-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Observational Evidence of For-Profit Delivery and Inferior Nursing Home Care: When Is There Enough Evidence for Policy Change?
Margaret McGregor and colleagues consider Bradford Hill’s framework for examining causation in observational research for the association between nursing home care quality and for-profit ownership.
Published in the journal: Observational Evidence of For-Profit Delivery and Inferior Nursing Home Care: When Is There Enough Evidence for Policy Change?. PLoS Med 13(4): e32767. doi:10.1371/journal.pmed.1001995
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.1001995Summary
Margaret McGregor and colleagues consider Bradford Hill’s framework for examining causation in observational research for the association between nursing home care quality and for-profit ownership.
Summary Points
Nursing home residents are a highly vulnerable population, and nursing home care quality has been a persistent focus of public concern.
There is considerable evidence from observational studies that public funding of care delivered in for-profit facilities is inferior to care delivered in public or nonprofit facilities.
The past decade has seen many industrialized countries increasing governmental payment for care of frail seniors in for-profit nursing homes, leading to questions about whether this leads to inferior care.
Many of Bradford Hill’s guidelines for causation can be found in published studies supporting a causal link between for-profit ownership and inferior care.
The precautionary principle should be applied when developing policy for this frail and vulnerable population.
Introduction
Nursing homes, also called residential long-term care facilities or aged care homes, are regulated institutions providing around-the-clock medical and social care to (mainly) older people who are unable to live independently due to physical and/or mental disability. Because of the vulnerability of this population and frequent media reports of scandals across many industrialized countries [1], nursing home care quality has been a persistent focus of public concern.
Inserted into the discourse on quality has been a trend in many countries to contract care to for-profit–owned facilities, and there has been considerable effort by researchers to understand the impact of for-profit ownership on care quality. Research into this area is not new [2]. O’Brien and colleagues asked the question in a 1983 review in which they included several United States studies going back to 1968 [3]. However, recent examples such as the 2011 failure of the largest United Kingdom private equity nursing home chain, Southern Cross [4], and a report in 2000 that the five largest US nursing home chains operated under bankruptcy protection [5], have brought this policy question to the forefront.
The issue has particular relevance at this time as jurisdictions are challenged to care for an increasing number of very frail people over the next two decades [6]. Even with policies to expand care at home, it is likely that many countries will require the construction of new nursing home beds [7].
In this paper, we evaluate the evidence for an association between for-profit ownership and inferior care, using Bradford Hill’s framework for examining causation in observational research. We further frame the issue in terms of the precautionary principle, asking, “At what point is it is time to shift policy direction based on the available evidence?”
Trends in Nursing Home Ownership and Care Delivery in Industrialized Countries
Nursing homes can be owned and operated by public (government or quasi-governmental), nonprofit, or for-profit entities, with differences among countries in financing, regulation, and mix of ownership. Box 1 describes a taxonomy of different ownership types. Regardless of the ownership and delivery of nursing home care, the majority of funding for nursing home care in industrialized countries comes from public sources [8].
Box 1. Taxonomy of Nursing Home Ownership
Public ownership: facilities owned by government or quasi-governmental bodies. Municipal governments, health regions, and Veterans Affairs would be examples of public and quasi-public owners.
Nonprofit ownership: nongovernmental ownership by religious or community groups or agencies, in which the facilities they operate are run as nonprofit societies. A nonprofit society or entity is constituted with the assumption that any revenue in excess of expenses will be used to benefit its clients.
For-profit facilities: owned and operated as businesses. Here it is assumed that revenue in excess of expenses can be directed to the owners—or, in the case of shareholder-owned companies, to shareholders. They include both small provider-owned facilities and large corporate chains whose headquarters are not necessarily in the province, or even the country, where they operate. The distinction between provider ownership and corporate ownership can be important: when facility owners are also care providers, it is fair to expect that—at least theoretically—their professional obligation balances the sometimes conflicting motivations of generating profit and providing good-quality care.
Table 1 summarizes trends in nursing home ownership across a range of years and countries. In the UK in 2012, 78% of residential care beds were in for-profit–owned facilities, a 10% increase from 2007 [9]. In Australia, roughly one-third of nursing home beds are owned by private for-profit companies [10]. In New Zealand, a survey of New Zealand Care Association members reported that approximately two-thirds of nursing homes were for-profit, a trend that was increasing [11]. In the US, more than two-thirds of beds are for-profit, with more than half owned by corporate chains [12,13].
