-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Transitioning to Country Ownership of HIV Programs in Rwanda
Agnes Binagwaho and colleagues describe how Rwanda achieved country ownership of its HIV programs.
Published in the journal: Transitioning to Country Ownership of HIV Programs in Rwanda. PLoS Med 13(8): e32767. doi:10.1371/journal.pmed.1002075
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1002075Summary
Agnes Binagwaho and colleagues describe how Rwanda achieved country ownership of its HIV programs.
Summary Points
Funding from the United States President’s Emergency Plan for AIDS Relief (PEPFAR) program in 2004 significantly bolstered Rwanda’s ability to develop a national HIV program with implementing partners.
In 2009, after 5 years of expanding HIV services to achieve universal access to antiretroviral treatment, Rwanda and PEPFAR embarked on a sustainability and country ownership phase of the AIDS response.
Commitment to the following seven principles helped to create a foundation for successful HIV program management transition from implementing nongovernmental partners to management by Rwanda: a political context of integration and decentralization, ownership through national coordination, participation and partnership, equity, efficiency, accountability, and integration of HIV care to strengthen the entire health system.
Introduction
An objective of development aid is to increase the capacity of recipient countries until they no longer require foreign assistance. Ideally, partners accompany host countries in this development journey by progressively transferring management skills and technical expertise to promote sustainability of country ownership of programs [1,2]. Reviews of donor-funded health programs have highlighted integration into existing government health systems as key to enabling sustainability [3–6]. However, there are few published analyses of how public health programs are transitioned from donor to host country management [2,7].
