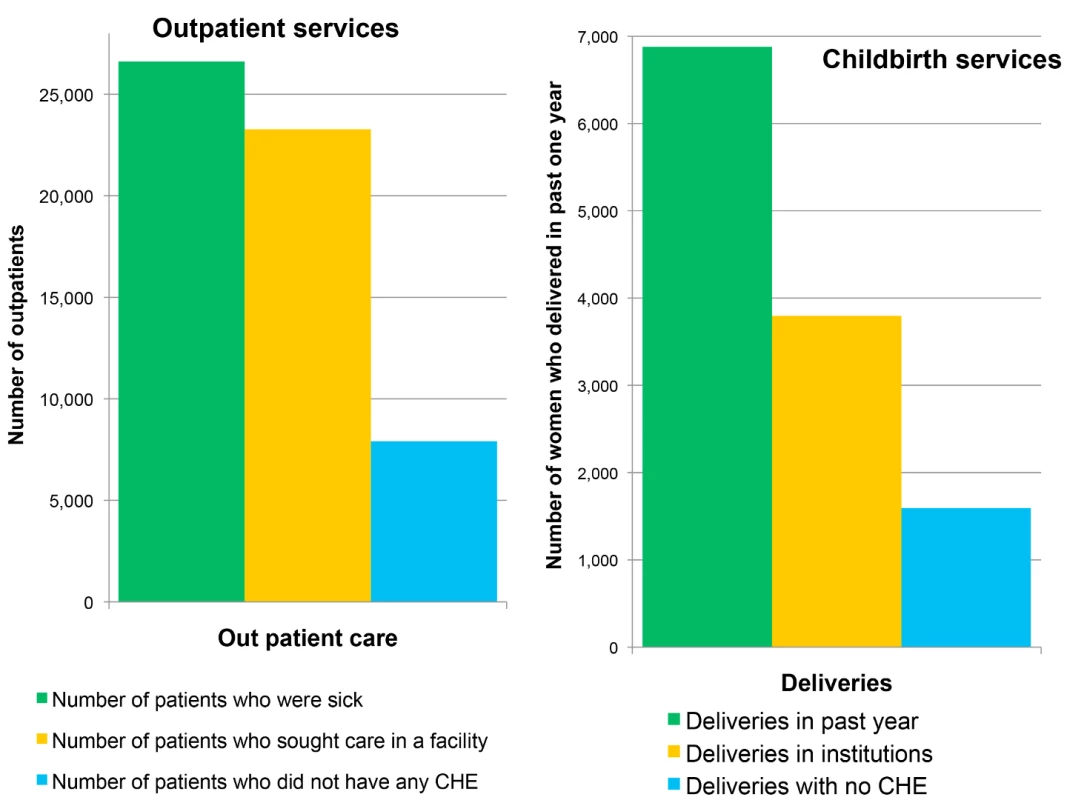
Source: NSS 60th round, 2004 [10]. Only 47% of households in India had access to drinking water within their premises. The rest of the households had to walk distances ranging from 100 metres to a few kilometres to get water.
Conclusions and Recommendations
India has pledged to achieve UHC by 2022. We found that while the population is reasonably covered by preventive and curative health services, financial coverage is lacking for most of these services (Figure 2). When we disaggregate coverage by population subgroups, we consistently find that people living in rural areas, belonging to lower caste households, and having a low economic status use the services much less compared to other groups.