Tab. 1. Percent of nursing home beds, by for-profit and nonprofit ownership 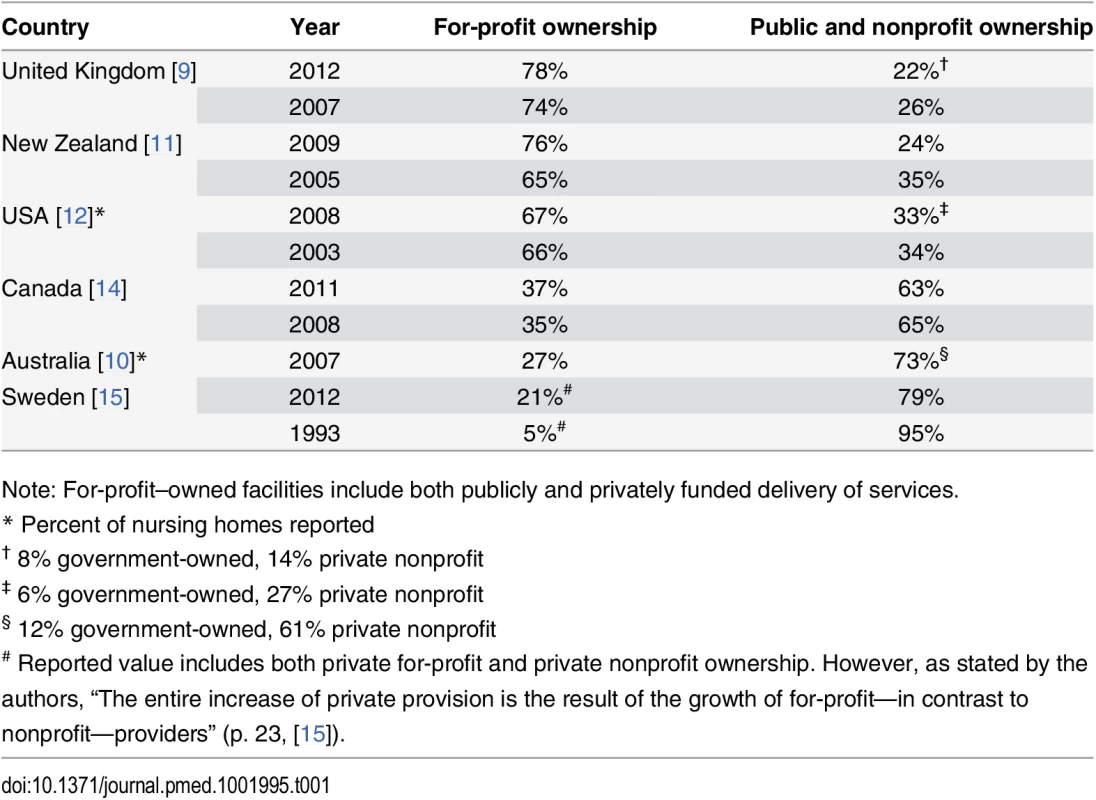
Note: For-profit–owned facilities include both publicly and privately funded delivery of services. The past decade has also seen the movement of private equity and other investor-owned firms into the nursing home sector, in both the US and other industrialized countries [4,13,16]. Some have termed this a “caretelization” of the nursing home industry, whereby large corporate providers have gained greater market share through the process of mergers, acquisitions, and takeovers [4].
Evaluating the Observational Evidence Using Bradford Hill’s Guidelines
There are challenges to measuring care quality (Box 2). Nonetheless, three systematic reviews have concluded that for-profit nursing homes had poorer care quality than nonprofit-owned homes [17–19]. A large meta-analysis found that two of four outcomes were significantly superior in nonprofit compared to for-profit homes [17]: more or higher quality staffing (ratio of effect 1.11, 95% confidence interval [CI]: 1.07 to 1.14), and lower pressure ulcer prevalence (0.91, 95% CI: 0.83 to 0.98). Non-significant results were found for the two other outcomes: fewer deficiencies in governmental regulatory assessments (0.90, 95% CI: 0.78 to 1.04) and lower physical restraint use (0.93, 95% CI: 0.82 to 1.05). The authors estimated that residents would receive 42,000 and 500,000 additional hours of nursing care per year, and have 600 and 7,000 fewer pressure ulcers in Canada and the US, respectively, if these services were provided solely by nonprofit facilities [17]. In 40 of the 82 studies reviewed, all statistically significant measures of quality favored nonprofit facilities, compared to only three studies in which all measures favored for-profit facilities [17].
Box 2. How Is Care Quality Measured in Nursing Homes?
Measurement of care quality in nursing homes is multidimensional, with numerous definitions, a vast range of indicators, and no gold standard for measurement [20,21]. Examples of different quality indicators include structural (such as staffing levels and training), process (such as inspection violations, continuity of care, prevalence of daily physical restraints, and indwelling catheters), and outcome indicators (such as prevalence of pressure sores, urinary tract infections, avoidable hospital admissions and dehydration) [20]. There is also growing recognition that, beyond staffing measures, there has been little progress in measuring resident - and family-reported experience of care [22,23], which is arguably one of the most meaningful measures in this population [23].
While no single indicator represents the overall quality of a nursing home, a disadvantage of using multiple quality indicators is that findings can be inconsistent [24]. A detection bias can also occur whereby rates of adverse outcomes may be higher in nursing homes or jurisdictions that actively “look for” problems [24]. Small numbers of events and small average facility size can limit the power of statistical analyses to find an effect [24]. This can lead to wide confidence intervals around estimates and conclusions that observed trends are not statistically significant [24]. Confounding can also result when comparing indicators between facilities, since patient case mix can vary between facilities [24]. Finally, many nursing homes are measured on self-reported indicators, leading to potential reporting bias for some indicators.
An editorial accompanying the above-described meta-analysis implied that the observational evidence is too weak for policy decisions, and that because of the impossibility of conducting randomized controlled trials of profit versus nonprofit status, causation cannot be proven [25]. This brings us to a theoretical debate about how we determine a link is causal when all we have, and all we are ever likely to have, is evidence from observational studies.
