-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Elevated Mutagenesis Does Not Explain the Increased Frequency of Antibiotic Resistant Mutants in Starved Aging Colonies
The frequency of mutants resistant to the antibiotic rifampicin has been shown to increase in aging (starved), compared to young colonies of Eschierchia coli. These increases in resistance frequency occur in the absence of any antibiotic exposure, and similar increases have also been observed in response to additional growth limiting conditions. Understanding the causes of such increases in the frequency of resistance is important for understanding the dynamics of antibiotic resistance emergence and spread. Increased frequency of rifampicin resistant mutants in aging colonies is cited widely as evidence of stress-induced mutagenesis (SIM), a mechanism thought to allow bacteria to increase mutation rates upon exposure to growth-limiting stresses. At the same time it has been demonstrated that some rifampicin resistant mutants are relatively fitter in aging compared to young colonies, indicating that natural selection may also contribute to increased frequency of rifampicin resistance in aging colonies. Here, we demonstrate that the frequency of mutants resistant to both rifampicin and an additional antibiotic (nalidixic-acid) significantly increases in aging compared to young colonies of a lab strain of Escherichia coli. We then use whole genome sequencing to demonstrate conclusively that SIM cannot explain the observed magnitude of increased frequency of resistance to these two antibiotics. We further demonstrate that, as was previously shown for rifampicin resistance mutations, mutations conferring nalidixic acid resistance can also increase fitness in aging compared to young colonies. Our results show that increases in the frequency of antibiotic resistant mutants in aging colonies cannot be seen as evidence of SIM. Furthermore, they demonstrate that natural selection likely contributes to increases in the frequency of certain antibiotic resistance mutations, even when no selection is exerted due to the presence of antibiotics.
Published in the journal: Elevated Mutagenesis Does Not Explain the Increased Frequency of Antibiotic Resistant Mutants in Starved Aging Colonies. PLoS Genet 9(11): e32767. doi:10.1371/journal.pgen.1003968
Category: Research Article
doi: https://doi.org/10.1371/journal.pgen.1003968Summary
The frequency of mutants resistant to the antibiotic rifampicin has been shown to increase in aging (starved), compared to young colonies of Eschierchia coli. These increases in resistance frequency occur in the absence of any antibiotic exposure, and similar increases have also been observed in response to additional growth limiting conditions. Understanding the causes of such increases in the frequency of resistance is important for understanding the dynamics of antibiotic resistance emergence and spread. Increased frequency of rifampicin resistant mutants in aging colonies is cited widely as evidence of stress-induced mutagenesis (SIM), a mechanism thought to allow bacteria to increase mutation rates upon exposure to growth-limiting stresses. At the same time it has been demonstrated that some rifampicin resistant mutants are relatively fitter in aging compared to young colonies, indicating that natural selection may also contribute to increased frequency of rifampicin resistance in aging colonies. Here, we demonstrate that the frequency of mutants resistant to both rifampicin and an additional antibiotic (nalidixic-acid) significantly increases in aging compared to young colonies of a lab strain of Escherichia coli. We then use whole genome sequencing to demonstrate conclusively that SIM cannot explain the observed magnitude of increased frequency of resistance to these two antibiotics. We further demonstrate that, as was previously shown for rifampicin resistance mutations, mutations conferring nalidixic acid resistance can also increase fitness in aging compared to young colonies. Our results show that increases in the frequency of antibiotic resistant mutants in aging colonies cannot be seen as evidence of SIM. Furthermore, they demonstrate that natural selection likely contributes to increases in the frequency of certain antibiotic resistance mutations, even when no selection is exerted due to the presence of antibiotics.
Introduction
Antibiotics target proteins involved in key cellular functions such as protein synthesis, RNA transcription, DNA replication, and cell wall biosynthesis (reviewed in [1], [2]). Most mutations that confer resistance to antibiotics affect these functions as well, and as a result reduce the fitness of exponentially growing bacteria [1]. Early in the study of resistance to antibiotics it was thought that since most resistance mutations appear to incur a fitness cost, resistance could be eradicated by limiting antibiotic usage. This optimistic view has more recently been demonstrated to be problematic [1]. For one, it turns out that in many cases deleterious effects of resistance mutations can be compensated for by additional mutations. Such compensatory mutations allow bacteria to maintain resistance over time [1]. Here we focus on a second, more neglected, reason for why it is possible for resistance mutations to persist and spread. A number of studies have demonstrated that, even in the absence of antibiotic treatment, mutants resistant to antibiotics tend to increase in frequency in response to various growth limiting conditions [3]–[6]. Such increases in resistance frequency may not only allow for the persistence and spread of resistance, but may also explain the emergence of resistance prior to bacteria ever encountering a given antibiotic. Understanding why such increases in resistance frequency occur is thus crucial.
Bjedov et al. [3] examined the frequencies with which aging (starved) and young (non-starved) colonies of Escherichia coli develop resistance to the antibiotic rifampicin (when no rifampicin is present in their growth media). They analyzed hundreds of different E. coli isolates, demonstrating that when starved through prolonged incubation on agar plates, an increase is observed in the frequency of rifampicin-resistant mutants. The extent of this increase varied greatly between different strains, and correlated with the environment from which the different strains were extracted. Bjedov et al. interpreted the observed increases in the frequency of resistant mutants as evidence for stress-induced mutagenesis (SIM), a dedicated mechanism by which bacteria are thought to increase mutation rates upon exposure to growth limiting conditions [3].
In a later paper (published in 2008) Wrande et al., who also observed an increase in the frequency of rifampicin resistant mutants in aging colonies, showed that some rifampicin resistance mutations provide a growth advantage in starved colonies [6]. Thus, the observed increase in the frequency of rifampicin resistant mutants may also be explained by natural selection favoring certain resistance mutations, conferring a growth advantage, rather than by increased mutagenesis.
Mutations conferring resistance to rifampicin generally occur in the RNA polymerase beta subunit gene, rpoB. Wrande et al. argued that the adaptive resistance mutations that arise under starvation cause rpoB to interact with the stationary phase sigma factor, rpoS, and induce the expression of genes that facilitate growth under starvation [6]. This allows the mutated bacteria to become “cheaters” that can grow while the other starved bacteria are put under growth arrest. While this theory may explain why an increase in the frequency of mutants resistant to rifampicin is observed in starved colonies, it cannot explain why Bjedov et al. observed an increased frequency of resistance to additional antibiotics, to which resistance is conferred by mutations occurring in other genes [3]. Although, it must be noted that the increases in the frequency of resistance that Bjedov et al. observed, for antibiotics other than rifampicin, were of a substantially lower magnitude than found for rifampicin.
Although the Wrande et al. results demonstrated that increased frequency of resistance to rifampicin in aging colonies can be explained by a mechanism different than SIM, the experiments of Bjedov et al. are still cited extensively as evidence of SIM occurring in natural bacterial populations (for example see [7]–[15], all published since 2012).
Increased mutagenesis resulting from stress may increase the frequency of resistance to antibiotics, through a mechanism different from SIM. Kohanski et al. demonstrated that growth in the presence of sub-lethal concentrations of bactericidal antibiotics leads to increases in the minimum inhibitory concentration (MIC) for a range of antibiotics [4]. Kohanski et al. suggested that these increases in resistance correlate with increases in the production of reactive oxygen species (ROS) that are thought to increase mutagenesis [4]. The mechanism suggested by Kohanski et al. to increase mutagenesis is different than SIM in that here mutagenesis would be increased through the action of an external mutagenic factor. Additionally, while SIM predicts that only a small sub-population of cells will increase mutation rate following exposure to a growth limiting stress [16], [17], the model under which external factors drive increases in resistance may suggest that the entire population will be affected and increase mutation rates.
Here we repeat the Bjedov et al. and Wrande et al. experiments on a lab strain of E. coli to show that the frequency of mutants resistant to two different antibiotics (rifampicin and nalidixic-acid) increases under starvation. We then use whole-genome sequencing to conclusively demonstrate that increased frequency of resistance to both antibiotics cannot be explained by SIM or increased mutagenesis across the entire starved population.