Fig. 2. Universal health coverage for selected health services in India in 2004. 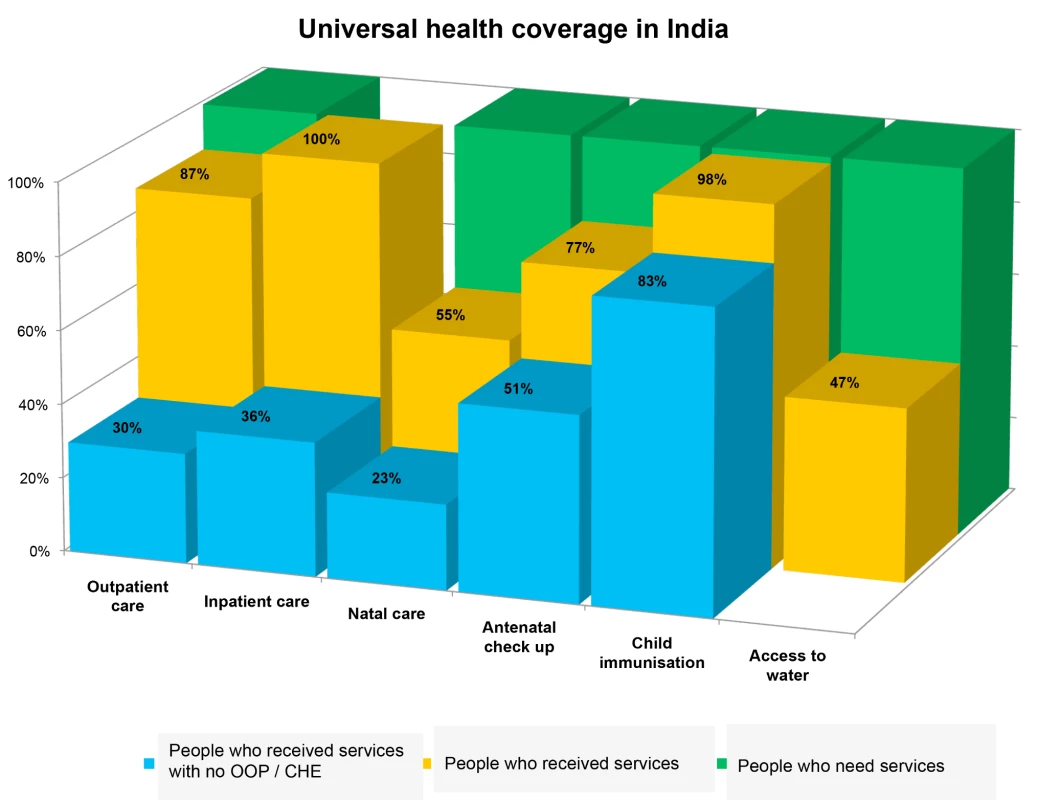
Source: NFHS 3, DLHS 3, NSS 60th round, and Coverage evaluation Survey [8]–[10],[15]. For India to move towards UHC, the first step should be to provide financial protection against medical expenses. Although there are currently many subsidised health insurance schemes for poor people [13], they do not address the main source of OOP payments, which is ambulatory care and medicines [14]. One of the measures that the government of India could take to improve coverage would be to provide access to free medicines for all individuals seeking care, which would reduce OOP payments considerably. The second measure would be to extend existing services to the most vulnerable sections of the population, that is the poorest, aboriginals, and others. With these two measures in place, the government could undertake additional actions to attain UHC. Another important stage would be to monitor progress against specific milestones. Because the current HMIS is inadequate, the government must employ periodic household surveys to capture the necessary information.
Supporting Information
Zdroje
1. WHO (2014) What is universal coverage? Available: http://www.who.int/health_financing/universal_coverage_definition/en/. Accessed 7 April 2014.
2. Bhore J (1946) Report of the health survey and development committee survey Vol 1. New Delhi: Government of India Press.
3. Ministry of Health and Family Welfare (1983) National health policy. New Delhi: Government of India.
4. Ministry of Health and Family Welfare (2002) National health policy 2002. New Delhi: Government of India.
5. Ministry of Health and Family Welfare (2005) National rural health mission. New Delhi.
6. Bang A, Chatterjee M, Dasgupta J, Garg A, Jain Y, et al.. (2012) High level expert group report on Universal Health Coverage for India. New Delhi: Public Health Foundation of India.
7. Planning Commission (2012) Twelfth five year plan (2012–2017): social sectors. New Delhi: Government of India.
8. International Institute for Population Sciences (2007) National family health survey: 2005–06. Mumbai: International Institute for Population Sciences.
9. International Institute for Population Sciences (2009) District level household and facility survey. Mumbai: Government of India.
10. National sample survey organisation (2006) Morbidity, health care and condition of the aged. New Delhi: Government of India.