We use the Bradford Hill framework to assess whether there is sufficient evidence to suggest causation [26]: the presence of plausibility, temporality, experiment, dose-response, coherence, analogy, consistency, magnitude of effect, and specificity (Box 3):
Box 3. Bradford Hill’s Guidelines for Assessing Causation
It is usually accepted that high-quality randomized controlled trials (RCTs) are able to overcome bias and confounding and, therefore, top the evidence hierarchy to provide sufficient evidence to establish a causal link between exposure and outcome [27]. However, properly conducted RCTs in many areas are rare—trials can be underpowered, unsuccessfully blinded, and suffer from undetected biases [27]. Furthermore, not all research questions can be investigated using RCTs. In the case of nursing homes, it would be neither ethical nor feasible to randomly assign facility ownership or care delivery to for-profit versus public or nonprofit status. Thus, we rely on observational studies to evaluate the relationships between quality of care and ownership, in which we observe rather than assign exposures. Criticisms of observational studies, however, are that they are more prone to bias and confounding.
Some suggest that guidelines for causation can be a useful tool for assessing if there is sufficient evidence before concluding causation [27]. The British epidemiologist, Sir Austin Bradford Hill, developed guidelines to evaluate evidence for a causal effect [26]. These guidelines, first published in 1965, in part to address the link between tobacco and lung disease, provide a useful framework for assessing evidence for a causal effect. Specifically, Bradford Hill suggested that nine relevant factors should be considered before concluding causation [26]:
Plausibility: The cause-and-effect interpretation of an association should fit with the known facts of the natural history and biology of the disease.
Temporality: A necessary criterion for a causal association is that the exposure must precede the outcome.
Experiment: Causation is more likely if evidence is based on randomized experiments.
Biological gradient or dose-response: The likelihood of a causal association is increased if a dose-response curve can be demonstrated.
Coherence: A causal conclusion should not contradict present substantive knowledge.
Analogy: For analogous exposures and outcomes, an effect has already been shown.
Consistency: A relationship is observed repeatedly, prospectively and retrospectively, in different populations.
Strength of the association: Strong associations are more likely to be causal than weak associations.
Specificity: If an association is limited to specific groups with a particular environmental exposure or is greatly increased in these groups, then the case for a causal association is strengthened.
Plausibility
All nursing homes must balance their revenues and expenses in order to survive. For-profit organizations operate on the principle that profits or net income (revenue in excess of expenses) is directed to the owners, investors, or shareholders [28]. In nonprofit organizations and publicly owned facilities, net income is used to benefit clients [28].
O’Neill describes the trade-off between profit and quality: “If increasing quality raises costs more quickly than it does revenues, profits must fall as quality improves” [29]. In order to generate profits, for-profit homes tend to have lower costs and lower staff-to-patient ratios than nonprofit facilities [30]. Money diverted to shareholders and investors leaves less money to pay for staff, and in turn, having fewer or untrained staff is associated with lower quality [31–34].
The lower level of staffing with for-profit ownership [17,18] stands in contrast to the well-established association between higher levels of total nursing and registered nursing staff and better care outcomes [31–34]. Nurse staffing levels have a positive impact on both the process and the outcomes of nursing home care, such as reduced resident time in bed, improved feeding assistance, incontinence care, exercise and repositioning [33], fewer regulatory deficiencies [35], and lower rates of pressure ulcers [17]. Higher staffing levels are associated with lower staff turnover [36]—a pre-condition for good relational care, which in turn is associated with improved quality of life [23] (i.e., relational care embraces the entire relationship between caregiver and care recipient, encompassing the physical, social, emotional, and spiritual dimensions of human connection [37,38]). In a US study, the largest ten for-profit chains had lower registered nurse and total nurse staffing hours and a 41% higher number of serious deficiencies than government facilities, controlling for other factors [30].
A second plausible mechanism proposed for the “for-profit” effect of inferior outcomes is that for-profit facilities have a lower threshold for transferring acutely ill residents to acute care facilities [39–42]. This higher rate of use of acute services (emergency department visits and hospital admissions) among residents in for-profit facilities has been a consistent finding and is thought to be in part related to avoidance of the higher costs associated with caring for acutely ill residents [39–42]. Hospital admission for nursing home residents is considered a poor outcome because it puts these residents at risk of iatrogenic infections [43], falls, delirium, and decline in functional status and quality of life [44]. Furthermore, there is now some evidence that illnesses such as pneumonia can be equally well managed within the facility [45].
A third plausible mechanism for the association of nonprofit and/or public facilities with improved quality of care may be related to their ability to become charitable foundations. In many jurisdictions, this status provides tax breaks and makes them better positioned to mobilize volunteers and solicit donations for equipment [46].
In ideal market conditions, residents’ should be able to “exit” (leaving the facility) or use “voice” (complaining) [47]. However, the high degree of vulnerability of the nursing home population and the information asymmetry required for meaningful choice make these ineffective as counterbalances to behaviors that sacrifice quality [48,49].
Temporality
Temporality has been investigated in several studies by examining conversions between ownership types. Longitudinal observational research from the US [50] and Sweden [51] has found that nursing homes converting to for-profit ownership demonstrated a subsequent decline in some quality measures. Nursing homes converting from for-profit to nonprofit status generally exhibit improvement both before and after conversion [52]. A major challenge to such research is the potentially confounding effect of unmeasured differences in nursing homes that choose to convert [50] compared to those who do not.