Results
Increased frequency of resistance to both rifampicin and nalidixic-acid in response to starvation
We repeated the starvation experiments carried out by Bjedov et al. and Wrande et al. [3], [6] on the fully sequenced Escherichia coli lab strain K12 MG1655. Briefly, experiments were started by spotting 300–600 cells from an overnight culture, on filters placed on Luria Broth (LB) plates. By starting experiments with so few cells we reduce the probability of having resistant cells within our cultures to begin with. Cells were then either starved or not. In order to grow bacteria without starvation we incubated the LB plates for a single day. To starve cells, we incubated the plates for an additional seven days. Scoring of resistance frequencies in the non-starved or starved populations was carried out through live counts of cells on normal LB plates and on plates containing either rifampicin or nalidixic acid. For each of the two antibiotics we conducted five independent experiments in which we quantified resistance frequency for 15 non-starved and 15 starved filters.
Cell growth was minimal within aging colonies. The average cell number increased only 1.25 fold from the first day following inoculation (1.6×108 cells) and seven days later (2×108 cells). At the same time, we found statistically significant increases in resistance frequency under starvation to both rifampicin (P = 0.0005, n = 15 according to a one-tailed, unpaired Mann-Whitney test), and nalidixic acid (P = 0.0003, n = 15). The average frequency of resistance to rifampicin increased ∼25-fold, from 2.6×10−8 in the non-starved bacteria to 6.6×10−7 in the starved bacteria. The average frequency of resistance to nalidixic acid increased 179-fold, from 2.9×10−10 in non-starved bacteria to 5.2×10−8 in starved bacteria.
Formulating expectations under a model in which increased frequency of antibiotic resistance in aging colonies results from stress-induced mutagenesis
We next used whole genome sequencing to examine whether the increases we observed in the frequency of resistance to rifampicin and nalidixic acid may be explained by increased mutagenesis due to starvation. To examine this, we must first formulate our expectations under a scenario in which increased mutagenesis indeed explains increased frequency of resistance.
Stress induced increases in mutagenesis may occur either in response to external mutagenic factors that may increase due to stress, or due to an intrinsic mechanism that allows bacteria to actively increase mutagenesis in response to stress. As an intrinsic mechanism, stress induced mutagenesis (SIM), has been studied extensively, using both plasmid and chromosomal “artificial” systems [8], [16], [18], [19]. Under the dominant model of SIM, only a small sub-population of bacteria, referred to as the HMS (hyper-mutable cell subpopulation) increases mutation rate substantially during SIM, while the majority of cells maintain a normal mutation rate [16], [17]. This HMS has been estimated to include 0.006–0.0006 of stressed cells [16], [20], [21].
Under the model of SIM where increased mutagenesis is limited to an HMS:
Where fstarved is the average mutation frequency across the entire starved population, p is the proportion of cells belonging to the HMS, fHMS is the mutation frequency within the HMS, and fnormal, is the mutation frequency within cells that do not belong to the HMS (which is the same as the mutation frequency in non-starved cells).Current estimates of “normal” mutation rates in E. coli, extracted from mutation accumulation experiments, followed by whole genome sequencing, are ∼0.001 mutations per genome per generation [22]. During our experiments the number of cells grew from ∼300 to on average approximately 2×108. These numbers can be used to conservatively estimate that ∼20 generations have passed during our experiments (conservatively, because this does not account for any possible cell death that occurred during the experiment). Thus, we can estimate that fnormal = 20×0.001 = 0.02. For SIM to explain the observed 25-fold increase in the frequency of resistance to rifampicin, fstarved would have to be 25-fold higher than fnormal. Therefore fstarved = 0.02×25 = 0.5.
From equation (1) and these values of fnormal and fstarved, we can see that:
Thus, if p = 0.006 (as previously estimated [20]), we would expect each HMS genome to acquire fHMS = ∼80 mutations. If the HMS drives the 25-fold increased frequency of resistance to rifampicin, we would expect that 24 of every 25 resistant genomes emerging under starvation will be members of the HMS. Thus, if SIM mediated by a small HMS explains the 25-fold increase in the frequency of rifampicin resistance we observe, we would expect 24 of 25 of rifampicin resistant genomes accumulating under starvation to accumulate on average ∼80 mutations during our experiment. Similarly, to explain the 179-fold increase in the frequency of resistance we observe to nalidixic acid, we would expect 178 of 179 nalidixic acid resistant genomes, emerging under starvation, to acquire, on average, almost 600 mutations each.Increased frequency of resistance to antibiotics under starvation cannot be explained by stress-induced mutagenesis of a small hyper-mutating cell subpopulation
To examine whether the genomes of the strains that have acquired resistance to rifampicin and nalidxic acid under starvation indeed accumulated such high numbers of mutations, we sequenced the full genomes of 15 starved rifampicin resistant isolates and 15 starved nalidixic acid resistant isolates. These resistant isolates were taken from two starvation experiments, in which a significant increase in resistance frequency was found to both antibiotics under starvation (106-fold increase in the frequency of resistance to rifampicin, P = 0.004, and a 145-fold increase in the frequency of resistance to nalidxic acid, P = 0.01).
As we mentioned above, for SIM mediated by an HMS to explain a 25-fold increase in rifampicin resistance frequency, 24 of 25 starved rifampicin resistant isolates would have to be members of the HMS. It can easily be calculated that when sequencing 15 starved rifampicin resistant isolates we can be significantly confident that we will sequence at least 13 members of the HMS under this scenario (P<0.05 under the binomial distribution). For SIM mediated by an HMS to explain a 179-fold increase in nalidixic acid resistance frequency 178 of 179 starved nalidixic acid resistant isolates would have to be members of the HMS. Under this scenario we can be significantly confident that we will sequence at least 14 members of the HMS when sequencing 15 starved nalidixic acid resistant isolates.
The 15 rifampicin resistant isolates we sequenced evolved on six independent filters, while the 15 nalidixic acid resistant isolates evolved on five independent filters. Rifampicin resistant mutants presented several different morphologies, when grown on the selective plates. For example, some mutants grew faster to form larger colonies, while others grew slower, forming smaller colonies. In order to maximize the likelihood that we would be sequencing independently evolving mutants, in the cases where we sequenced more than one rifampicin resistant mutant from the same filter, we chose mutants with different morphologies. We were unable to do the same for nalidixic acid resistant mutants, because all of them presented similar morphologies.
DNA was extracted from each mutant. We then pooled the DNA from the 15 nalidixic acid resistant strains, and separately pooled the DNA from the 15 rifampicin resistant strains. Pooling was done so as to obtain equal concentrations of DNA from each mutant (see Materials and Methods). The two pools were sequenced on the Illumina HiSeq2000 platform. We sequenced single-end 50 bp reads. The coverage obtained for each pool is given in Supplementary Table S1, and in Supplementary figures S1, S2. As is evident from Supplementary Table S1, high coverage was obtained so that each strain within a pool had on average between 59 and 67X coverage.
We analyzed the sequencing data we obtained using permissive thresholds, so as not to miss any possible mutations (see Materials and Methods). We then confirmed candidate mutations through PCR amplification and Sanger re-sequencing from each of the individual genomes. Even though our thresholds for the identification of putative mutations were very permissive, only four unique mutations were found in the 15 nalidixic acid resistant genomes, and only seven unique mutations in the 15 rifampicin resistant genomes. Mutations causing resistance to nalidixic acid occur mostly in the DNA gyrase gene gyrA [23]. Three of the mutations found in the nalidixic acid resistant strains were non-synonymous mutations to gyrA, that were previously characterized as causing resistance to this antibiotic [23] (Table 1). All Seven mutations occurring in the rifampicin resistant genomes were non-synonymous. All of them occurred in the rpoB gene (Table 2). Mutations causing resistance to rifampicin are known to occur within rpoB [24], [25].