As defined through its national policy, Vision 2020, Rwanda has committed to reducing its dependence on external aid [8]. In response to the growing AIDS crisis, Rwanda advocated for increasing resources from bilateral, multilateral, and civil society organizations to combat HIV [9,10]. In 2003, the World Bank and the Global Fund for AIDS, Tuberculosis and Malaria (Global Fund) were among the first contributors to the AIDS response in Rwanda [8–10]. The launch of the US President’s Emergency Plan for AIDS Relief (PEPFAR) program in 2004 dramatically increased the funding available to support HIV programs in Rwanda (Fig 1). PEPFAR provided 989.7 million US dollars (USD) from 2004 to 2013, and the Global Fund provided 529.2 million USD from 2003 to 2013 [9–12].
Fig. 1. Total PEPFAR approved funding to Rwanda for HIV, tuberculosis (TB)/HIV, and health systems strengthening, 2004–2013. 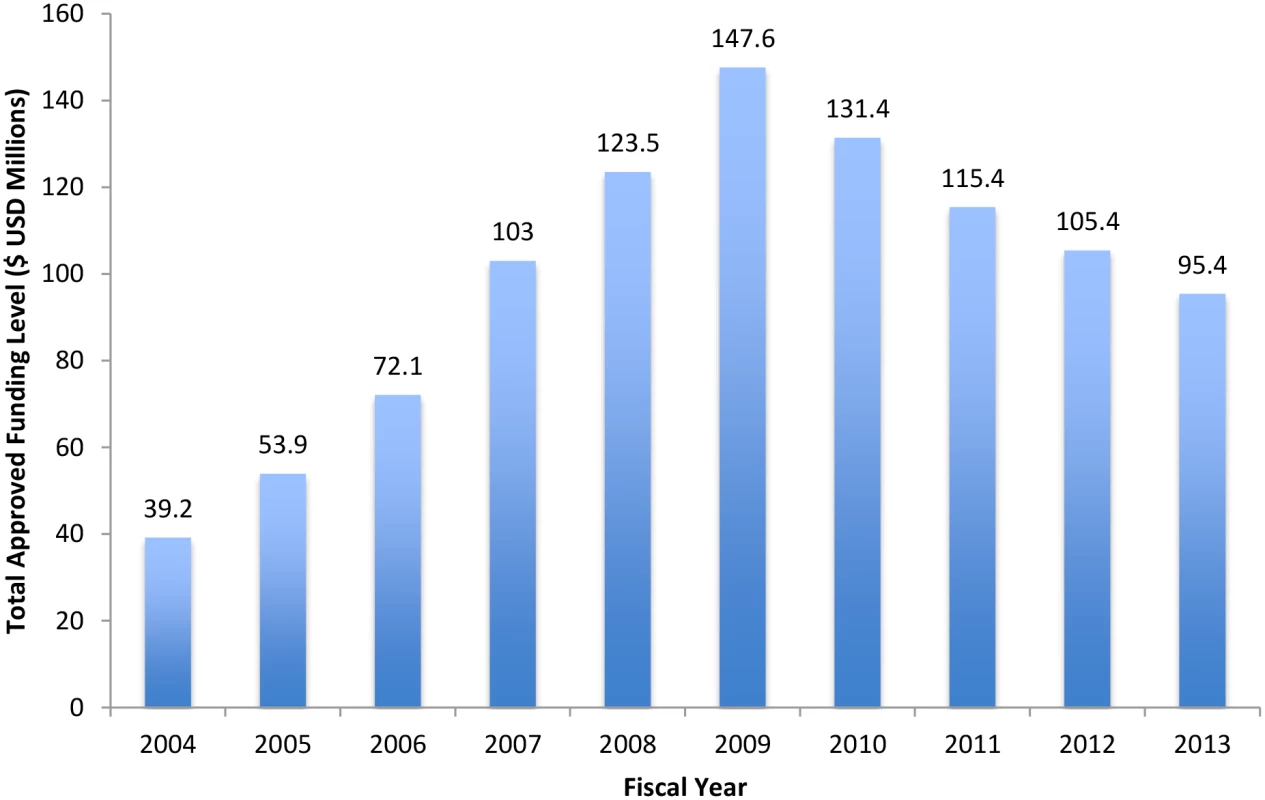
Sources: FY2004–2011: http://www.pepfar.gov/documents/organization/199598.pdf; 2012: http://www.pepfar.gov/documents/organization/212155.pdf; 2013: http://www.pepfar.gov/documents/organization/222179.pdf. FY, Fiscal Year. This article describes key principles that allowed for the successful transition of HIV program ownership from the donor-led agencies to Rwanda.
Launching National Scale-up for HIV Care in Rwanda
Through PEPFAR, the US government (USG) developed partnerships with the Government of Rwanda (GOR) for the national AIDS response. Six US agencies managed PEPFAR funds in Rwanda and supported national HIV scale-up programming; the Centers for Disease Control and Prevention (CDC) oversaw in-country implementation of Rwanda’s national HIV program on behalf of the involved Department of Health and Human Services (HHS) agencies. This partnership helped to scale up a national emergency response to the HIV epidemic. Within 5 years, Rwanda’s national HIV program achieved near-universal access to HIV prevention, care, and treatment (Table 1). Rwanda’s decentralized health sector, as well as its policies that permit for task shifting of services, helped to expeditiously provide universal and comprehensive HIV services throughout the country in a geographically equitable manner.