Experiment
While it is unlikely that experimental evidence from randomized trials will ever be available to compare nursing home ownership and quality, two US studies [39,40] have recently used a method (instrumental variables analysis) that mimics randomization. This approach can estimate causal relationships when it is not possible to conduct a randomized trial.
The two studies examined a national cohort of newly admitted residents to short - [39] and long-stay facilities [40], including almost 14,000 US nursing homes. Data were drawn from national standardized clinical data (Minimum Data Set, MDS) linked to Medicare claims over an 18-month period between 2004 and 2005. Authors mimicked randomization of residents into more or less “exposure” to nonprofit homes by using “differential distance” to the nearest nonprofit nursing home relative to the nearest for-profit nursing home. Both studies found higher rates of hospital admissions and one study [39] demonstrated inferior outcomes for mobility, pain, and function measures among residents living in for-profit facilities compared to nonprofit facilities. The authors concluded that the observed effects were likely causal and could not be explained by unmeasured differences in case mix between facilities with different ownership structures.
Dose-Response Effect
A gradient effect between profit margins and US nursing home inspection violations has been reported [29]. O’Neill and colleagues examined 952 for-profit facilities in California to assess the relationship between profit and the number of total and serious deficiencies reported by regulatory inspectors. Authors divided facilities into four profit categories from the lowest to the highest profit group. After controlling for resident case mix and other facility and market characteristics, the authors found the highest profit group had significantly more total deficiencies than those in the second-highest profit group. They also found that facilities in the highest profit group had significantly more serious deficiencies than the three lower profit groups, suggesting an inverse gradient (dose-response) effect of profit on quality [29].
Coherence, Analogy, and Consistency
Parallel studies have found for-profit services in sectors other than residential long-term care to be of inferior quality, including hemodialysis centers [53] and Health Maintenance Organizations (HMOs) [54]. Outside of the health sector, studies looking at the daycare sector in Canada [55,56] have found a similar quality gap between for-profit and nonprofit ownership.
The majority of studies evaluating nursing home ownership and care quality have used US data [17], where the distinction is typically between private for-profit and nonprofit. Studies have also reported the association between for-profit status and inferior care when compared to either nonprofit or public models in other countries, including Canada [57–60], Israel [61], and Australia [62]. While most studies are from industrialized, high-income countries, we find no reason to expect that evidence from low - and middle-income countries would be different.
Strength of the Association
The differences reported in observational studies associated with for-profit status have generally not been large (with reported relative risks between 1 and 2) [17]. However, the magnitudes of effect are often small in studies of health care interventions, reflecting the implementation of interventions within complex systems [63].
Specificity
This term refers to the causative agent resulting in very specific effects. This criterion is more relevant to a biomedical (versus a health systems or policy) paradigm—for example, the assumption that mesothelioma, a very specific type of lung cancer, is only seen when an individual has been exposed to asbestos [64]. While the concept is of limited application in the health policy arena, the strongest empirical evidence exists for the association of for-profit status and lower staffing levels. Since the number of staff hired is also the most costly line item with the greatest likelihood of affecting profit, one might argue that there is some degree of specificity to the association.
Nursing Homes Are Complex Adaptive Systems and Context “Matters”
Nursing homes are complex adaptive systems [65], and health policy research, unlike biomedical research, is unlikely to discover one causal link to any system-level outcome. The association between for-profit ownership and inferior care is not a simple one.
In predominantly for-profit environments, some not-for-profit groups, despite their mandate, operate more as competitive market entities, with the focus often shifting towards increasing revenues at the expense of quality. Conversely, in jurisdictions dominated by the nonprofit or public sector, overall quality for the whole region is generally found to be better, including care delivered in for-profit nursing homes [66]. One interpretation is that the predominantly public sector raises the bar for all facilities, thus mitigating the effect of profit-making on quality. Such findings, rather than refuting the plausibility of the observed association, speak to various predisposing and mitigating contextual factors.
Additionally, where comparisons of quality have subdivided nonprofit ownership into governmental (publicly owned) and nonprofit groups, there is often a hierarchy of outcomes, whereby public models are superior to both for-profit and nonprofit models and for-profit models are inferior to public and nonprofit owned organizations [58,67,68].
When Is There Sufficient Evidence for Policy Change?
Bradford Hill did not prescribe these guidelines as rules that must be fulfilled before an association can be judged as causal, but as a way of examining if cause and effect is the reasonable inference [69]. In the current case, some of the Bradford Hill criteria are clearly met, while others are less clear.
At the very least, the precautionary principle should apply to this highly vulnerable nursing home population. The precautionary principle shifts the debate by calling for preventive action, even when there is uncertainty but credible evidence of potentially significant impacts. This shift in burden of proof is based on the obvious premise that harms to the public's health should be avoided and that society should not have to wait for conclusive evidence before acting to protect itself [70]. Taking a precautionary approach emphasizes our responsibility to ask, when do we know enough to act as if something is causal? [71]
What Are the Policy Challenges?