Tab. 1. Mutations identified in 15 starved, nalidixic acid resistant isolates. 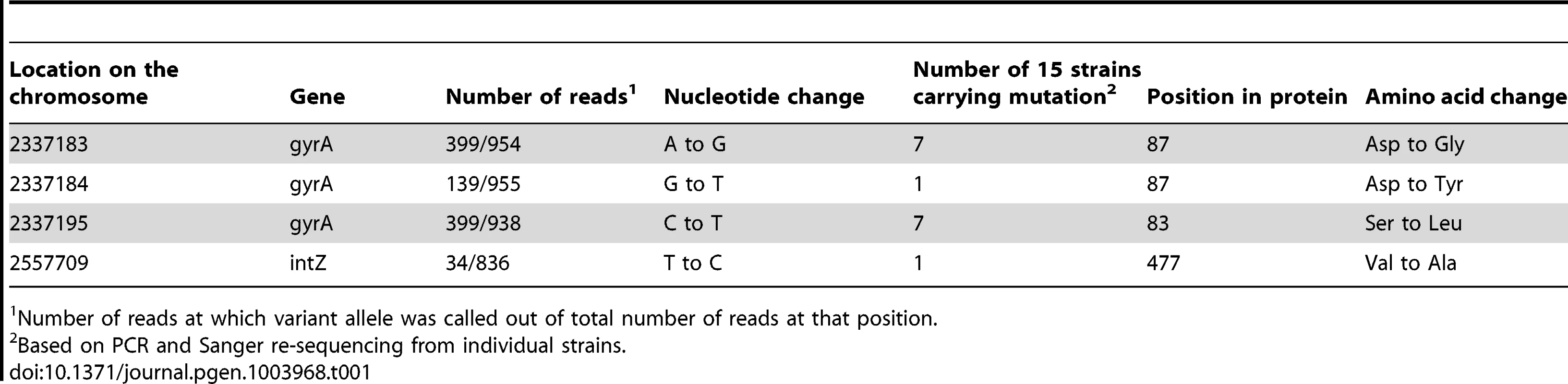
Number of reads at which variant allele was called out of total number of reads at that position. Tab. 2. Mutations identified in 15 starved, rifampicin resistant isolates. 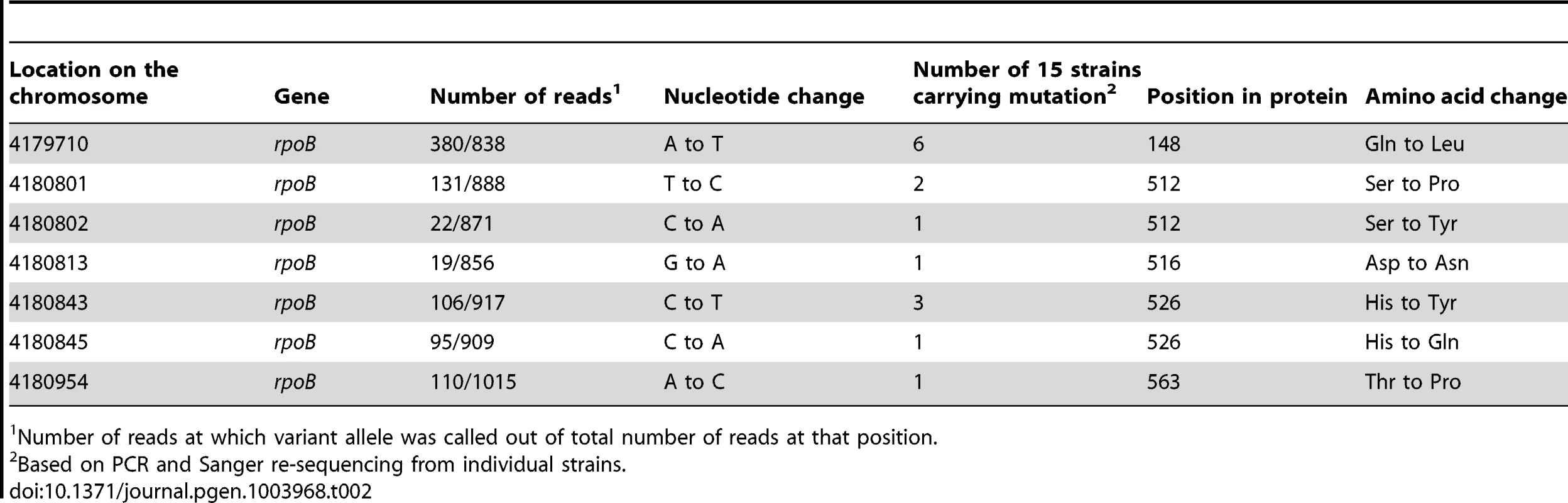
Number of reads at which variant allele was called out of total number of reads at that position. We amplified and re-sequenced the regions containing the mutations we identified through whole-genome sequencing, separately for each genome within each of the two pools. This allowed us to confirm that each resistant genome acquired only a single resistance mutation that conferred resistance in that genome. Specifically, each nalidixic resistant genome contained one, and only one of the three gyrA mutations we identified (Table 1), and each rifampicin resistant genome contained one, and only one of the seven mutations we identified in rpoB (Table 2). We could therefore confirm that mutations we identified through whole genome sequencing explained resistance in all 30 strains, and that no resistance mutations were missed. This provides a good internal control demonstrating that we likely did not miss any additional mutations that may have occurred in these strains.
To summarize, each rifampicin resistant genome accumulated only a single, resistance mutation and no other mutations occurred in the 15 rifampicin resistant genomes. 14 of the 15 nalidixic acid resistant genomes also acquired only the single resistance mutation, while one of the 15 acquired a single additional mutation, for a total of two mutations. These numbers are incredibly smaller than what would be expected if a small HMS (of the size previously estimated) drives the observed 25-fold increase in the frequency of resistance to rifampicin, and/or the 179-fold observed increase in the frequency of resistance to nalidixic acid (∼80 mutations per genome for at least 13 of the 15 rifampicin resistant genomes, almost 600 per genome for at least 14 of the 15 nalidixic acid resistant genomes, see above).
Even if the proportion of cells belonging to the HMS is 10% of all cells (meaning almost 20-fold higher than highest available estimates), we would still expect each HMS cell to acquire on average 4.82 mutations during our experiments, in order to explain a 25-fold increase in the frequency of resistance to rifampicin (see equation (2) above). Simulations indicate that under such a scenario we would expect to observe in 15 HMS cells (with 95% confidence, see Materials and Methods and Figure 1), between 56 and 89 mutations. Even if only 13 of the 15 rifampicin resistant genomes we sequenced belonged to the HMS (see above), we would still expect (with 95% confidence) to observe between 48 and 79 mutations, according to our simulations. This is again, a much higher number than we actually observed in the 15 rifampicin resistant genomes we sequenced (where each genome acquired only the one resistance conferring mutation). An even higher number of mutations would have to occur in HMS cells in order to explain the 179-fold increase in resistance frequency, we observed, to nalidixic acid.