Tab. 1. Key HIV Program Indicators in Rwanda, 2005–2013. 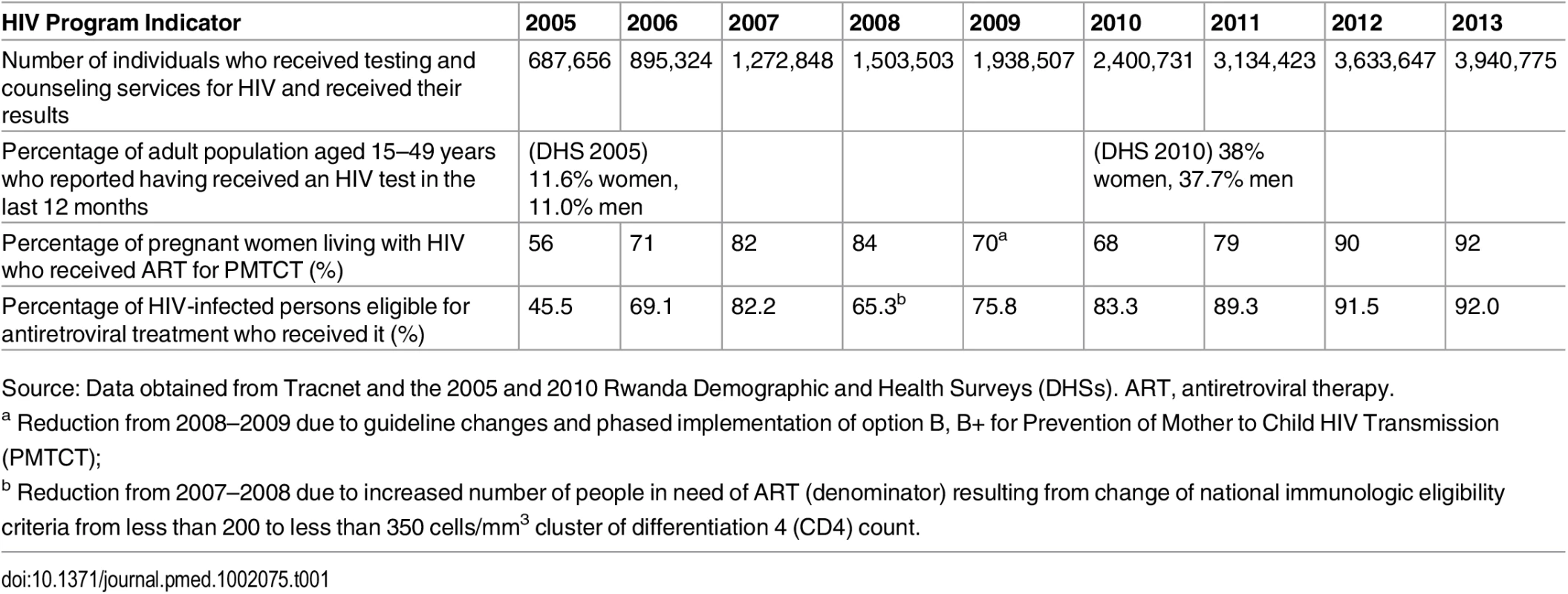
Source: Data obtained from Tracnet and the 2005 and 2010 Rwanda Demographic and Health Surveys (DHSs). ART, antiretroviral therapy. From the onset, GOR sought to expand its involvement in the direct management of its externally funded health and HIV programs given its commitment to national ownership as articulated in Vision 2020 [8]. In 2009, Rwanda and its PEPFAR-funded partners aligned to support a second “sustainability and country ownership” phase of the AIDS response, which promoted the transition of HIV clinical service program leadership from partnering nongovernmental organizations (NGOs) to the host country [1,13]. Key within the transition plan developed by Rwanda and its partners was to allow for direct PEPFAR financing to the host country government. The plan also employed existing PEPFAR-funded international NGOs working in Rwanda and experts in HIV program management to accompany GOR as it learned how to best manage PEPFAR-supported programs. By February 2012, program transition occurred: Rwanda’s Ministry of Health (MOH) became a direct recipient of PEPFAR funds and was responsible for coordinating comprehensive HIV services for nearly 40,000 patients in 76 health facilities.
Prerequisites for Transition: The Foundation for Sustainability
The following seven principles were instrumental in building a foundation that permitted for this successful HIV program leadership transition to occur.