The policy response to the evidence on facility ownership clearly depends on jurisdictional context. In jurisdictions contemplating construction of new nursing home beds, policy makers need to support public and nonprofit facility ownership. Possible policy approaches include the sale of government savings bonds to raise public funds for capital construction [72], providing support to nonprofit societies with the necessary expertise for them to make competitive bids on requests for proposals, and valuing social capital and links with the community in the bidding process [7].
All jurisdictions should require public funding be earmarked and spent on mandated minimum direct care staffing levels consistent with the evidence, with no discretion for facilities to re-direct this money to other budgetary items (including profit generation). In countries where a majority of facilities are owned by large for-profit chains, proposed “downstream” policy approaches include improved financial transparency of how public resources are spent and the adoption of cost controls on administration [73]. Unfortunately, these approaches are costly to implement [74].
Decision-makers have a responsibility to ensure nursing home public policy is most consistent with the available evidence and least likely to cause harm. The majority of funding to operate and deliver care in nursing homes is derived from public, taxpayer-funded sources. When provided by the for-profit sector, the evidence suggests there is a greater likelihood of inferior care. It is time to re-align policy with evidence. Our seniors deserve better.
Supporting Information
Zdroje
1. Lloyd L, Banerjee A, Harrington C, Jacobsen F, Szebehely M. It’s A Scandal! Comparing the Causes and Consequence of Nursing Home Media Scandals in Five Countries. International Journal of Sociology and Social Policy 2014;34(1/2):2–18.
2. Institute of Medicine (US) Committee on Implications of For-Profit Enterprise in Health Care. Chapter 6: Quality of Care. Cover of For-Profit Enterprise in Health Care For-Profit Enterprise in Health Care. In: BH G, ed.: Washington (DC): National Academies Press (US), 1986.
3. O'Brien J, Saxberg BO, Smith HL. For-profit or not-for-profit nursing homes: does it matter? The Gerontologist 1983;23(4):341–8. 6352419
4. Scourfield P. Caretelization revisited and the lessons of Southern Cross. Critical Social Policy 2012;32 (1):137–48.
5. U.S. General Accounting Office. Nursing Homes: Aggregate Medicare Payments Are Adequate Despite Bankruptcies. Testimony before the Special Committee on Aging, U.S. Senate. GAO/T-HEHS-00-192. Washington, DC, September 5, 2000 (accessed October 26, 2014).
6. Jagger C, Collerton JC, Davies K, Kingston A, Robinson LA, Eccles MP, et al. Capability and dependency in the Newcastle 85+ cohort study. Projections of future care needs. BMC geriatrics 2011;11 : 21. doi: 10.1186/1471-2318-11-21 21542901
7. McGregor M, Ronald L. Residential Long-Term Care for Canadian Seniors: Non-profit, For-profit or Does it Matter? (Rep. No. 14). Montreal: IRPP Institute for Research in Public Policy., 2011.
8. Canadian Institute for Health Information. Exploring The 70 : 30 Split: How Canada's Health Care System is Financed. 2005. https://secure.cihi.ca/estore/productFamily.htm?pf=PFC588&lang=fr&media=0 (accessed October 26, 2014).
9. Grant Thornton. Residential elderly care UK sector review pp. 1–24. http://www.grant-thornton.co.uk/Documents/Private-Residential-Elderly-Care-UK-sector-review.PDF (Accessed March 18, 2016). 2014.
10. Australian Government, Productivity Commission. Trends in Aged Care Services: some implications. http://www.pc.gov.au/__data/assets/pdf_file/0004/83380/aged-care-trends.pdf. September 2008, pp. 1–267. Accessed March 18, 2016.
11. Grant Thornton New Zealand Ltd. Aged Residential Care Service Review. September 2010, pp 1–222. http://www.grantthornton.co.nz/assets/documents/home/aged-residential-care-service-review.pdf (accessed March 18, 2016)
12. Harrington C, Carrillo H, Blank BW. Nursing Facilities, Staffing, Residents, and Facility Deficiencies, 2003–08. University of California, San Francisco. pp 1–146. http://theconsumervoice.org/uploads/files/issues/OSCAR_complete_2009.pdf (Accessed February 21, 2015). 2009.
13. Harrington C, Hauser C, Olney B, Rosenau PV. Ownership, financing, and management strategies of the ten largest for-profit nursing home chains in the United States. International journal of health services: planning, administration, evaluation 2011;41(4):725–46.
14. Canadian Union of Public Employees. Residential Long-Term Care in Canada: Our Vision for Better Seniors’ Care. October 2009 (with updated appendix in 2011). pp 1–101. http://cupe.ca/residential-long-term-care-canada-our-vision-better-seniors-care (Accessed February 21, 2015).
15. Marketisation in Nordic Eldercare: A Research Report on Legislation, Oversight, Extent and Consequence. Stockholm University. pp. 1–289. Editors: Gabrielle Meagher and Marta Szebehely. http://www.normacare.net/wp-content/uploads/2013/09/Marketisation-in-nordic-eldercare-webbversion-med-omslag1.pdf (Accessed February 21, 2015).
16. Lakhani N, Whittell R. Who owns the care homes—and why are they so in debt? The Independent. Monday 05 November 2012.