Fig. 1. Actual number of observed mutations in rifampicin resistant and nalidixic acid resistant starved genomes is much smaller than expected within HMS (hypermutating cell subpopulation) cells. 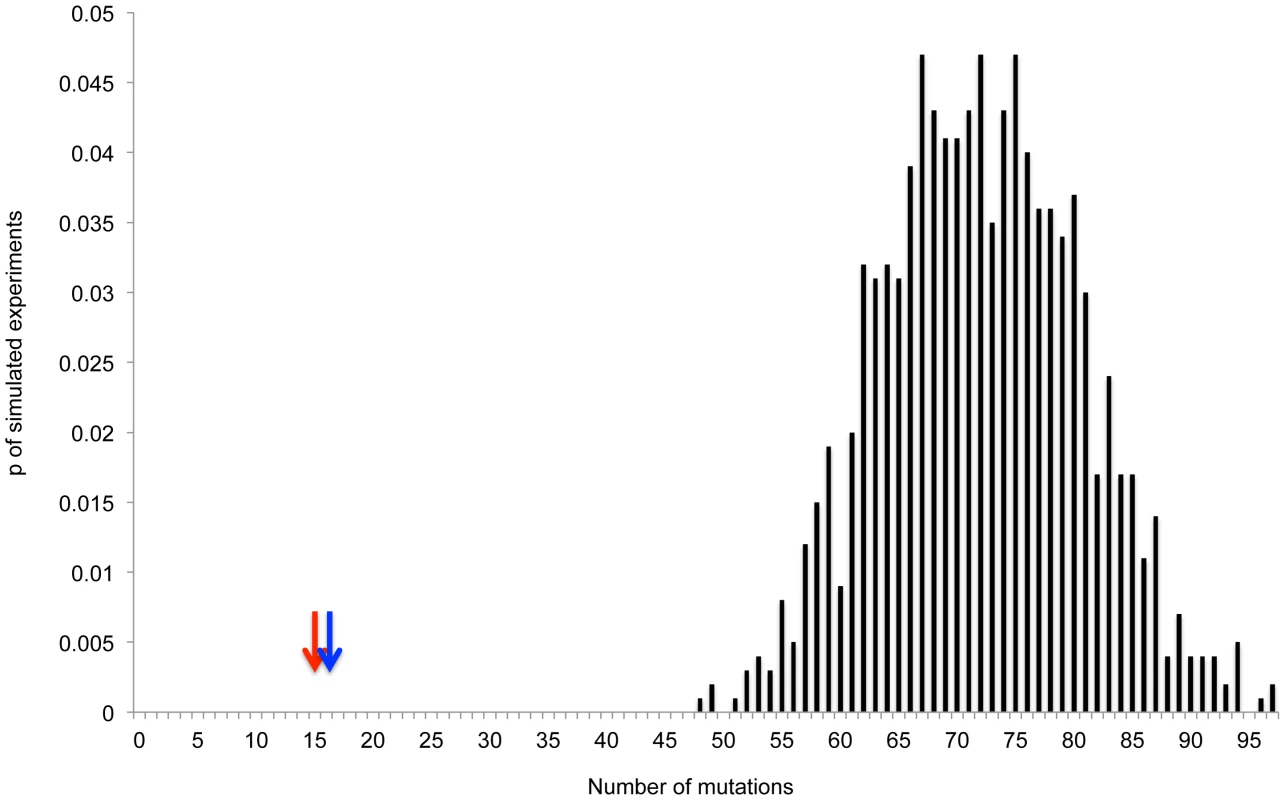
Drawn is the distribution of the numbers of mutations we would expect to find in 1000 simulated experiments in which we sequence 15 HMS genomes, and each HMS genome is expected to accumulate on average 4.82 mutations (calculated based on a 25-fold increase in mutagenesis across the entire starved population and an HMS size of 10%). The arrows represent the numbers of mutations we actually observed in 15 fully sequenced starved rifampicin (Red), or nalidixic acid (Blue) resistant genomes. In the case of nalidixic acid, we observed that mutants arising on the same filter always carried the exact same mutations. This suggests that the nalidixic acid resistant mutants we sequenced that evolved on the same filter did not evolve independently but rather clonally expanded following a single mutation event. This in itself provides some evidence that increases in the frequency of resistance to nalidixic acid are not due to increase mutagenesis [6]. At the same time, this means we did not actually sequence 15 independently arising nalidixic acid resistant strains, but rather only five independently arising strains (the 15 strains sequenced came from five independent filters). This fact however should not significantly affect the results, because under current estimates of the size of the HMS, we would expect to observe almost 600 mutations per HMS strain, to explain a 179-fold increase in the frequency of resistance to nalidixic acid. Even if the size of the HMS is 10% of all cells, we would still expect to observe approximately 36 mutations on average within each nalidixic acid independently evolved resistant genome we sequenced. We however found only one or two mutations per sequenced genome. In the case of rifampicin resistance, when sequencing mutants from the same filter, we selected mutants presenting different morphologies. For this reason, the mutants we sequenced that arose on the same filter evolved independently and did not share the same mutations.
To conclude, our results demonstrate conclusively that increases in resistance frequencies to both rifampicin and nalidixic acid cannot be explained by the resistant genomes belonging to a small HMS. Thus, the model of SIM under which the HMS contributes most of the increase in mutagenesis, cannot explain the observed increases in the frequency of antibiotic resistance, demonstrated to occur in response to starvation.
Elevated frequency of antibiotic resistance can also not be explained by an overall increase in mutagenesis across the entire starved bacterial population
It is also possible that increased mutagenesis occurs not only in a small HMS, but rather across the entire starved population. This, for instance, may be expected if increased mutagenesis acts due to an external mutagenic factor that increases as a result of starvation. To test whether increased mutagenesis across the entire starved population may explain the observed increase in the frequency of antibiotic resistance, we sequenced the full genomes of 15 non-starved, and 15 starved isolates that were not tested for resistance to antibiotics. These isolates represent the general population of non-starved and starved bacteria respectively. As with the sequencing of the rifampicin and nalidixic acid resistant genomes, sequencing was carried out on pools of 15 genomes. Pools were sequenced to extremely high coverage (Supplementary Table S1 and Supplementary Figures S3 and S4) on the Illumina HiSeq2000 platform. Identified mutations were confirmed through PCR and Sanger re-sequencing.
Only three mutations were found to occur in the 15 starved isolates (Table 3). Each of the three mutations occurred in only a single genome. One of the starved genomes acquired two of the mutations found, another one acquired one mutation, and the remaining 13 starved genomes acquired no mutations. Only one mutation was found to occur in the 15 non-starved isolates (Table 3). This mutation appeared in a single genome, meaning 14 of the non-starved genomes acquired no mutations, while one of these genomes acquired a single mutation.
Tab. 3. Mutations identified in 15 non-starved and 15 starved isolates, untested for resistance. 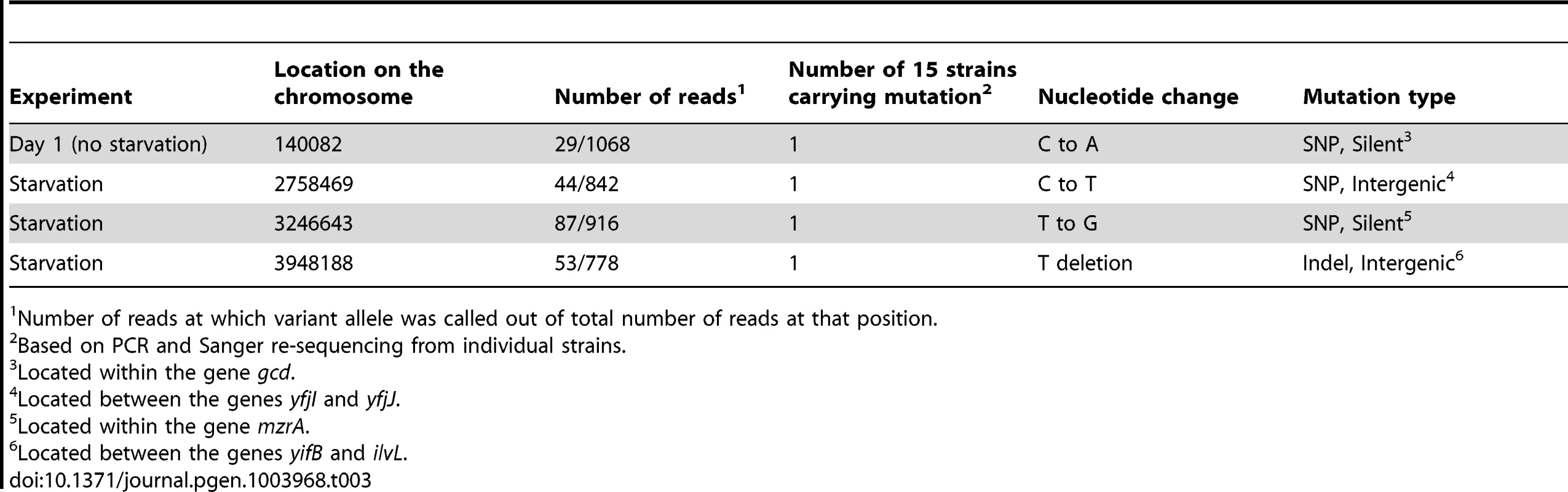
Number of reads at which variant allele was called out of total number of reads at that position. As described above, current estimates of “normal” mutation rates in E. coli are ∼0.001 mutations per genome per generation [22], and we conservatively estimate that ∼20 generations have passed during our experiments. It is therefore possible to estimate that the average non-starved genome would accumulate ∼0.001×20 = 0.02 mutations during our experiment. In order for increases in mutagenesis occurring across the entire population, to explain a 25-fold increase in the frequency of rifampicin resistance, mutation rates would have to increase on average 25-fold. Thus, the average starved genome would accumulate 0.02×25 = 0.5 mutations. Simulations (Figure 2A, Materials and Methods) indicate that under such a regimen the probability of observing three or less mutations in 15 starved genomes is quite small, albeit not sufficiently small to demonstrate statistical significance (∼0.06). When one considers the 179-fold increase in mutation rate that would need to occur in order to explain what we observed when it came to resistance to nalidixic acid, the results are even more striking. If such an increase in mutation had occurred we would expect the average stressed genome to accumulate 0.02×179 = 3.58 mutations. When sequencing 15 starved strains our simulations indicate we would expect (with 95% confidence) to observe between 40 and 67 mutations (Figure 2B). Under such a regimen one would never expect to observe a number of mutations as low as we actually observed.