11. Registrar General of India (2013) Estimated birth rate, death rate and infant mortality rate, 2012. SRS Bull 48 : 1–6.
12. Registrar General and Census Commissioner (2011) Annual health survey 2010–11: Uttar Pradesh. New Delhi: Registrar General and Census Commissioner.
13. La Forgia G, Nagpal S (2012) Government-sponsored health insurance in India: are you covered? Washington (D.C.): World Bank. Available: http://elibrary.worldbank.org/content/book/9780821396186.
14. ShaktivelS, KaranA (2010) Deepening health security in India: evidence from national sample surveys since 1980s. Econ Polit Wkly 45 : 55–60.
15. UNICEF (2009) Coverage evaluation survey. New Delhi: UNICEF.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2014 Číslo 9- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Nech brouka žít… Ať žije astma!
- Intermitentní hladovění v prevenci a léčbě chorob
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ghana
- Sorting Reality from What We Think We Know About Breast Cancer in Africa
- The PLOS “Monitoring Universal Health Coverage” Collection: Managing Expectations
- Monitoring and Evaluating Progress towards Universal Health Coverage in India
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tanzania
- Monitoring and Evaluating Progress towards Universal Health Coverage in Brazil
- Monitoring and Evaluating Progress towards Universal Health Coverage in Thailand
- Monitoring and Evaluating Progress towards Universal Health Coverage in Estonia
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Prioritizing Pregnant Women for Long-Lasting Insecticide Treated Nets through Antenatal Care Clinics
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
- Convergence of Mortality Rates among Patients on Antiretroviral Therapy in South Africa and North America
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Beyond UHC: Monitoring Health and Social Protection Coverage in the Context of Tuberculosis Care and Prevention
- Intimate Partner Violence and Reproductive Coercion: Global Barriers to Women's Reproductive Control
- Genetic Predisposition to Increased Blood Cholesterol and Triglyceride Lipid Levels and Risk of Alzheimer Disease: A Mendelian Randomization Analysis
- Readmissions after Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia among Young and Middle-Aged Adults: A Retrospective Observational Cohort Study
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Infected Women Receiving Cotrimoxazole Prophylaxis: A Multicenter Randomized Placebo-Controlled Trial
- Equity-Oriented Monitoring in the Context of Universal Health Coverage
- The Clinical and Economic Impact of Point-of-Care CD4 Testing in Mozambique and Other Resource-Limited Settings: A Cost-Effectiveness Analysis
- Effective Coverage: A Metric for Monitoring Universal Health Coverage
- Mortality in Patients with HIV-1 Infection Starting Antiretroviral Therapy in South Africa, Europe, or North America: A Collaborative Analysis of Prospective Studies
- Global Financing and Long-Term Technical Assistance for Multidrug-Resistant Tuberculosis: Scaling Up Access to Treatment
- Oral Cholera Vaccine Development and Use in Vietnam
- Monitoring and Evaluating Progress towards Universal Health Coverage in Bangladesh
- Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ethiopia
- Preventing Acute Malnutrition in Young Children: Improving the Evidence for Current and Future Practice
- Monitoring and Evaluating Progress towards Universal Health Coverage in Singapore
- Monitoring and Evaluating Progress towards Universal Health Coverage in China
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tunisia
- Receptor-Defined Subtypes of Breast Cancer in Indigenous Populations in Africa: A Systematic Review and Meta-Analysis
- WHO Essential Medicines Policies and Use in Developing and Transitional Countries: An Analysis of Reported Policy Implementation and Medicines Use Surveys
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Negative Women: A Multicentre Randomized Controlled Trial
- Preventing Acute Malnutrition among Young Children in Crises: A Prospective Intervention Study in Niger
- Monitoring Progress towards Universal Health Coverage at Country and Global Levels
- Monitoring Intervention Coverage in the Context of Universal Health Coverage
- Regular Breakfast Consumption and Type 2 Diabetes Risk Markers in 9- to 10-Year-Old Children in the Child Heart and Health Study in England (CHASE): A Cross-Sectional Analysis
- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