Political Context of Decentralization
Rwanda’s decentralization policy, implemented in 2005, empowers administrative districts, led by mayors, to coordinate all health activities undertaken within their district health facilities and health-oriented NGOs. Rwanda’s network of 45,000 community health workers (CHWs) is the backbone of the country’s health care system, providing care at the village level. This care then integrates with more advanced care provided at health centers in sectors, district hospitals, and referral hospitals at the central level. The decentralized nature of Rwanda’s health system permitted for effective expansion of HIV services to health facilities in districts. For example, the number of health facilities providing Prevention of Mother to Child HIV Transmission (PMTCT) services increased nationwide from 53 in 2003 to 404 in 2011.
Ownership through National Coordination
From the beginning, Rwanda endorsed “the three ones” governance principle for its national AIDS response: one national HIV coordinating body, one national HIV strategic plan, and one national monitoring system [14]. NGOs operating in Rwanda with PEPFAR funding were committed to the long-term objectives in the national plan and aligned their HIV service delivery activities accordingly. Harmonizing HIV service delivery approaches across different NGOs early on expedited the eventual consolidation and transfer of these programs to MOH management.
Participation and Partnership
The national HIV prevention, treatment, and mitigation guidelines were developed through an inclusive, participatory process among key implementation stakeholders (national and international NGOs as well as the beneficiaries). As a result, partners employed the MOH comprehensive HIV treatment protocol, which promoted a common system of procurement and distribution of HIV drugs and consumables. Partners strengthened HIV leadership capacity at MOH through management training, direct skills transfer, and technical support to develop national tools and electronic systems to track HIV program activities at central, health facility, and community levels. This collaboration leveraged synergies across the health sector and accelerated universal access to HIV care and treatment. Further, the sense of solidarity, partnership, and trust between PEPFAR, the international NGOs, and MOH garnered through these experiences was critical for the eventual transition of HIV program leadership from partners to GOR in 2012.
Equity
Before these partnerships existed to support a more robust HIV response in Rwanda, Rwanda’s MOH worked with civil society to develop an equitable approach for allocating limited antiretroviral therapy (ART) for people living with HIV (PLWH). Each health facility providing ART created an enrollment committee comprised of health professionals, social workers, and representatives of local associations of PLWH to ensure that the most vulnerable had access to treatment. Once there was sufficient treatment for all through PEPFAR funding, this committee was transformed into a therapeutic committee to improve support for PLWH retention in treatment. Moreover, from 2003 onwards, to assure equitable geographic access to treatment, GOR coordinated with its partnering NGOs to assume regional responsibilities. To ensure adequate staffing of these new HIV clinics that were being created to optimize geographic equity to care, a complementary program to build an appropriately trained workforce was developed. This assured the delivery of sophisticated HIV health services in remote areas, facilitating PLWH to be treated near their own communities by Rwandan health professionals under the authority of their own local governmental leaders.
Efficiency
Operationalizing the geographic mandate of NGO partners reduced implementation costs and promoted efficiency by discouraging duplication and improving coordination. In addition, the national plan required that each NGO partner undertake the full range of HIV services and support supervision, training, and mentorship in an integrated manner. This approach reduced the number of partners and logistics - and transport-related costs, all of which helped to streamline the transition process to host country ownership of the HIV delivery system. In addition, GOR implemented nationally approved salary structures for health personnel in all facilities. By adhering to this salary policy, NGO partners helped to promote staff retention across facilities; this simplified the transition process as health personnel status and salaries remained unaffected once MOH assumed responsibilities for HIV program management in 2012.
Accountability
Rwanda has implemented a number of transparency, anticorruption, and quality assurance policies for all sectors, including health [15,16]. In 2003, the National AIDS Control Commission created a project management unit to oversee the donor funds for the HIV response directly managed by GOR. However, at the time, Rwandan health institutions had limited financial and administrative capacity to manage the program. Thus, to rapidly implement HIV programs funded by PEPFAR, the USG provided funding directly to international NGOs (rather than directly to GOR) to support the expansion of HIV-related services. Over time, these partnering NGOs helped build the administrative and programmatic capacity of Rwandan institutions at the central, district, health facility, and community levels, with an emphasis on accountability for results.