Fig. 2. Actual number of observed mutations in 15 starved genomes is smaller than expected under a model of increased mutagenesis affecting the entire starved population. 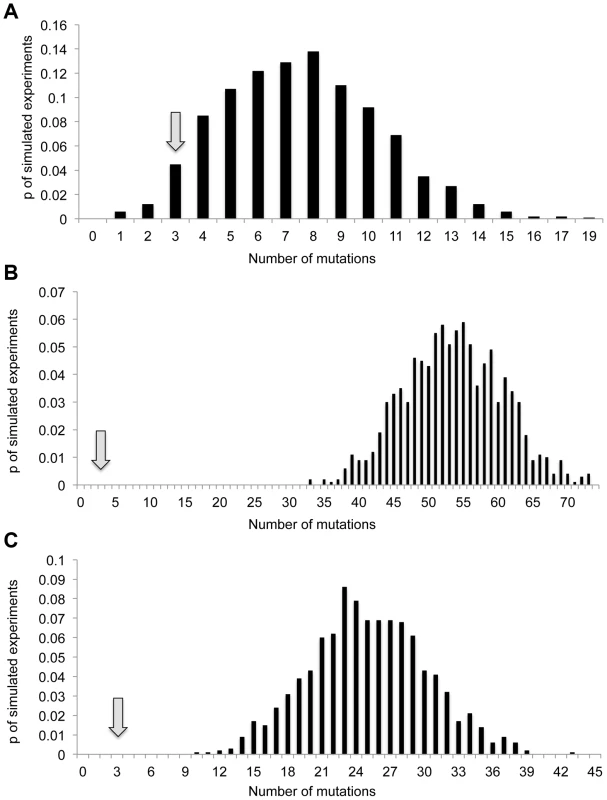
Drawn are the distributions of the numbers of mutations observed in simulations of 1000 experiments, in which 15 genomes are sequenced, under three different average mutation frequencies: (A) 0.5 mutations per genome (25–fold higher than expected under current estimates of mutation rates, assuming 20 generations). (B) 3.58 mutation per genome (179–fold higher than expected under current estimates of mutation rates, assuming 20 generations). (C) 25 mutations per 15 genomes (25-fold higher than the number of mutations we observed in the 15 non-starved genomes we sequenced. Arrows represent actual number of mutations observed in the 15 starved genomes we sequenced. There is a second, less conservative way to estimate the expected number of mutations under an on average 25-fold or 179-fold increase in mutagenesis, affecting the entire bacterial population. One can estimate the expected number of mutations in the absence of starvation based on the actual number of mutations we observed in the 15 non-starved genomes we sequenced and multiply this number by 25 or 179. Since we observed a single mutation in the 15 non-starved genomes, we would expect to observe, in the 15 starved genomes, 25 mutations under a 25-fold increase in mutagenesis and 179 mutations, under a 179-fold increase in mutagenesis. According to simulations, under an average mutation frequency of 25 mutations per 15 genomes, we would expect to observe with 95% confidence between 15 and 35 mutations in the 15 starved genomes we sequenced (Figure 2C). In none of the simulated experiments do we observe less than 10 mutations. The fact that we observed only three mutations within the sequenced starved genomes therefore indicates that there was not a sufficient increase in mutagenesis to explain the observed increases in the frequency of resistance to either rifampicin or nalidixic acid.
To summarize, given that we observed only three mutations in the 15 starved genomes we sequenced, increased mutagenesis across the entire population is very unlikely to explain the observed 25-fold increase in the frequency of resistance to rifampicin, and definitely cannot explain the observed 179-fold increase in the frequency of resistance to nalidixic acid. We can therefore conclude that the patterns of increased resistance frequency we observe in our starvation experiments cannot be explained by increases in mutagenesis affecting the entire starved bacterial population.
Relative fitness advantage of resistant mutants in aging compared to young colonies
We demonstrate conclusively that elevated mutagenesis cannot explain the increases observed in the frequency of resistant mutants. This raises the intriguing possibility that natural selection may contribute to the observed increases in the frequency of mutants resistant to both rifampicin and nalidixic acid. Wrande et al. have demonstrated using competition experiments that several rifampicin resistant mutants have a relative growth advantage in aging compared to young colonies [6]. We conducted similar competition experiments to examine whether the three different nalidixic acid resistance mutations, we found had emerged in the aging colonies, also confer a relative fitness benefit in aging compared to young colonies. Briefly, we inserted different antibiotic cassettes (Kanamycin (Kan) and Chloramphenicol (Chl)) into the genomes of the nalidixic acid resistant mutants and of the wildtype E. coli. We generated cells of all mutants and of the wildtype containing both these cassettes so that we could account for fitness effects of the cassettes themselves. It is important to note that having sequenced the full genomes of the different resistant mutants, we know they carry no other mutations beyond the resistance mutations we aim to test. As with the original starvation experiments we inoculated 102 to 103 cells of wildtype E. coli (unmarked) on filters. Following one day of growth we inoculated ∼300 marked wildtype cells and ∼300 marked mutant cells on the day old colonies of wildtype unmarked E. coli. We then estimated the mutant to wildtype ratio at the day of inoculation (day zero), after the first day and after seven days.
To examine whether different nalidixic acid resistance mutations carry relative fitness benefits in aging colonies, we compared the mutant to wildtype ratios of the different mutants at day zero, to these ratios one day and seven days following inoculation. We found that for the amino acid position 87 D to G mutation there is a significant increase in the mutant to wildtype ratio at day seven compared to days one and zero (P = 0.0002 and 0.0063 respectively, according to a one-tailed, unpaired Mann-Whitney test). The mutant to wildtype ratio was on average 1.05, 0.9 and 2.46, on days zero, one and seven, respectively. Interestingly, at day one the ratio of mutant to wildtype is significantly lower than on day zero (P = 0.0023). These results indicate that this mutant has a relative fitness disadvantage compared to wildtype in young colonies, but that the same mutation confers a growth advantage within aging colonies. This growth advantage is strong enough to allow this mutant to outcompete the wildtype in aging colonies even though it earlier on had a growth disadvantage when the colonies were younger. We can therefore deduce that the position 87 D to G nalidixic acid resistant mutant has a relative fitness advantage in aging compared to young colonies. The fitness advantage of this mutant may contribute to the increase in the frequency of nalidixic acid resistant mutants in aging colonies.
The second mutant at the same position (position 87 D to Y) has a very different effect on fitness. Similarly to the D to G mutant, the D to Y mutant appears to be less fit than the wildtype in young colonies (as the ratio of mutant to wildtype is strongly significantly lower at day one compared to day zero (average mutant to wildtype ratio of 1.19 and 0.55 at days zero and one respectively, P<<0.0001)). However, for the D to Y mutant this fitness cost of the mutant becomes even more pronounced in aging colonies where the mutant to wildtype ratio decreases even further (mutant to wildtype ratio = 0.3, P = 0.031). For the third mutant (amino acid position 83 S to L) the ratio of mutant to wildtype increases between days 0 and 1 and day7 (from 1.02 and 1.08 at days 0 and 1 to 2.6 at day 7). However, this difference is not statistically significant (P>>0.05, for both comparisons, according to a one-tailed, unpaired Mann-Whitney test).
To examine whether the Kan and Chl markers in themselves affected the results of our competition experiment, we carried out competition experiments, similar to the ones described above, using two wildtype strains, each containing one of the two resistance cassettes. We found that the ratios of wildtype cells carrying the Kan marker to wildtype cells carrying the Chl marker remained consistently very close to one in day0 day1 and day7 (1.06, 1.08 and 0.99, respectively).
Discussion
In our starvation experiments, the frequency of resistance to rifampicin increased on average 25-fold, and the frequency of resistance to nalidixic acid increased on average 179-fold. Our sequencing and simulation results clearly demonstrate that SIM cannot explain these observed increases in resistance frequency. This is in sharp contrast to the widespread assumption that increased frequency of resistance to antibiotics under starvation is the direct result of SIM, and that such increased resistance frequency can be seen as evidence that SIM occurs in natural bacterial populations (for example see [7]–[15], all published since 2012).