17. Comondore VR, Devereaux PJ, Zhou Q, Stone SB, Busse JW, Ravindran NC, et al. Quality of care in for-profit and not-for-profit nursing homes: systematic review and meta-analysis. BMJ 2009;339:b2732. doi: 10.1136/bmj.b2732 19654184
18. Hillmer MP, Wodchis WP, Gill SS, Anderson GM, Rochon PA. Nursing home profit status and quality of care: is there any evidence of an association? Medical Care Research and Review 2005;62(2):139–66. 15750174
19. Xu D, Kane RL, Shamliyan TA. Effect of nursing home characteristics on residents' quality of life: a systematic review. Archives of Gerontology and Geriatrics 2013;57(2):127–42. doi: 10.1016/j.archger.2013.03.015 23623273
20. Castle NG, Ferguson JC. What is nursing home quality and how is it measured? The Gerontologist 2010;50(4):426–42. doi: 10.1093/geront/gnq052 20631035
21. Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. International Journal of Nursing Studies 2011;48(6):732–50. doi: 10.1016/j.ijnurstu.2011.02.014 21397229
22. Kane RA, Kling KC, Bershadsky B, Kane RL, Giles K, Degenholtz HB, et al. Quality of life measures for nursing home residents. The journals of gerontology. Series A, Biological sciences and medical sciences 2003;58(3):240–8. 12634291
23. Ramage-Morin P. Successful aging in healthcare institutions. Statistics Canada 2006;Report # 82–003.
24. Mor V, Berg K, Angelelli J, Gifford D, Morris J, Moore T. The quality of quality measurement in U.S. nursing homes. The Gerontologist 2003;43 Spec No 2 : 37–46. 12711723
25. Konetzka RT. Do not-for-profit nursing homes provide better quality? BMJ 2009;339:b2683. doi: 10.1136/bmj.b2683 19654183
26. Hill AB. The Environment and Disease: Association or Causation? Proceedings of the Royal Society of Medicine 1965;58 : 295–300. 14283879
27. Howick J, Glasziou P, Aronson JK. The evolution of evidence hierarchies: what can Bradford Hill's 'guidelines for causation' contribute? Journal of the Royal Society of Medicine 2009;102(5):186–94. doi: 10.1258/jrsm.2009.090020 19417051
28. Weech-Maldonado R, Laberge A, Pradhan R, Johnson CE, Yang Z, Hyer K. Nursing home financial performance: the role of ownership and chain affiliation. Health Care Management Review 2012;37(3):235–45. doi: 10.1097/HMR.0b013e31823dfe13 22261667
29. O'Neill C, Harrington C, Kitchener M, Saliba D. Quality of care in nursing homes: an analysis of relationships among profit, quality, and ownership. Medical Care 2003;41(12):1318–30. 14668664
30. Harrington C, Olney B, Carrillo H, Kang T. Nurse staffing and deficiencies in the largest for-profit nursing home chains and chains owned by private equity companies. Health Services Research 2012;47(1 Pt 1):106–28. doi: 10.1111/j.1475-6773.2011.01311.x 22091627
31. Bates-Jensen BM, Schnelle JF, Alessi CA, Al-Samarrai NR, Levy-Storms L. The effects of staffing on in-bed times of nursing home residents. Journal of the American Geriatrics Society 2004;52(6):931–8. 15161457
32. Munroe DJ. The influence of registered nurse staffing on the quality of nursing home care. Research in Nursing and Health 1990;13(4):263–70. 2374834
33. Schnelle JF, Simmons SF, Harrington C, Cadogan M, Garcia E, B MB-J. Relationship of nursing home staffing to quality of care. Health Services Research 2004;39(2):225–50. 15032952
34. Centers for Medicare and Medicaid Services (CMS). 2001. Report to Congress: Appropriateness of Minimum Nurse Staffing Ratios in Nursing Homes: Phase II Final Report. Baltimore: CMS. http://www.allhealth.org/briefingmaterials/abt-nursestaffingratios%2812-01%29-999.pdf (accessed September 20, 2014).
35. Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing home staffing and its relationship to deficiencies. Journals of Gerontology Series B-Psychological Sciences & Social Sciences 2000 Sep;55(5):S278–S287. 10985299
36. Harrington C, Swan JH. Nursing home staffing, turnover, and case mix. Medical care research and review 2003;60(3):366–92; discussion 93–9. 12971234
37. Canadian Aboriginal AIDS Network. Relational Care: A Guide to Health Care and Support for Aboriginal People Living with HIV/AIDS, 2008, p.8 http://caan.ca/wp-content/uploads/2012/05/Relational-Care-20081.pdf (Accessed March 18, 2016).
38. McGilton KS, Pringle DM, O'Brien-Pallas LL, Wynn F, Streiner D. Development and psychometric testing of the Relational Care Scale. Journal of Nursing Measurement 2005;13(1):51–64. 16315570
39. Grabowski DC, Feng Z, Hirth R, Rahman M, Mor V. Effect of nursing home ownership on the quality of post-acute care: an instrumental variables approach. Journal of Health Economics 2013;32(1):12–21. doi: 10.1016/j.jhealeco.2012.08.007 23202253
40. Hirth RA, Grabowski DC, Feng Z, Rahman M, Mor V. Effect of nursing home ownership on hospitalization of long-stay residents: an instrumental variables approach. International Journal of Health Care Finance and Economics 2013.