Rwanda’s HIV program performance improved steadily over the first 5 years of PEPFAR funding (Table 1) [17]. The quality of Rwanda’s HIV program and financial management systems improved over this period, and donor confidence in its administrative and reporting mechanisms was bolstered [16]. Moreover, in 2010, Rwanda began to publicly report semiannual budget execution of domestic and development partners’ projects during the MOH Joint Health Sector Review. These efforts laid the groundwork for the establishment of larger direct cooperative agreements between CDC and Rwandan institutions, which was necessary for successfully transitioning HIV program management from NGO partners to GOR.
Integration of HIV Care to Strengthen the Health System
Since 2003, Rwandan and international stakeholders have embraced a shared vision that controlling the HIV epidemic requires integration of HIV services within the existing health system. The national policy was to create a sustainable system for Rwandans to manage HIV services for the long term without creating a parallel service delivery system. Partnering NGOs (such as the International Center for AIDS Care and Treatment Programs [ICAP] at Columbia University and AIDSRelief) supported Rwanda’s national policy and applied the chronic disease model to HIV care as a way to strengthen critical components of the Rwandan health system such as infrastructure, personnel, supply chain, clinical management, information systems, and laboratory services [18]. This alignment with Rwanda’s national policy improved integration of HIV patient services and yielded benefits across the entire health system with respect to HIV funds. This allowed Rwanda to build an integrated health service delivery platform, in which HIV could be addressed as a chronic disease.
Implementing Transition: Overcoming Challenges
Despite the gains made through the effective partnership during the early years of HIV program scale-up, there were several challenges Rwanda encountered when implementing the management transition of PEPFAR-funded HIV programs in 2009.
First, Rwanda’s MOH initially lacked the human resources capacity and technical expertise needed to effectively manage the national scale-up of PEPFAR programs. Despite this limitation, MOH was eager to manage the PEPFAR-funded programs rapidly given the importance of national ownership of critical services delivered in Rwanda. However, during those early years of the emergency response to AIDS, the focus on expanding nationwide access to life-saving care and treatment prevailed over strengthening routine program management capacity. Rwanda could have benefited from taking on more responsibilities for service delivery and reporting even earlier than the transition schedule permitted. This tension between respecting host country ownership and being pragmatic about implementation capacity limitations presented numerous challenges at the onset. Such challenges, however, were overcome through consistent, open communication between GOR and USG partners and the shared vision to optimize access and quality of HIV services provided to all Rwandans in need.
Second, once it became time for implementing NGOs to transition program management to GOR, partners faced an ambitious timeframe to complete this process. Specifically, the transition time mandated by USG meant that between 2009 and 2012, a total of 56,568 HIV-infected patients in care (including 25,206 patients on ART) needed to be transferred to different support systems in a seamless manner and without compromise of the quality of care. To meet this objective, a transition task force was formed, comprised of key Rwanda MOH officials, partner NGOs, and CDC, to both plan and monitor the transition of the 76 health facilities involved with HIV care delivery at the time. A key goal for the task force was to maintain the quality of HIV clinical services throughout the transition, using a jointly agreed timeline with clear performance indicators. The task force conducted readiness, baseline, and follow-up assessments and reviewed program data to identify gaps and areas for improvement. Through reconfiguring staff where needed, meeting regularly with stakeholders, routine visits to health facilities, and improved mentorship and supportive supervision from the central level, the program was transitioned to MOH with sustained clinical and management performance 24 months after transition. This task force illustrates the importance of partners committing to jointly monitoring program performance throughout a transition period. Resource-limited countries are likely to require extensive technical support from partners to reach this decision point. Development partners on the other hand need to be willing to reinforce their support for mentorship, quality improvement, and monitoring and evaluation.
Looking Ahead
Over the past 10 years, Rwanda has developed the expertise and experience to successfully manage a large cohort of HIV-infected individuals, and its clinicians are now able to provide high-quality care to patients at all stages of HIV disease. When PEPFAR partners like ICAP and AIDSRelief transitioned their responsibilities, some of their experienced staff were directly transferred to Rwanda’s MOH to assist in the mentorship of the program managers and health care providers. However, as scientific knowledge advances and HIV prevention and care evolves, Rwanda may still need more advanced technical assistance to help address HIV transmission hot spots, HIV drug resistance, novel drug regimens, improved diagnostic testing methods, and long-term sequelae of HIV and its treatment. The Rwandan government has contracted with more than 20 American academic institutions with the aim to improve the quality of teaching of Rwandan health professionals, in order to be ready for the upcoming changes in the clinical management and quality improvement of the HIV response and to address other health threats [19]. In addition, as the resources for the global HIV response are plateauing and Rwanda’s health sector is mandated to meet diverse health needs of its population, it is important to further prioritize the available resources towards higher-impact interventions in order to achieve greater results. The continued support of development partners is critical as the country finds its way to self-reliance while building a strong health system.
Conclusions
A decade ago, HIV was a mortal threat to the Rwandan people and an overwhelming challenge for the Rwandan health system. Today, Rwanda has a robust system for delivering quality care to all those affected by HIV [20]. This was possible through the collaboration between GOR and its partners to develop a program from the onset that would allow for national ownership, sustainable development, and patient-centered health care [19].
Rwanda’s HIV program transition experience illustrates both the importance of building capacity and systems within host countries to manage programs as well as the importance of jointly monitoring results to bolster collaboration. Several prerequisites that enabled the successful HIV program transition in Rwanda were identified, including understanding the political context of integration and decentralization, ownership through national coordination, participation and partnership, equity, efficiency, accountability, and developing HIV delivery systems that simultaneously strengthened the entire health system.
Transition of donor-funded programs to country management is an important step on the development pathway and should be built into any program at the very beginning for more efficiency. To offer life-saving services to their people in a sustainable way, governments should strategize with their partners to achieve program transition of HIV delivery and beyond. Countries should seek more program management responsibility and request—as needed—specialized external technical support that helps to assure access to care, high quality, and accountability for the populations in need.
Zdroje
1. Goosby E, Von Zinkernagel D, Holmes C, Haroz D, Walsh T. Raising the Bar: PEPFAR and New Paradigms for Global Health. J Acquir Immune Defic Syndrome. 2012 Aug 15;60 Suppl 3:S158–62. doi: 10.1097/QAI.0b013e31825d057c
2. Bennett S, Singh S, Ozawa S, Tran N, Kang JS. Sustainability of donor programs: evaluating and informing the transition of a large HIV prevention program in India to local ownership. Global Health Action 2011, 4 : 7360 – doi: 10.3402/gha.v4i0.7360
3. Bossert TJ. Can they get along without us? Sustainability of donor-supported health projects in Central America and Africa. Soc Sci Med. 1990;30 : 1015–23. 2336568
4. Vermund S, Sidat M, Weil LF, Tique JA, Moon TD, Ciampa PJ. Transitioning HIV care and treatment programs in southern Africa to full local management. AIDS. 2012 June 19; 26(10): 1303–1310. doi: 10.1097/QAD.0b013e3283552185 22706012
5. Palen J, El-Sadr W, Phoya A, Imtiaz R, Einterz R, Quain E, Blandford J, Bouey P, Lion A. PEPFAR, health system strengthening, and promoting sustainability and country ownership. J Acquir Immune Defic Syndr. 2012 Aug 15; 60 Suppl 3:S113–9. doi: 10.1097/QAI.0b013e31825d28d7 22797732
6. Lo S, Horton R. AIDS and global health: the path to sustainable development. Lancet. 2015 Jul 11;386(9989):106–8. Epub 2015 Jun 24. 26117721.
7. Sgaier SK, Ramakrishnan A, Dhingra N et al. How The Avahan HIV Prevention Program Transitioned From The Gates Foundation. Health Affairs, 32, no.7 (2013):1265–1273
8. Ministry of Finance Rwanda Vision 2020. 2012. http://www.minecofin.gov.rw/fileadmin/templates/documents/NDPR/Vision_2020_.pdf
9. Bank World. Long-term payoffs from funding the fight against HIV/AIDS in Rwanda. 2012. http://www.worldbank.org/en/news/feature/2012/07/22/long-term-payoffs-from-funding-the-fight-against-hivaids-in-rwanda
10. Rapports d’activites de la commission Nationale de Lutte Contre le SIDA. 2003. http://repositories.lib.utexas.edu/bitstream/handle/2152/5009/4106.pdf?Sequence=1
11. PEPFAR. The Operational Plans of the U.S. President's Emergency Plan for AIDS Relief (2004–2013). 2013. http://www.pepfar.gov/about/c19388.htm
12. The Global Fund to Fight AIDS, Tuberculosis, and Malaria. Grant portfolio to Rwanda. Accessed 2016. http://www.theglobalfund.org/en/portfolio/country/results/?loc=RWA
13. Goosby E, Dybul M, Fauci AS, Fu J, Walsh T, Needle R, Bouey P. The United States President’s Emergency Plan for AIDS Relief: a story of partnerships and smart investments to turn the tide of the global AIDS pandemic. J Acquir Immune Defic Syndr. 2012 Aug 15;60 Suppl 3:S51–6. doi: 10.1097/QAI.0b013e31825ca721 22797740
14. UNAIDS. “Three Ones” key principles: Coordination of National Responses to HIV/AIDS: Guiding principles for national authorities and their partners. Conference Paper 1, Washington Consultation 25.04.04. unaids.org.ua/files/three-ones_keyprinciples_en.pdf
15. The World Bank—PRMPS, Combating corruption in the public sector Success stories. March 2013. http://sna.gov.it/fileadmin/files/workshop_seminari/Selection-of-case-studies.pdf
16. The Office of the Inspector General, The Global Fund to Fight AIDS, Tuberculosis and Malaria; Audit Report on the Global Fund Grants to Rwanda. Audit Report No.: GF-OIG-10-003 Issue Date: 11 March 2011. http://www.theglobalfund.org/documents/oig/OIG_RwandaCountryAudit2011_Report_en/
17. Rwanda CORDAID, Performance Based Funding in Rwanda, a comparative study. April 2007. http://www.multicountrypbfnetwork.org/Field_study.pdf
18. El-Sadr WM, Abrams EJ. Scale-up of HIV care and treatment: can it transform healthcare services in resource-limited settings? AIDS. 2007 Oct;21 Suppl 5:S65–70. doi: 10.1097/01.aids.0000298105.79484.62 18090271
19. Binagwaho A, Scott KW. Improving the World’s Health Through the Post-2015 Development Agenda: Perspectives from Rwanda. Int J Health Policy Manag 2015;4 : 203–5. doi: 10.15171/ijhpm.2015.46 25844381
20. Farmer PE, Nutt CT, Wagner CM, et al. Reduced premature mortality in Rwanda: lessons from success. BMJ 2013;346:f65. doi: 10.1136/bmj.f65 23335479
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2016 Číslo 8- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Metabolit živočišné stravy produkovaný střevní mikroflórou zvyšuje riziko závažných kardiovaskulárních příhod
-
Všetky články tohto čísla
- Dementia across the Lifespan and around the Globe—Pathophysiology, Prevention, Treatment, and Societal Impact: A Call for Papers
- Progress and Challenges in Scaling Up Laboratory Monitoring of HIV Treatment
- Facility-Based Delivery during the Ebola Virus Disease Epidemic in Rural Liberia: Analysis from a Cross-Sectional, Population-Based Household Survey
- Availability and Use of HIV Monitoring and Early Infant Diagnosis Technologies in WHO Member States in 2011–2013: Analysis of Annual Surveys at the Facility Level
- Duration of Adulthood Overweight, Obesity, and Cancer Risk in the Women’s Health Initiative: A Longitudinal Study from the United States
- Improving Clinical Risk Stratification at Diagnosis in Primary Prostate Cancer: A Prognostic Modelling Study
- Genetically Predicted Body Mass Index and Breast Cancer Risk: Mendelian Randomization Analyses of Data from 145,000 Women of European Descent
- Social Dancing and Incidence of Falls in Older Adults: A Cluster Randomised Controlled Trial
- Genetic and Environmental Risk for Chronic Pain and the Contribution of Risk Variants for Major Depressive Disorder: A Family-Based Mixed-Model Analysis
- Long-Term Outcomes Associated with Traumatic Brain Injury in Childhood and Adolescence: A Nationwide Swedish Cohort Study of a Wide Range of Medical and Social Outcomes
- On Risk Estimation versus Risk Stratification in Early Prostate Cancer
- Make Data Sharing Routine to Prepare for Public Health Emergencies
- Assessment of Adverse Events in Protocols, Clinical Study Reports, and Published Papers of Trials of Orlistat: A Document Analysis
- Concussions and Repercussions
- South Asia as a Reservoir for the Global Spread of Ciprofloxacin-Resistant : A Cross-Sectional Study
- Building from the HIV Response toward Universal Health Coverage
- Transitioning to Country Ownership of HIV Programs in Rwanda
- Accelerating the Uptake and Timing of Antiretroviral Therapy Initiation in Sub-Saharan Africa: An Operations Research Agenda
- Glycemic Control and the Risk of Tuberculosis: A Cohort Study
- Adjuvant Trastuzumab in HER2-Positive Early Breast Cancer by Age and Hormone Receptor Status: A Cost-Utility Analysis
- Uptake of Home-Based HIV Testing, Linkage to Care, and Community Attitudes about ART in Rural KwaZulu-Natal, South Africa: Descriptive Results from the First Phase of the ANRS 12249 TasP Cluster-Randomised Trial
- An Audit and Feedback Intervention for Reducing Antibiotic Prescribing in General Dental Practice: The RAPiD Cluster Randomised Controlled Trial
- Multidrug-Resistant Tuberculosis Treatment in North Korea: Is Scale-Up Possible?
- Associations between Mental Health and Ebola-Related Health Behaviors: A Regionally Representative Cross-sectional Survey in Post-conflict Sierra Leone
- Pancreatic Cancer Surgical Resection Margins: Molecular Assessment by Mass Spectrometry Imaging
- Integrated Delivery of Antiretroviral Treatment and Pre-exposure Prophylaxis to HIV-1–Serodiscordant Couples: A Prospective Implementation Study in Kenya and Uganda
- Measuring Burden of Unhealthy Behaviours Using a Multivariable Predictive Approach: Life Expectancy Lost in Canada Attributable to Smoking, Alcohol, Physical Inactivity, and Diet
- Comparison of Outcomes before and after Ohio's Law Mandating Use of the FDA-Approved Protocol for Medication Abortion: A Retrospective Cohort Study
- Core Outcomes for Colorectal Cancer Surgery: A Consensus Study
- Adverse Renal, Endocrine, Hepatic, and Metabolic Events during Maintenance Mood Stabilizer Treatment for Bipolar Disorder: A Population-Based Cohort Study
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Glycemic Control and the Risk of Tuberculosis: A Cohort Study
- Transitioning to Country Ownership of HIV Programs in Rwanda
- Dementia across the Lifespan and around the Globe—Pathophysiology, Prevention, Treatment, and Societal Impact: A Call for Papers
- Social Dancing and Incidence of Falls in Older Adults: A Cluster Randomised Controlled Trial
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