Wrande et al. have demonstrated that some rifampicin resistance mutations to the RNA polymerase beta subunit gene, rpoB confer a growth advantage under starvation [6]. Rodríguez-Verdugo et al. further demonstrated that some rifampicin resistance mutations also increase fitness when bacteria are exposed to heat shock in a glucose limited media [26]. Wrande et al. hypothesized that the mutant RpoB proteins interact with the stationary phase sigma factor RpoS to induce the expression of genes that control stationary phase. This in turn makes the resistant mutants “cheaters” of stationary phase that can continue growing while wildtype cells enter growth arrest [6]. We add to these results by demonstrating that at least one mutation conferring resistance to nalidixic acid also provides a similar growth advantage in aging compared to young colonies. Interestingly, a recent paper by Webber et al. [27] demonstrated that the position 87 D to G mutation, that we show is fitter in aging colonies leads to the induction of the expression of several stress responsive sigma factors, including rpoS. Therefore, it appears that some mutations conferring resistance to both antibiotics may increase fitness in aging colonies through interactions with the bacterial stress response. A similar adaptive effect was also demonstrated for a mutation conferring resistance to a third antibiotic. Paulander et al. [28] showed that a specific mutation to the rpsL gene, conferring resistance to streptomycin confers a growth advantage when salmonella are grown in media with poorer carbon sources. Paulander et al. further showed that the mutant failed to induce expression of RpoS and that, fitting with this the mutant was deficient in its ability to cope with severe heat shock [28]. The fact that resistance mutations to three different antibiotics targeting three different genes have been shown to increase fitness, independently of antibiotic exposure, under certain growth-limiting conditions is intriguing. Even more intriguing is the possibility that for all three antibiotics the causes of such increased fitness of resistant mutants is related to modulation of the bacterial stress response via interaction of some kind with rpoS.
Our results demonstrate that there is at least one nalidixic acid resistance mutation conferring a growth advantage in aging colonies and the results of Wrande et al. demonstrate the same for several rifampicin resistance mutations. We cannot however provide conclusive evidence that this positive selection is sufficient to explain the observed fold increase in the frequency of resistance to both antibiotics.
There are other factors that may, in addition to natural selection, also contribute to increased frequency of resistant mutants in aging colonies. According to Luria and Delbruck the number of resistant bacteria increases on two accounts: first, new mutations occur with each generation and second, there is growth of resistant bacteria from previous mutations [29]. It is therefore easy to deduce that some increase in the frequency of resistant mutants is expected even in the absence of selection in favor of mutations and/or increased mutagenesis. However, for this to lead to the dramatic increases in resistance frequency observed in the aging colonies, many generations would have to occur between day one of the experiment and seven days later. Yet, we observed only a 1.25 fold increase in cell numbers between the two time points, indicating that most cell growth occurs prior to day one and there is very little cell growth in aging colonies following the first day. It is possible that there is more cell growth within starved colonies then observed through live counts of cells, if within starved colonies there is much more cell death than within younger colonies. However, Wrande et al. [6] conducted Live/Dead microscopy analyses and found no evidence of increased cell death in aging colonies.
Another factor that may contribute to increases in the frequency of resistant mutants may be the occurrence of resistance mutations early on in some experiments. In such cases the frequency of resistant mutants at the end of the experiment may be much higher then in other experiments. This might lead to an over estimation of differences in the frequencies with which resistant mutants emerge between aging and young colonies [6], [29].
It is also theoretically possible that the observed increase in frequency of resistant mutants does not actually happen on the starved filters. Rather, it is possible that when exposed to the antibiotics on the selective plates, starved cells produce higher frequencies of persisters that are phenotypically resistant. If these persisters replicate at all on the selective plates, resistant mutants could then be generated and strongly selected for, due to the presence of antibiotics on the selective plates. We do however have strong evidence that this scenario does not in fact explain the increased frequency of resistance, and that the resistant mutants we sequenced have indeed been generated on the filters, rather than on the selective plates. We found that in the case of nalidixic acid resistance, all resistant mutants extracted from the same filter carried the exact same resistance mutation. This would not be expected if resistant mutants were not generated on the filters. We could not demonstrate a similar trend for rifampicin resistant mutants, because we purposefully selected mutants presenting different morphologies when sequencing mutants from the same filter. However Wrande et al. showed that rifampicin mutants arising on the same section of a starved colony tended to have the same exact mutations [6].
To conclude, we demonstrate that the increased frequency of mutants resistant to both rifampicin and nalidixic acid in aging colonies cannot be explained by increased mutagenesis. Our results, together with the results of Wrande et al. [6] further show that some resistance mutations to both antibiotics provide a growth advantage within aging colonies. These results are intriguing as they suggest that there is selection in favor of certain resistance mutations even in the absence of antibiotic treatment. Such antibiotic-independent selection in favor of certain resistance mutations may greatly affect the dynamics of antibiotic resistance emergence and spread within natural bacterial populations.
Materials and Methods
Starvation experiments
MG1655 E. coli K12 laboratory strain was used in this study. The strain was ordered from the ATCC. Starvation experiments were conducted as previously described in [3]. Briefly, 300–600 cells from an overnight culture were plated on a 0.45 um nitrocellulose filter (Whatman, GmbH). Three filters were placed on each Luria Broth (LB) agar plate (10 g/l tryptone, 5 g/l Yeast extract, 5 g/l NaCl, 15 g/l agar). Bacteria were then incubated at 37°C, for either a single day, or an extra seven days (for a total of eight days). Following incubation each bacterial spot was re-suspended in 1 ml of LB and incubated for 1 hour at 37°C. In order to determine the number of viable bacterial cells, appropriate dilutions were spread on LB agar plates. In order to determine the number of antibiotic resistant cells, 100 ul from the undiluted bacterial suspension was taken and plated in duplicates on LB agar plates supplemented with antibiotic nalidixic acid (40 µg/ml) or rifampicin (100 µg/ml).
DNA extractions and pooling of samples
Following growth on filters, starved and non-starved bacteria were grown on LB plates and on LB plates supplemented with either rifampicin or nalidixic acid (see above). For sequencing, we selected individual colonies from these LB or antibiotic supplemented LB plates. Each colony was grown over night at 37°C on liquid LB or on LB supplemented with the appropriate antibiotics. The bacterial DNA was then extracted using the DNeasy Blood & Tissue Kit (QIAGEN, GmbH Hamburg) according to the manufacturer's instructions. The DNA concentration of each sample was quantified using NanoDrop (Thermo scientific, Wilmington USA). Following quantification, 1 ug from each DNA sample was taken and pooled together with 14 other samples (of the same kind). In such a manner four pools were generated for sequencing, each containing DNA from 15 isolates: (1) day-7 samples that are nalidixic acid resistant; (2) Day-7 samples that are rifampicin resistant; (3) day-1 samples untested for resistance; (4) day-7 samples untested for resistance.
Analyses of sequencing data
Sequencing reads were separated based on their barcodes, and a single fastq file was generated for each of the four pooled libraries. Reads within each fastq file were aligned to the fully sequenced E. coli K12 MG1655 genome, using the bwa software package [30], and SAM files were generated. SAM files were then converted into BAM files, sorted and indexed using the samtools software package [31]. The samtools program mpileup was then used to generate a list of putative variable sites within each pool. The –E option was used. This option helps sensitivity, and may harm specificity. In other words it reduces the probability that we will miss mutations that have occurred, but increases the probability of identifying putative mutations that are not really there. Mpileup was made to print all putative variable sites, irrespective of their reliability (so as to not miss any possible mutations). An external Perl script was written to go through the putative variable sites identified by the mpileup program. The program extracted variable sites appearing at a frequency of higher than 10 reads. This is an extremely permissive threshold given that the mean coverage per genome within each pool ranges between 53 and 75X (Supplementary Table S1).
It is known that there are systematic sequencing errors in which one sees a variable site in many reads but biased to a single strand (i.e. where there is a site that has a X nucleotide in the reference sequence and a Y nucleotide in n different sequencing reads, but these n reads almost always map to a single strand (either the + or the − strand)) [32]. To avoid such errors we removed from our analyses any variable sites that had less than 5 reads map to either the + or the − strand of the reference sequence. To call indels we used the Varscan v2.3.4 mpileup2indel program [33]. We, again, used very permissive thresholds, demanding only that an indel appear in at least 10 reads, and in at least 0.02 of the total reads. The strand-filter option was used to remove from consideration indels appearing only on a single strand (as mentioned above a known systematic error of Illumina sequencing).
