-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa
article has not abstract
Published in the journal: Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa. PLoS Med 11(9): e32767. doi:10.1371/journal.pmed.1001686
Category: Collection Review
doi: https://doi.org/10.1371/journal.pmed.1001686Summary
article has not abstract
This paper is part of the PLOS Universal Health Coverage Collection. This is the summary of the South Africa country case study. The full paper is available as Supporting Information file Text S1.
Background
South Africa's colonial and apartheid inheritance is one of substantial social, economic, and health inequalities [1]. Since the first democratic elections in 1994, the human development index has declined considerably, largely because of the HIV epidemic, which has reduced life expectancy. The South African government has committed to a universal health system, which is seen as critical to improve population health and redress inequalities [2].
Universal Health Coverage: The Policy Context
South Africa (SA) has a divided health system, with the minority of the population using private health services, particularly if covered by private voluntary health insurance (approximately 17% of the population), and the remainder of the population relying mainly on tax-funded health services [1],[3]. Many South Africans face health service access constraints.
A green paper published in late 2011 mapped out policies to move towards universal health coverage (UHC) over a 15-year period [2]. In the first phase, the emphasis is on investing in improving access to and the management and quality of public sector health services, particularly at the primary health care level. A range of activities has been initiated, driven by the very active leadership of the current minister of health. The second phase is intended to introduce a strategic purchasing mechanism, by establishing a semi-autonomous National Health Insurance Fund (NHIF). Although termed a National Health Insurance (NHI), it would be tax funded, through allocations from general tax revenue and possibly additional earmarked taxes. It is envisaged that the NHIF will create a universal entitlement to comprehensive health services, to be accessed through primary health care (PHC) gatekeepers and following referral routes.
Monitoring and Evaluation for UHC
As SA is at an early stage in its UHC reforms, it does not have an explicit UHC monitoring and evaluation framework or system. While there are a number of administrative systems (such as the District Health Information System) and household surveys that can be used for UHC assessment, there are several challenges and deficiencies with the data [4]. Data from routine administrative systems are frequently inaccessible outside of government departments and of questionable data quality. There are also limitations in terms of equity analyses; most indicators of relevance to monitoring UHC progress can only be disaggregated by geographic area (province and sometimes district), with few indicators able to be disaggregated by other equity stratifiers, such as income and gender.
Progress towards UHC in South Africa
Given that UHC reforms have only recently begun to be implemented, it is not feasible to assess progress in this regard. We were, however, able to assess South Africa's status relative to the goals of UHC, by drawing on some suggested international benchmarks. In relation to service inputs, SA is well below the WHO's Service Availability and Readiness Assessment (SARA) benchmark for inpatient beds (17 beds per 10,000 population in SA; 25 per 10,000 recommended by SARA). While SA is slightly above the SARA benchmark for core personnel (25 per 10,000 population in SA; SARA, 23 per 10,000), there are considerable variations in the distribution of health workers among geographic areas. There are also disparities across geographic areas in other inputs (e.g., per capita public spending on PHC services), outputs (such as utilisation rates), and health outcomes [4].
From a UHC perspective, an indicator of particular importance is that of health service utilisation, as it provides insights into the extent to which people have access to care. The SARA benchmarks are five outpatient visits per person and 100 inpatient discharges per 1,000 population per year. While overall utilisation rates in SA appear to be in line with these benchmarks (4.2 outpatient visits and 95 inpatient admissions in either public or private facilities), Figure 1 highlights substantial differences across provinces. Utilisation rates are also lower than the SARA benchmarks for the population dependent on publicly funded services (4.1 outpatient visits and 89 inpatient admissions) yet well above these benchmarks for those with private insurance coverage (5.5 outpatient visits and 139 inpatient admissions) [5]. Disparities created by fragmented funding pools are such that the private insurance pool has per capita spending levels that are 6.2 times greater than the tax-funded pool [3].
Fig. 1. Health facility utilisation rates by province, South Africa, 2008. 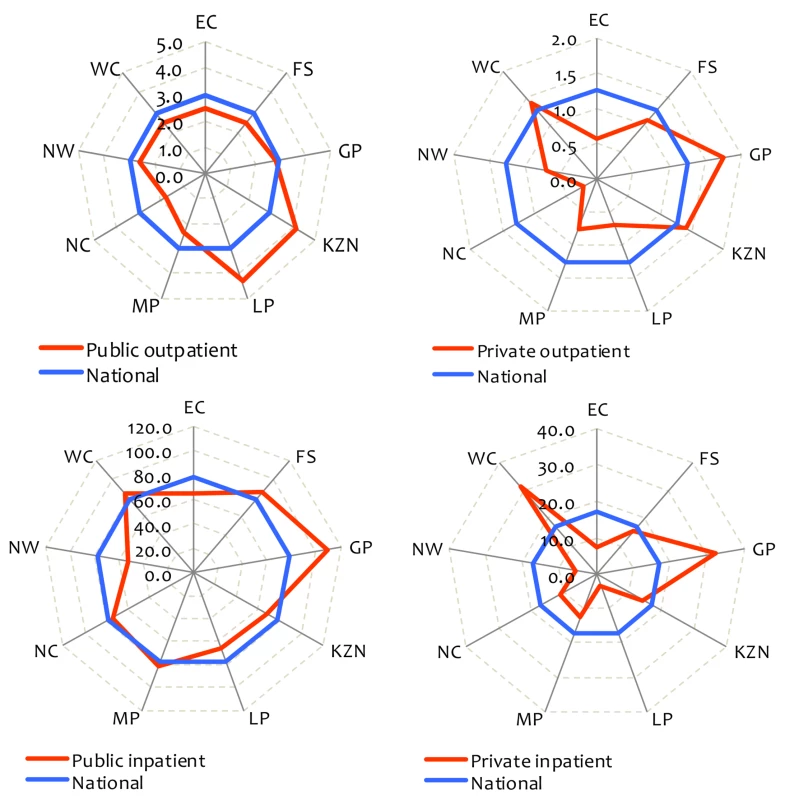
Outpatient and inpatient utilisation are visits per person and admissions per 1,000 population per year, respectively. The provinces are Eastern Cape (EC), Free State (FS), Gauteng (GP), KwaZulu-Natal (KZN), Limpopo (LP), Mpumalanga (MP), Northern Cape (NC), North West (NW), and Western Cape (WC). Source: Alaba and McIntyre [5]. Financial protection is also of importance from a UHC perspective. Although levels of impoverishment from out-of-pocket payments in SA are low (Figure 2), they are far greater in the poorer than richest provinces.
Fig. 2. Impoverishment associated with out-of-pocket payments by province in South Africa, 2005/2006. 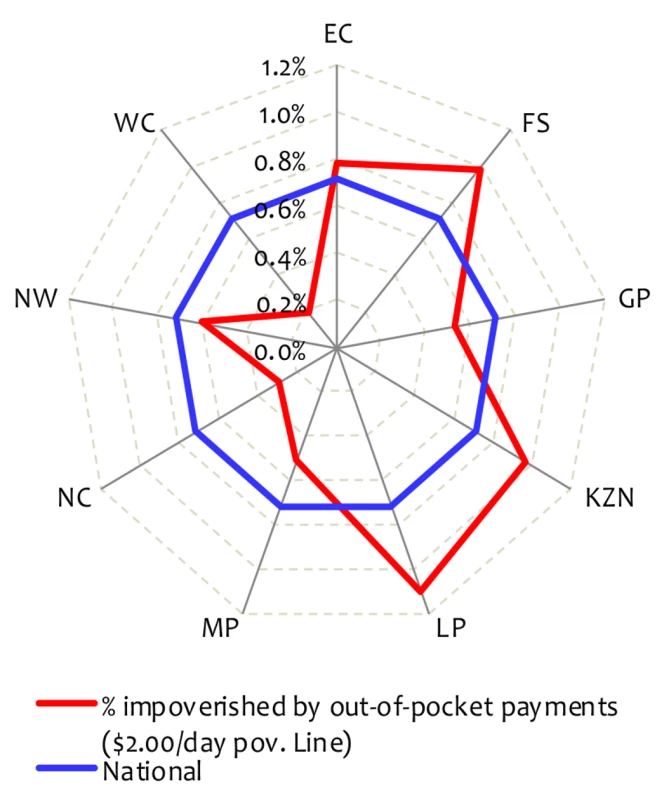
The provinces are Eastern Cape (EC), Free State (FS), Gauteng (GP), KwaZulu-Natal (KZN), Limpopo (LP), Mpumalanga (MP), Northern Cape (NC), North West (NW), and Western Cape (WC). Source: Authors' analysis of Statistics South Africa's Income and Expenditure Survey [6]. Conclusions and Recommendations
To evaluate a country's status relative to UHC goals, it is critical to have UHC-related international benchmarks against which to compare country data. While some benchmarks have been suggested recently, more debate and a consensus on a widely supported set of benchmarks are needed.
It is important for SA to develop an explicit UHC monitoring and evaluation system at an early stage of reform implementation to support the refinement of reforms over time. Given its inheritance of pervasive inequalities, reducing inequalities should be emphasised while moving to UHC. Improvements in information systems and surveys are required to improve data quality, and to allow for disaggregation of indicators by a range of equity stratifiers. In addition, routine administrative data should be made more widely available.
Supporting Information
Zdroje
1. CoovadiaH, JewkesR, BarronP, SandersD, McIntyreD (2009) The health and health system of South Africa: historical roots of current public health challenges. Lancet 374 : 817–834.
2. Department of Health (2011) National Health Act (61/2003): Policy on National Health Insurance. Government Gazette 34523. Pretoria: National Department of Health, Republic of South Africa.
3. AtagubaJE, McIntyreD (2012) Paying for and receiving benefits from health services in South Africa: is the health system equitable? Health Policy Plann 27: i35–i45.
4. Day C, Gray A (2013) Health and related indicators. Padarath A, English R, editors. South African Health Review 2012/13. Durban: Health Systems Trust.
5. AlabaOA, McIntyreD (2012) What do we know about health service utilisation in South Africa? Dev Southern Afr 29 : 704–724.
6. Statistics South Africa (2008). Income and expenditure of households 2005/2006 dataset. Pretoria: Statistics South Africa.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2014 Číslo 9- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ghana
- Sorting Reality from What We Think We Know About Breast Cancer in Africa
- The PLOS “Monitoring Universal Health Coverage” Collection: Managing Expectations
- Monitoring and Evaluating Progress towards Universal Health Coverage in India
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tanzania
- Monitoring and Evaluating Progress towards Universal Health Coverage in Brazil
- Monitoring and Evaluating Progress towards Universal Health Coverage in Thailand
- Monitoring and Evaluating Progress towards Universal Health Coverage in Estonia
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Prioritizing Pregnant Women for Long-Lasting Insecticide Treated Nets through Antenatal Care Clinics
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
- Convergence of Mortality Rates among Patients on Antiretroviral Therapy in South Africa and North America
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Beyond UHC: Monitoring Health and Social Protection Coverage in the Context of Tuberculosis Care and Prevention
- Intimate Partner Violence and Reproductive Coercion: Global Barriers to Women's Reproductive Control
- Genetic Predisposition to Increased Blood Cholesterol and Triglyceride Lipid Levels and Risk of Alzheimer Disease: A Mendelian Randomization Analysis
- Readmissions after Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia among Young and Middle-Aged Adults: A Retrospective Observational Cohort Study
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Infected Women Receiving Cotrimoxazole Prophylaxis: A Multicenter Randomized Placebo-Controlled Trial
- Equity-Oriented Monitoring in the Context of Universal Health Coverage
- The Clinical and Economic Impact of Point-of-Care CD4 Testing in Mozambique and Other Resource-Limited Settings: A Cost-Effectiveness Analysis
- Effective Coverage: A Metric for Monitoring Universal Health Coverage
- Mortality in Patients with HIV-1 Infection Starting Antiretroviral Therapy in South Africa, Europe, or North America: A Collaborative Analysis of Prospective Studies
- Global Financing and Long-Term Technical Assistance for Multidrug-Resistant Tuberculosis: Scaling Up Access to Treatment
- Oral Cholera Vaccine Development and Use in Vietnam
- Monitoring and Evaluating Progress towards Universal Health Coverage in Bangladesh
- Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ethiopia
- Preventing Acute Malnutrition in Young Children: Improving the Evidence for Current and Future Practice
- Monitoring and Evaluating Progress towards Universal Health Coverage in Singapore
- Monitoring and Evaluating Progress towards Universal Health Coverage in China
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tunisia
- Receptor-Defined Subtypes of Breast Cancer in Indigenous Populations in Africa: A Systematic Review and Meta-Analysis
- WHO Essential Medicines Policies and Use in Developing and Transitional Countries: An Analysis of Reported Policy Implementation and Medicines Use Surveys
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Negative Women: A Multicentre Randomized Controlled Trial
- Preventing Acute Malnutrition among Young Children in Crises: A Prospective Intervention Study in Niger
- Monitoring Progress towards Universal Health Coverage at Country and Global Levels
- Monitoring Intervention Coverage in the Context of Universal Health Coverage
- Regular Breakfast Consumption and Type 2 Diabetes Risk Markers in 9- to 10-Year-Old Children in the Child Heart and Health Study in England (CHASE): A Cross-Sectional Analysis
- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