41. McGregor MJ, Tate RB, McGrail KM, Ronald LA, Broemeling AM, Cohen M. Care outcomes in long-term care facilities in British Columbia, Canada. Does ownership matter? Medical Care 2006;44(10):929–35. 17001264
42. Menec VH, Nowicki S, Blandford A, Veselyuk D. Hospitalizations at the end of life among long-term care residents. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2009;64(3):395–402. doi: 10.1093/gerona/gln034 19196640
43. Boockvar KS, Gruber-Baldini AL, Burton L, Zimmerman S, May C, Magaziner J. Outcomes of infection in nursing home residents with and without early hospital transfer. Journal of the American Geriatrics Society 2005;53(4):590–6. 15817003
44. Gillick MR, Serrell NA, Gillick LS. Adverse consequences of hospitalization in the elderly. Social Science and Medicine 1982;16(10):1033–8. 6955965
45. Dosa D. Should I hospitalize my resident with nursing home-acquired pneumonia? Journal of the American Medical Directors Association 2005;6(5):327–33. 16165074
46. Arai S, Hutchison P, Pedlar A, Lord J, Sheppard V. Shared Values, Networks and Trust Among Canadian Consumer Driven Disability Organizations. Disability Studies Quarterly 2008;28. doi: 10.18061/dsq.v28i1.68
47. Hirschman A. Exit, Voice, and Loyalty: Responses to Decline in Firms, Organizations, and States. Harvard University Press: Cambridge, US. pp. 1–176. 1970.
48. Grabowski DC. Consumer complaints and nursing home quality. Medical Care 2005;43(2):99–101. 15655422
49. Hirth RA, Banaszak-Holl JC, Fries BE, Turenne MN. Does quality influence consumer choice of nursing homes? Evidence from nursing home to nursing home transfers. Inquiry: a journal of medical care organization, provision and financing 2003;40(4):343–61. 15055834
50. Bowbliss JL. Ownership Conversion by Nursing Homes and the Quality of Care. Department of Economics, Miami University # 2009 10 2009 [cited 2009 Dec 7];1–39. http://www.fsb.muohio.edu/fsb/ecopapers/docs/bowblijr-2009-10-paper.pdf 2009.
51. Arfwidsson J, Westerberg J. Profit seeking and the quality of elder care—an empirical study of private equity's impact on the Swedish eldercare market: implications for financial performance and quality of care. Master's Thesis—Stockholm School of Economics 2014;1–47.
52. Grabowski DC, Stevenson DG. Ownership conversions and nursing home performance. Health Services Research 2008;43(4):1184–203. doi: 10.1111/j.1475-6773.2008.00841.x 18355255
53. Devereaux PJ, Schunemann HJ, Ravindran N, Bhandari M, Garg AX, Choi PT, et al. Comparison of mortality between private for-profit and private not-for-profit hemodialysis centers: a systematic review and meta-analysis. Journal of the American Medical Association 2002;288(19):2449–57. 12435258
54. Himmelstein DU, Woolhandler S, Hellander I, Wolfe SM. Quality of care in investor-owned vs not-for-profit HMOs. Journal of the American Medical Association 1999;282(2):159–63. 10411197
55. Japel C, Tremblay J, Côté S. Quality Counts! Assessing the quality of daycare services based on the Quebec Longitudinal Study of Child Development. IRPP Choices 11 (5). http://irpp.org/wp-content/uploads/assets/vol11no5.pdf (Accessed March 27, 2015). 2005.
56. Cleveland G, Forer B, Hyatt D, Japel C, Krashinsky M. New Evidence about Child Care in Canada: Use Patterns, Affordability and Quality. IRPP Choices 14 (12). http://irpp.org/research-studies/choices-vol14-no12/ (Accessed March 27, 2015). 2008.
57. McGregor MJ, Abu-Laban RB, Ronald LA, McGrail KM, Andrusiek D, Baumbusch J, et al. Nursing home characteristics associated with resident transfers to emergency departments. Canadian Journal on Aging 2014;33(1):38–48. doi: 10.1017/S0714980813000615 24398137
58. McGregor MJ, Cohen M, Stocks-Rankin CR, Cox MB, Salomons K, McGrail KM, et al. Complaints in for-profit, non-profit and public nursing homes in two Canadian provinces. Open Medicine 2011;5(4):e183–92. 22567074
59. Tanuseputro P, Chalifoux M, Bennett C, Gruneir A, Bronskill SE, Walker P, et al. Hospitalization and Mortality Rates in Long-Term Care Facilities: Does For-Profit Status Matter? Journal of the American Medical Directors Association 2015;16(10):874–83. doi: 10.1016/j.jamda.2015.06.004 26433862
60. Shapiro E, Tate RB. Monitoring the outcomes of quality of care in nursing homes using administrative data. Canadian Journal of Aging 1995;14(4):755–68.
61. Clarfield AM, Ginsberg G, Rasooly I, Levi S, Gindin J, Dwolatzky T. For-profit and not-for-profit nursing homes in Israel: do they differ with respect to quality of care? Archives of Gerontology and Geriatrics 2009;48(2):167–72. doi: 10.1016/j.archger.2008.01.001 18295359
62. Baldwin R, Chenoweth L, Dela Rama M, Liu Z. Quality failures in residential aged care in Australia: The relationship between structural factors and regulation imposed sanctions. Australasian Journal on Ageing 2014.
63. Burton C. Heavy tailed distributions of effect sizes in systematic reviews of complex interventions. PLoS ONE 2012;7(3):e34222. doi: 10.1371/journal.pone.0034222 22479569
64. Britton M. The epidemiology of mesothelioma. Seminars in Oncolology 2002;29(1):18–25.
65. Miller JH, Page SE. Complex Adaptive Systems: An Introduction to Computational Models of Social Life: Princeton University Press, 2007.
66. Grabowski DC, Hirth RA. Competitive spillovers across non-profit and for-profit nursing homes. J Health Econ 2003;22(1):1–22. 12564715
67. Berta W, Laporte A, Valdmanis V. Observations on institutional long-term care in Ontario: 1996–2002. Canadian Journal of Aging 2005;24(1):70–84.
68. McGregor MJ, Cohen M, McGrail K, Broemeling AM, Adler RN, Schulzer M, et al. Staffing levels in not-for-profit and for-profit long-term care facilities: does type of ownership matter? Canadian Medical Association Journal 2005;172(5):645–9. 15738489
69. Lucas RM, McMichael AJ. Association or causation: evaluating links between "environment and disease". Bulletin of the World Health Organization 2005;83(10):792–5. 16283057
70. Annas GJ. Burden of proof: judging science and protecting public health in (and out of) the courtroom. American Journal of Public Health 1999;89(4):490–3. 10191788
71. Kriebel D. The reactionary principle: inaction for public health. Occupational and Environmental Medicine 2007;64(9):573–4. 17704201
72. Government of Alberta. News release: Accommodations for seniors will be priority for new bonds. http://alberta.ca/release.cfm?xID=275309828DE4A-07EF-D0FE-8354B971D1CCAC47. December 16, 2009.
73. Harrington C, Armstrong H, Halladay M, Havig A, Jacobsen F, MacDonald M. Comparison of nursing home financial transparency and accountability in four locations. Ageing International 2015;November 19 (online):1–23.
74. Grabowski DC, Castle NG. Nursing homes with persistent high and low quality. Medical Care Research and Review 2004;61(1):89–115. 15035858
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2016 Číslo 4- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Why Are Some Population Interventions for Diet and Obesity More Equitable and Effective Than Others? The Role of Individual Agency
- Risk of Bias in Systematic Reviews of Non-Randomized Studies of Adverse Cardiovascular Effects of Thiazolidinediones and Cyclooxygenase-2 Inhibitors: Application of a New Cochrane Risk of Bias Tool
- The Vast and Varied Global Burden of Norovirus: Prospects for Prevention and Control
- The Association between Sulfonylurea Use and All-Cause and Cardiovascular Mortality: A Meta-Analysis with Trial Sequential Analysis of Randomized Clinical Trials
- Disentangling the Association between Statins, Cholesterol, and Colorectal Cancer: A Nested Case-Control Study
- Gender Differences in Homicide of Neonates, Infants, and Children under 5 y in South Africa: Results from the Cross-Sectional 2009 National Child Homicide Study
- Mobile Phones As Surveillance Tools: Implementing and Evaluating a Large-Scale Intersectoral Surveillance System for Rabies in Tanzania
- Building Learning Health Systems to Accelerate Research and Improve Outcomes of Clinical Care in Low- and Middle-Income Countries
- The Future of the RTS,S/AS01 Malaria Vaccine: An Alternative Development Plan
- Birth “Out-of-Hours”: An Evaluation of Obstetric Practice and Outcome According to the Presence of Senior Obstetricians on the Labour Ward
- A Nested Case–Control Study of Metabolically Defined Body Size Phenotypes and Risk of Colorectal Cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC)
- Development and Validation of a New Prognostic System for Patients with Hepatocellular Carcinoma
- Underweight, Markers of Cachexia, and Mortality in Acute Myocardial Infarction: A Prospective Cohort Study of Elderly Medicare Beneficiaries
- The Impact of Hotspot-Targeted Interventions on Malaria Transmission in Rachuonyo South District in the Western Kenyan Highlands: A Cluster-Randomized Controlled Trial
- Experimental Treatment of Ebola Virus Disease with TKM-130803: A Single-Arm Phase 2 Clinical Trial
- Is There Evidence of Poorer Birth Outcomes for Mothers and Babies When the Most Senior Obstetrician Is Not On Site?
- Clinical Implications of Cancer Genomics: A Call for Papers
- The ITA.LI.CA Staging System: A Novel Staging System for Hepatocellular Carcinoma
- Observational Evidence of For-Profit Delivery and Inferior Nursing Home Care: When Is There Enough Evidence for Policy Change?
- Child Homicide: A Global Public Health Concern
- The Chernobyl Disaster and Beyond: Implications of the Sendai Framework for Disaster Risk Reduction 2015–2030
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Observational Evidence of For-Profit Delivery and Inferior Nursing Home Care: When Is There Enough Evidence for Policy Change?
- Experimental Treatment of Ebola Virus Disease with TKM-130803: A Single-Arm Phase 2 Clinical Trial
- The Chernobyl Disaster and Beyond: Implications of the Sendai Framework for Disaster Risk Reduction 2015–2030
- Is There Evidence of Poorer Birth Outcomes for Mothers and Babies When the Most Senior Obstetrician Is Not On Site?
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