Variable sites were removed from consideration if they appeared in more than one of the pools. Such variable sites will most often represent systematic sequencing errors. In rarer cases they may represent mutations that have fixed between the ATCC E. coli K-12 MG1655 strain we used, and the MG1655 sequenced reference strain, or alleles that were polymorphic within the MG1655 stock we received from the ATCC. They may also in rare cases represent mutations that occurred when we grew bacteria prior to the initiation of our experiments (after all, we sequenced the results of two separate experiments that were each started after growing bacteria over night). Either way, variable sites appearing in more than one experiment do not represent mutations that occurred during our experiments, since they are not unique to any one experiment.
Confirmation of mutations through PCR And Sanger re-sequencing
Variable sites (mutations) that passed the above-described, extremely lax thresholds were confirmed through PCR and Sanger re-sequencing. The primers used are given in Supplementary Table S2. Confirmed mutations are summarized in Tables 1–3.
Mutation frequency simulations
To examine whether the number of mutations we observed in a pool of x genomes, could be explained by a certain expected mean mutation frequency f, we carried out simulations of 1000 in-silico experiments. Since mutation is a Poisson process [29], we assumed that the number of mutations we will observe for each genome in each experiment is Poisson distributed around the mean frequency f. To simulate an experiment, we therefore drew and summed up x numbers that are Poisson distributed around f. Drawing of numbers was done using the R package's rpois function. For each simulated experiment we get a number of mutations we would observe in x genomes in that experiment. The distributions of these numbers from 1000 simulated experiments represent what we would expect to observe in 1000 random experiments, given a certain number of sequenced genomes and a certain mean mutation frequency. A 95% confidence interval was calculated by removing the 0.025 lowest and highest values of these distributions, and thus maintaining the values we would expect to observe in 0.95 of experiments.
Competition experiments
From the 15 sequenced nalidixic acid resistant bacteria, we selected three that each carried one of the three unique resistance mutations we identified (Table 1). Since these genomes were sequenced, we know they contain no additional mutations. We performed linear transformation of antibiotic resistance cassettes (Chloramphenicol or Kanamycin) into chromosomal region 642520–642820 of wildtype E. coli MG1655 and of the three different mutants (the primers used are given in Supplementary Table S2). Linear transformation was carried out as was described by [34]. For each mutant and the wildtype, we generated strains carrying each one of the two cassettes. The drug resistance cassettes were kindly provided us by Prof. John Roth. Competition experiments were then performed as was previously described in [6]. Briefly, about 300–600 unmarked wildtype cells were spotted on a nitrocellulose filter membrane. On the following day (which we mark as day0) a mixture of 300–600 wild type cells (marked with either chloramphenicol or kanamycin) and 300–600 nalidixic acid resistant mutant cells (marked with either kanamycin or chloramphenicol) were spotted on top of the day old unmarked colony. The exact ratio of marked wildtype to marked mutant cells inoculated onto the day old filter was estimated through live counts (day0). We then measured the ratio of mutant to wildtype after one additional day (day1), and after seven additional days (day7). The measurement of these ratios was done by scraping the mixture spots, placing them in liquid LB and allowing them to recover for 1 hr at 37°C. Then 100 ul from the suspension were plated on LB chloramphenicol and on LB kanamycin plates and viable cells were counted the following day. In order to control for possible effects of the antibiotic cassettes themselves on fitness, we conducted similar competition experiments between chloramphenicol marked and kanamycin marked wildtype cells.
Supporting Information
Zdroje
1. AnderssonDI, HughesD (2010) Antibiotic resistance and its cost: is it possible to reverse resistance? Nat Rev Microbiol 8 : 260–271.
2. KohanskiMA, DwyerDJ, CollinsJJ (2010) How antibiotics kill bacteria: from targets to networks. Nat Rev Microbiol 8 : 423–435.
3. BjedovI, TenaillonO, GerardB, SouzaV, DenamurE, et al. (2003) Stress-induced mutagenesis in bacteria. Science 300 : 1404–1409.
4. KohanskiMA, DePristoMA, CollinsJJ (2010) Sublethal antibiotic treatment leads to multidrug resistance via radical-induced mutagenesis. Mol Cell 37 : 311–320.
5. McMahonMA, XuJ, MooreJE, BlairIS, McDowellDA (2007) Environmental stress and antibiotic resistance in food-related pathogens. Appl Environ Microbiol 73 : 211–217.
6. WrandeM, RothJR, HughesD (2008) Accumulation of mutants in “aging” bacterial colonies is due to growth under selection, not stress-induced mutagenesis. Proc Natl Acad Sci U S A 105 : 11863–11868.
7. MartincorenaI, LuscombeNM (2013) Non-random mutation: The evolution of targeted hypermutation and hypomutation. Bioessays 35 : 123–130.
8. RosenbergSM, SheeC, FrischRL, HastingsPJ (2012) Stress-induced mutation via DNA breaks in Escherichia coli: a molecular mechanism with implications for evolution and medicine. Bioessays 34 : 885–892.
9. RyallB, EydallinG, FerenciT (2012) Culture history and population heterogeneity as determinants of bacterial adaptation: the adaptomics of a single environmental transition. Microbiol Mol Biol Rev 76 : 597–625.
10. ObolskiU, HadanyL (2012) Implications of stress-induced genetic variation for minimizing multidrug resistance in bacteria. BMC Med 10 : 89.
11. BogumilD, DaganT (2012) Cumulative impact of chaperone-mediated folding on genome evolution. Biochemistry 51 : 9941–9953.
12. FeherT, BogosB, MehiO, FeketeG, CsorgoB, et al. (2012) Competition between transposable elements and mutator genes in bacteria. Mol Biol Evol 29 : 3153–3159.
13. Sanchez-AlberolaN, CampoyS, BarbeJ, ErillI (2012) Analysis of the SOS response of Vibrio and other bacteria with multiple chromosomes. BMC Genomics 13 : 58.
14. BuergerS, SpoeringA, GavrishE, LeslinC, LingL, et al. (2012) Microbial scout hypothesis, stochastic exit from dormancy, and the nature of slow growers. Appl Environ Microbiol 78 : 3221–3228.
15. MacleanRC, Torres-BarceloC, MoxonR (2013) Evaluating evolutionary models of stress-induced mutagenesis in bacteria. Nat Rev Genet 14 : 221–227.
16. RoscheWA, FosterPL (1999) The role of transient hypermutators in adaptive mutation in Escherichia coli. Proc Natl Acad Sci U S A 96 : 6862–6867.
17. GonzalezC, HadanyL, PonderRG, PriceM, HastingsPJ, et al. (2008) Mutability and importance of a hypermutable cell subpopulation that produces stress-induced mutants in Escherichia coli. PLoS Genet 4: e1000208.
18. GalhardoRS, HastingsPJ, RosenbergSM (2007) Mutation as a stress response and the regulation of evolvability. Crit Rev Biochem Mol Biol 42 : 399–435.
19. Al MamunAA, LombardoMJ, SheeC, LisewskiAM, GonzalezC, et al. (2012) Identity and function of a large gene network underlying mutagenic repair of DNA breaks. Science 338 : 1344–1348.
20. GalhardoRS, DoR, YamadaM, FriedbergEC, HastingsPJ, et al. (2009) DinB upregulation is the sole role of the SOS response in stress-induced mutagenesis in Escherichia coli. Genetics 182 : 55–68.
21. FosterPL (2007) Stress-induced mutagenesis in bacteria. Crit Rev Biochem Mol Biol 42 : 373–397.
22. LeeH, PopodiE, TangH, FosterPL (2012) Rate and molecular spectrum of spontaneous mutations in the bacterium Escherichia coli as determined by whole-genome sequencing. Proc Natl Acad Sci U S A 109: E2774–2783.
23. SaenzY, ZarazagaM, BrinasL, Ruiz-LarreaF, TorresC (2003) Mutations in gyrA and parC genes in nalidixic acid-resistant Escherichia coli strains from food products, humans and animals. J Antimicrob Chemother 51 : 1001–1005.
24. JinDJ, CashelM, FriedmanDI, NakamuraY, WalterWA, et al. (1988) Effects of rifampicin resistant rpoB mutations on antitermination and interaction with nusA in Escherichia coli. J Mol Biol 204 : 247–261.
25. JinDJ, GrossCA (1988) Mapping and sequencing of mutations in the Escherichia coli rpoB gene that lead to rifampicin resistance. J Mol Biol 202 : 45–58.
26. Rodriguez-VerdugoA, GautBS, TenaillonO (2013) Evolution of Escherichia coli rifampicin resistance in an antibiotic-free environment during thermal stress. BMC Evol Biol 13 : 50.
27. WebberMA, RicciV, WhiteheadR, PatelM, FookesM, et al. (2013) Clinically relevant mutant DNA gyrase alters supercoiling, changes the transcriptome, and confers multidrug resistance. MBio 4: e00273–13.
28. PaulanderW, Maisnier-PatinS, AnderssonDI (2009) The fitness cost of streptomycin resistance depends on rpsL mutation, carbon source and RpoS (sigmaS). Genetics 183 : 539–532SI, 539-546, 531SI-532SI.
29. LuriaSE, DelbruckM (1943) Mutations of Bacteria from Virus Sensitivity to Virus Resistance. Genetics 28 : 491–511.
30. LiH, DurbinR (2009) Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25 : 1754–1760.
31. LiH, HandsakerB, WysokerA, FennellT, RuanJ, et al. (2009) The Sequence Alignment/Map format and SAMtools. Bioinformatics 25 : 2078–2079.
32. MeachamF, BoffelliD, DhahbiJ, MartinDI, SingerM, et al. (2011) Identification and correction of systematic error in high-throughput sequence data. BMC Bioinformatics 12 : 451.
33. KoboldtDC, ZhangQ, LarsonDE, ShenD, McLellanMD, et al. (2012) VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res 22 : 568–576.
34. DatsenkoKA, WannerBL (2000) One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc Natl Acad Sci U S A 97 : 6640–6645.
Štítky
Genetika Reprodukčná medicína
Článek Ribosome Synthesis and MAPK Activity Modulate Ionizing Radiation-Induced Germ Cell Apoptosis inČlánek Fission Yeast Shelterin Regulates DNA Polymerases and Rad3 Kinase to Limit Telomere Extension
Článok vyšiel v časopisePLOS Genetics
Najčítanejšie tento týždeň
2013 Číslo 11- Gynekologové a odborníci na reprodukční medicínu se sejdou na prvním virtuálním summitu
- Je „freeze-all“ pro všechny? Odborníci na fertilitu diskutovali na virtuálním summitu
-
Všetky články tohto čísla
- Molecular Recognition by a Polymorphic Cell Surface Receptor Governs Cooperative Behaviors in Bacteria
- The Light Skin Allele of in South Asians and Europeans Shares Identity by Descent
- Ribosome Synthesis and MAPK Activity Modulate Ionizing Radiation-Induced Germ Cell Apoptosis in
- Retrotransposon Silencing During Embryogenesis: Cuts in LINE
- Roles of XRCC2, RAD51B and RAD51D in RAD51-Independent SSA Recombination
- Parallel Evolution of Chordate Regulatory Code for Development
- A Genetic Approach to the Recruitment of PRC2 at the Locus
- Deletion of the Murine Cytochrome P450 Locus by Fused BAC-Mediated Recombination Identifies a Role for in the Pulmonary Vascular Response to Hypoxia
- Elevated Mutagenesis Does Not Explain the Increased Frequency of Antibiotic Resistant Mutants in Starved Aging Colonies
- Deletion of an X-Inactivation Boundary Disrupts Adjacent Gene Silencing
- Interplay between Active Chromatin Marks and RNA-Directed DNA Methylation in
- Recombinogenic Conditions Influence Partner Choice in Spontaneous Mitotic Recombination
- Crosstalk between NSL Histone Acetyltransferase and MLL/SET Complexes: NSL Complex Functions in Promoting Histone H3K4 Di-Methylation Activity by MLL/SET Complexes
- A New Role for the GARP Complex in MicroRNA-Mediated Gene Regulation
- RNAi-Dependent and Independent Control of LINE1 Accumulation and Mobility in Mouse Embryonic Stem Cells
- Loss of DNMT1o Disrupts Imprinted X Chromosome Inactivation and Accentuates Placental Defects in Females
- Inhibition of the Smc5/6 Complex during Meiosis Perturbs Joint Molecule Formation and Resolution without Significantly Changing Crossover or Non-crossover Levels
- Disruption of Lipid Metabolism Genes Causes Tissue Overgrowth Associated with Altered Developmental Signaling
- Translation Initiation Factors eIF3 and HCR1 Control Translation Termination and Stop Codon Read-Through in Yeast Cells
- Recruitment of TREX to the Transcription Machinery by Its Direct Binding to the Phospho-CTD of RNA Polymerase II
- MYB97, MYB101 and MYB120 Function as Male Factors That Control Pollen Tube-Synergid Interaction in Fertilization
- Oct4 Is Required ∼E7.5 for Proliferation in the Primitive Streak
- Contrasted Patterns of Crossover and Non-crossover at Meiotic Recombination Hotspots
- Transposable Prophage Mu Is Organized as a Stable Chromosomal Domain of
- Ash1l Methylates Lys36 of Histone H3 Independently of Transcriptional Elongation to Counteract Polycomb Silencing
- Fine-Mapping the Genetic Association of the Major Histocompatibility Complex in Multiple Sclerosis: HLA and Non-HLA Effects
- Genomic Mechanisms Accounting for the Adaptation to Parasitism in Nematode-Trapping Fungi
- Decoding a Signature-Based Model of Transcription Cofactor Recruitment Dictated by Cardinal Cis-Regulatory Elements in Proximal Promoter Regions
- Removal of Misincorporated Ribonucleotides from Prokaryotic Genomes: An Unexpected Role for Nucleotide Excision Repair
- Fission Yeast Shelterin Regulates DNA Polymerases and Rad3 Kinase to Limit Telomere Extension
- Activin Signaling Targeted by Insulin/dFOXO Regulates Aging and Muscle Proteostasis in
- Activin-Like Kinase 2 Functions in Peri-implantation Uterine Signaling in Mice and Humans
- Demographic Divergence History of Pied Flycatcher and Collared Flycatcher Inferred from Whole-Genome Re-sequencing Data
- Recurrent Tissue-Specific mtDNA Mutations Are Common in Humans
- The Histone Variant His2Av is Required for Adult Stem Cell Maintenance in the Testis
- The Maternal-to-Zygotic Transition Targets Actin to Promote Robustness during Morphogenesis
- Reconstructing the Population Genetic History of the Caribbean
- and Are Required for Growth under Iron-Limiting Conditions
- Whole Genome, Whole Population Sequencing Reveals That Loss of Signaling Networks Is the Major Adaptive Strategy in a Constant Environment
- Neuron-Specific Feeding RNAi in and Its Use in a Screen for Essential Genes Required for GABA Neuron Function
- RNA∶DNA Hybrids Initiate Quasi-Palindrome-Associated Mutations in Highly Transcribed Yeast DNA
- Mouse BAZ1A (ACF1) Is Dispensable for Double-Strand Break Repair but Is Essential for Averting Improper Gene Expression during Spermatogenesis
- Genetic and Functional Studies Implicate Synaptic Overgrowth and Ring Gland cAMP/PKA Signaling Defects in the Neurofibromatosis-1 Growth Deficiency
- DUX4 Binding to Retroelements Creates Promoters That Are Active in FSHD Muscle and Testis
- Pathways-Driven Sparse Regression Identifies Pathways and Genes Associated with High-Density Lipoprotein Cholesterol in Two Asian Cohorts
- PLOS Genetics
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- and Are Required for Growth under Iron-Limiting Conditions
- Genetic and Functional Studies Implicate Synaptic Overgrowth and Ring Gland cAMP/PKA Signaling Defects in the Neurofibromatosis-1 Growth Deficiency
- The Light Skin Allele of in South Asians and Europeans Shares Identity by Descent
- RNA∶DNA Hybrids Initiate Quasi-Palindrome-Associated Mutations in Highly Transcribed Yeast DNA
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy





