-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Dissociation of Tissue Destruction and Bacterial Expansion during Bubonic Plague
The hallmark of bubonic plague, a disease that ravaged Medieval Europe and is still prevalent in several countries, is the bubo, a highly inflammatory and painful lymph node, which is characterized by high concentrations of bacteria within a severely damaged organ. Yersinia pestis, the causative agent, expresses a surface protease, Pla, critical to the development of bubonic plague. This multitarget protease has the potential to activate the fibrinolytic pathway and to promote destruction of extracellular protein networks within tissues. Hence, it was expected that Pla was responsible for the tissue destructions of the bubo, and consequently, for bacterial propagation and virulence. However, we found, using various engineered Yersinia strains in a mouse model of bubonic plague, that Pla proteolytic activity was dispensable for lymph node alteration, but was required to achieve high bacterial loads in the organ. Further analysis showed that Pla is essential for preventing the bacteria from being destroyed in the host. Therefore, the role of Pla as a virulence factor is to protect Y. pestis survival and integrity in the host, rather than to assist its spread through tissue destruction.
Published in the journal: Dissociation of Tissue Destruction and Bacterial Expansion during Bubonic Plague. PLoS Pathog 11(10): e32767. doi:10.1371/journal.ppat.1005222
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1005222Summary
The hallmark of bubonic plague, a disease that ravaged Medieval Europe and is still prevalent in several countries, is the bubo, a highly inflammatory and painful lymph node, which is characterized by high concentrations of bacteria within a severely damaged organ. Yersinia pestis, the causative agent, expresses a surface protease, Pla, critical to the development of bubonic plague. This multitarget protease has the potential to activate the fibrinolytic pathway and to promote destruction of extracellular protein networks within tissues. Hence, it was expected that Pla was responsible for the tissue destructions of the bubo, and consequently, for bacterial propagation and virulence. However, we found, using various engineered Yersinia strains in a mouse model of bubonic plague, that Pla proteolytic activity was dispensable for lymph node alteration, but was required to achieve high bacterial loads in the organ. Further analysis showed that Pla is essential for preventing the bacteria from being destroyed in the host. Therefore, the role of Pla as a virulence factor is to protect Y. pestis survival and integrity in the host, rather than to assist its spread through tissue destruction.
Introduction
Plague killed millions of humans during pandemics of the past and is still entrenched in regions of Asia, Africa and the Americas [1,2]. The last decades have witnessed resurgences and geographical extensions of the disease, leading WHO to categorize it as a re-emerging health problem [3,4], and there are concerns that future climatic changes might further increase the occurrence of plague outbreaks in existing or new foci [2].
Bubonic plague is the most frequent form of the disease and results from intradermal injection by an infected flea of the Gram-negative bacterium Yersinia pestis [5,6]. Bacteria proceed then, via lymphatic draining, to the proximal lymph node and expand in this organ to high numbers of widespread and infiltrating extracellular organisms [7–11]. At this stage, the swollen and highly painful draining lymph node (dLN) is referred to as a “bubo”. Without treatment, bubonic plague most often progresses to fatal septicemia [12,13]. The 50% lethal dose (LD50) of Y. pestis in mice is <10 and ~20 colony forming units (cfu) by the subcutaneous (sc) and intradermal (id) routes, respectively [6,14–16].
Y. pestis is a clonal species recently emerged from the foodborne enteropathogen Y. pseudotuberculosis [17], which causes self-limiting gastrointestinal diseases in humans [18,19] and has an LD50 in mice of 105−107 cfu following oral or sc inoculation [20,21]. Therefore, although the two species are genetically nearly identical [22], they display dramatically different pathogenic potentials. In a previous work, we used the Y. pestis/Y. pseudotuberculosis pair to explore the pathophysiology of bubonic plague [16]. Comparison of the diseases induced upon id injection of the two species showed that the dermal portal of entry newly acquired by Y. pestis is not the key to its increased virulence. The study also revealed specific histology features in the dLN within 2 days of infection. In buboes, plague was characterized by high bacterial loads, poorly contained bacterial infiltrates and widespread tissue destruction; in Y. pseudotuberculosis-infected dLNs, bacteria formed dense colonies enclosed in a focal and organized inflammatory reaction while the overall architecture of the dLN was preserved.
At this stage, it was not clear if and how the characteristics of the mature bubo were connected in a pathophysiological pathway. The severe tissue damage might have been a consequence of the high bacterial burdens, through the action of bacterial or immunological components, and conversely, destructions of the lymph node parenchyma, by removing tissue barriers, could have been a facilitating factor for the free diffusion and expansion of Y. pestis within the organ. The Y. pestis pPla plasmid is one of the few genetic determinants that differentiate the plague bacillus from its Y. pseudotuberculosis ancestor [22]. Since this plasmid has been shown to participate in bacterial dissemination in vivo and to play a major role in Y. pestis virulence [15,23–25], it was a potentially useful tool to analyze the relationships between the various features that specify a Y. pestis-infected dLN and to relate these features to virulence. pPla encodes Pla, a protease of the omptin family [26,27], which cleaves mammalian plasminogen into active fibrinolytic plasmin and inactivates several inhibitors of the fibrinolytic pathway [28]. Pla also degrades antibacterial factors [15,23,29], manipulates in vivo the pro-inflammatory response through interference with the FasL/caspase-3 pathway [30], and confers adherence to various cell lines and extracellular matrix components, either directly [31–36], or through processing of the YapE adhesin [37]. The pla gene encoding Pla is abundantly expressed in the dLN of Y. pestis-infected mice [38]. In heterologous expression systems, the proteolytic action of Pla at the bacterial surface is hampered by the O-antigen (O-Ag) fraction of the outer membrane lipopolysaccharide [39]. However, Pla is fully active in Y. pestis because genes encoding the O-Ag synthesis enzymes are naturally non-functional in this species [40].
The aim of this work was to use Y. pestis and Y. pseudotuberculosis strains differentially expressing Pla to analyze three defining characteristics of the bubo: infiltrating and diffuse pattern of bacterial invasion, extensive and disrupting tissue damage, and elevated bacterial titers. This approach helped us dissect the bubonic plague complex phenotype, uncovering new insights into the causal links between the various manifestations of the disease and their relation to outcome.
Materials and Methods
Animal ethics
Animals were housed in the Institut Pasteur BSL3 animal facility accredited by the French Ministry of Agriculture to perform experiments on live mice (accreditation B 75 15–01), in compliance with French and European regulations on care and protection of Laboratory Animals (EC Directive 86/609, French Law 2001–486 issued on June 6, 2001). Protocols were approved by the Institut Pasteur Veterinary Staff and performed in compliance with the NIH Animal Welfare Insurance #A5476-01 issued on 02/07/2007.
Bacteria and plasmids
Bacterial strains and plasmids used in this study are listed in Table 1. Bacteria were grown using Luria-Bertani medium (LB), supplemented (Yersinia) or not (Escherichia coli) with 0.002% (w/v) hemin (LBH), at 28°C and 37°C, respectively. Selection for trimethoprim resistance was done using Müller-Hinton medium. Chloramphenicol (25 μg.ml-1), kanamycin (Km: 30 μg.ml-1) or trimethoprim (Tmp; 100 mg.ml-1) was added to the media as necessary. All experiments involving Yersinia strains were performed in a BSL3 laboratory.
Tab. 1. Plasmids and bacterial strains. 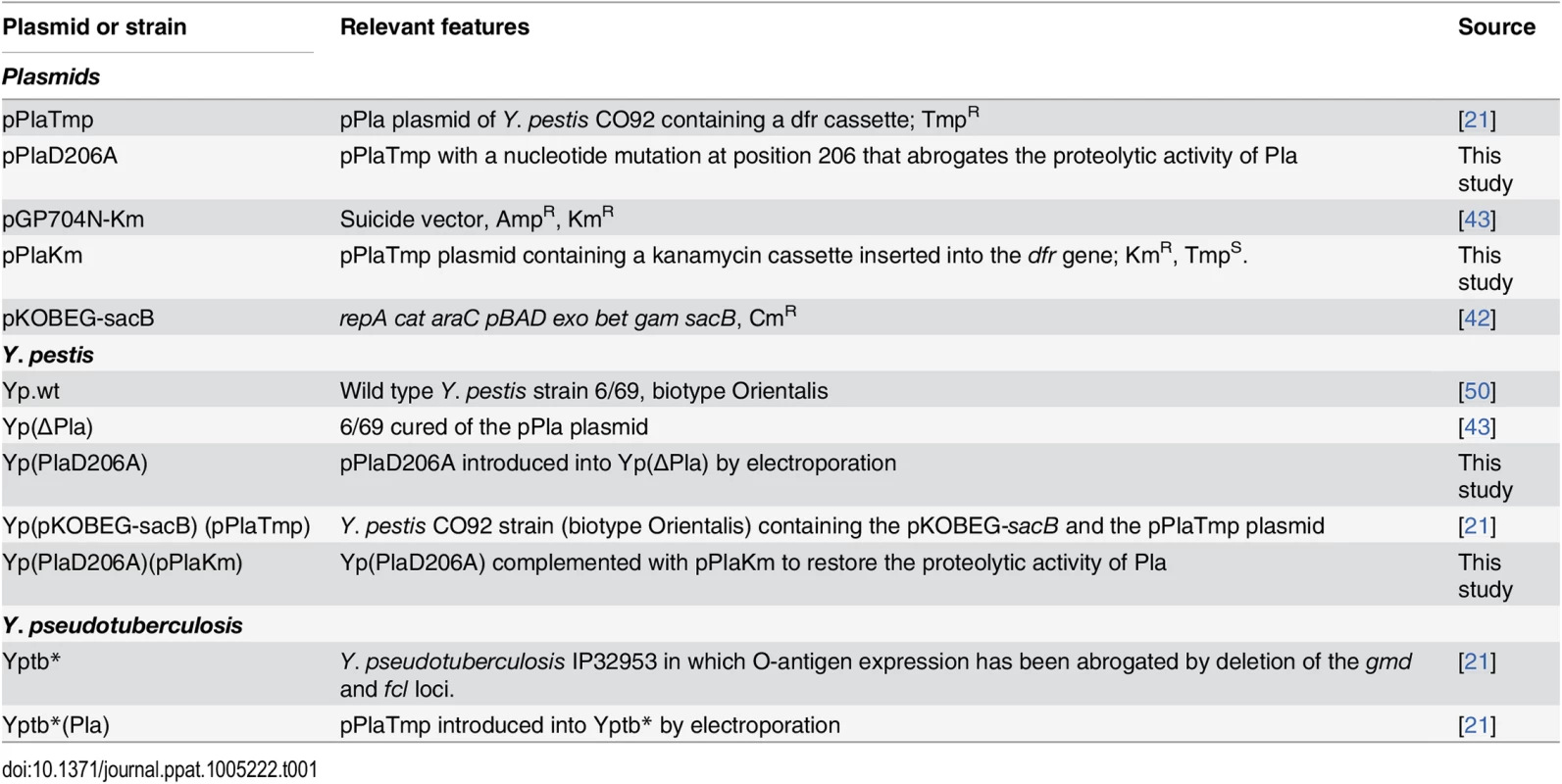
Mutagenesis of pla
Single nucleotide replacement in pla was performed by PCR amplification of the whole 9.6 kb pPlaTmp plasmid from strain Yptb*(Pla) (Table 1), using the divergent non-overlapping primers 896 and 897 harboring the required mutation (S1 Table) and a high-fidelity DNA Polymerase (Phusion, NewEnglandBiolab) [41]. The 80 μl reaction mix, containing 0.125 mM dNTP, 0.1875 μM of primers and 0.5 μl of Taq Polymerase, was incubated for 5 min at 98°C and subjected to 30 cycles of denaturation (30 s at 98°C), annealing (30 s at 60°C), and extension (3 min 30 s at 72°C), and a final cycle of extension (7 min at 72°C). The resulting PCR product was digested with DpnI to cleave the methylated template and subjected to electrophoresis. The band with the expected size was excised from the gel, extracted using the QIAquick Gel Extraction Kit (Qiagen), and introduced into E. coli DH5α by transformation. Recombinant clones were selected on Tmp plates and plasmids were extracted using the Plasmid maxi kit (Qiagen). Sequencing of the entire replicon, using the primers listed in S1 Table showed that it was 100% identical at the nucleotide level to the pPla template, except at position 7,341 in pla where the A was replaced by a C at the second position of the codon, leading to the expected replacement of an aspartic amino acid by an alanine at position 206 of the Pla protein sequence. The recombinant plasmid, designated pPlaD206A, was introduced by electroporation into Yp(∆Pla). Recombinant Y. pestis, designated Yp(PlaD206A) (Table 1), were selected on Tmp agar plates and the presence of the Tmp cassette was verified by PCR with primer pair 260B/C (S1 Table). To confirm the presence of the recombinant pPlaD206A plasmid, the PCR product encompassing this region (primers 839A/B (S1 Table)) was digested with BlpI, which only cleaves the A/C mutated site.
Complementation of Yp(PlaD206A) with a functional pla gene
In order to obtain a pPla plasmid labeled with an antibiotic cassette other than Tmp (already present on pPlaD206A), the dfr locus of the pPlaTmp plasmid was replaced by a Km cassette using the short flanking homologous regions (SFH)-PCR procedure [42]. Briefly, the Km locus was PCR amplified from the pGP704N-Km template [43] with primer pair 954A/B (S1 Table) that encompass the extremities of the Km cassette and 50 bp of the dfr gene. This PCR product was introduced into Yp(pKOBEG-sacB)(pPlaTmp) [21] by electroporation. KmR colonies were tested for correct allelic exchange between the PCR product and the target site by PCR with primers 932/933 (S1 Table) and 260B/C [21], located at each end of the kan cassette and outside the dfr gene, respectively. All colonies contained both pPlaTmp and pPlaKm. To obtain Y. pestis clones containing pPlaKm, but devoid of pPlaTmp, the plasmids were extracted with the QuickLyse Miniprep kit (Qiagen) and introduced by electroporation into Yp(ΔPla). KmR clones, designated Yp(pPlaKm) (Table 1) were selected. The presence of the pPlaKm and the absence of pPlaTmp were confirmed by PCR with primer pairs 932/933 and 260B/C. Transfer of pPlaKm to Yp(PlaD206A) after plasmid extraction and electroporation resulted in the generation of Yp(PlaD206A)(pPlaKm) (Table 1). The presence of both the wild type and the mutated versions of pla was verified by amplification of the region encompassing the A -> C replacement on pla with primers 839A/B (S1 Table), followed by digestion with BlpI. The presence of three bands (one corresponding to the uncut wild type version of pla, and the other two to the fragments generated by the BlpI cleavage), confirmed the presence of the two forms of pPla in the strain.
Plasminogen-activation assay
The assay was performed as described [21,44], with slight modifications: bacteria were incubated at 37°C in Ca/Mg-free phosphate buffer containing 4 μg human Glu-plasminogen (American Diagnostica) and 30 μl of a 3 mM solution (in H20) of the chromogenic plasmin substrate S-2251 (Chromogenix) in a total volume of 200 μl. Breakdown of the chromogenic substrate was monitored by serial measurements of absorbance at 405 nm (A405) using a microtiter-plate reader. Experiments were performed in duplicate and at least twice.
Mouse infection
Eight-week old female OF1 mice (Charles River, France) were anesthetized by intraperitoneal injection of 10 mg.kg-1 Xylazine (Rompun 2%, Bayer, Germany) + 100 mg.kg-1 Ketamine (Imalgène 1000, Merial, France) and infected as described [16,45]. Briefly, bacteria grown overnight on LBH agar medium were adjusted to the desired concentration in saline, based on A600 measurement, and 10 μl (5,000 cfu) were injected id into the mouse ear pinna. Cfu counts were verified by plating on LBH. Control mice received the same volume of saline without bacteria. Mice were followed up for 21 days for survival. For cfu enumeration or histology examination of the LN, infected mice were euthanized by cervical dislocation at 48h post-infection (pi), unless otherwise specified, and the ipsilateral superficial parotid LN [46], which drains the injection site [16], was harvested.
Histology and immunohistochemistry
LNs were first collected in a Zinc-based preservative [47,48] and then embedded in low melting-point paraffin (Poly(ethylenglycol) diesterate, Aldrich). Four μm sections were stained with standard hematoxylin-eosin (HE) staining [49]. For immunohistochemistry, sections were treated for endogenous peroxidase activity by incubation for 20 min in 0.3% (v/v) H2O2, and for 20 min in normal serum from the appropriate animal host (dilution 1 : 10 in PBS (pH 7.4) containing 1% (w/v) milk powder) prior to incubation for 1 h with one of the following antibodies: rabbit polyclonal antiserum against the Y. pestis F1 Ag or the Y. pseudotuberculosis serotype I O-Ag (produced by the French Reference Center for Yersinia, Institut Pasteur), or a rat anti-mouse CD45R (B220 clone, Caltag). After three washes in PBS-1% (w/v) milk powder, LN sections were incubated for 1 h with the following secondary antibodies or reagent (Dako): EnVision+System HRP-labeled anti-rabbit (undiluted), streptavidin-peroxidase conjugate (diluted 1 : 600), or rat-specific biotinylated Ig (diluted 1 : 400) followed by streptavidin-peroxidase conjugate. Bound peroxidase activity was detected using 3-amino-9-ethylcarbazole (AEC) substrate (Sigma). Tissues were counterstained with Harris’ hematoxylin. Sections were photographed with a DMX1200 or DS-Fi1 Nikon Camera connected to an E800 or E600 Nikon microscope equipped with 2× to 100× Plan Apochromat objectives, or scanned with a MiraxScan Z1 from Zeiss.
Statistical analyses
Statistical analyses were performed with the Prism version 5 for Mac software (GraphPad Software, San Diego California), using the Student’s t test or Mann-Whitney U test, depending on the distribution of the data, to compare bacterial loads in organs and the log-rank test to compare mortality rates.
Clustering analysis of the LN lesional patterns: histology sections were scored according to previously described criteria of histology lesions in the lymph node [16]. Each sample was scored as « 0 » or « 1 » for each of the criteria related to tissue damage and inflammatory reaction, so that a « 0 / 1 » table gathering the lesional patterns of all samples was created. The table was computed by the BioNumerics software, version 6.6 (Applied Maths, Kortrijk, Belgium), using the Minimum Spanning Tree approach to analyze and display the similarity of the patterns.
Results
Y. pestis infiltrating pattern of progression in the bubo does not require pPla
Following injection of Y. pestis into the dermis, bacteria disseminate to the dLN. They first settle and spread in the subcapsular sinus, from which multifocal bacterial extensions subsequently penetrate into the cortex [11,16]. In contrast, the closely related species Y. pseudotuberculosis forms in the dLN discrete peripheral clumps separated from the parenchyma by an inflammatory cell mantle [16]. To determine whether the Y. pestis-specific plasmid pPla was responsible for the infiltrating behavior of Y. pestis, we used a set of four strains: (i) wild type Y. pestis (Yp.wt), (ii) its derivative cured of the pla-bearing plasmid pPla (Yp(ΔPla)), (iii) a Y. pseudotuberculosis strain in which O-Ag production has been abrogated (Yptb*) [21], and (iv) its derivative in which pPla was introduced (Yptb*(Pla), [21] (Table 1). The use of an O-Ag-deprived strain of Y. pseudotuberculosis was necessary because the activity of Pla is inhibited in the presence of the lipopolysaccharide side chains [39]. We previously showed that the plasminogen activator activity of the recombinant Yptb*(Pla) strain is similar to that of Yp.wt [21]. Each of the four strains was inoculated in the mouse ear pinna at a dose of 5,000 cfu. This loading dose was found in an earlier work to produce well-developed lymphadenites exhibiting distinct features of Y. pestis versus Y. pseudotuberculosis infection [16]. Two days after infection, the animals were euthanized and the ipsilateral superficial parotid dLN was taken for microscopic examination. Immunostaining of dLNs infected with either Yp.wt or Yp(∆Pla) evidenced diffuse and infiltrating bacterial projections towards the LN center in both cases (Fig 1A). The similar pattern of bacterial infiltration between pPla-positive and -negative Y. pestis was confirmed at higher magnification (Fig 1B). In contrast to Y. pestis, Yptb* and Yptb*(Pla) assumed a less diffuse spatial distribution, forming compact bacterial patches located at the dLN periphery (Fig 1A). However, at higher magnification, Pla-expressing Y. pseudotuberculosis bacteria were often found to form less densely packed colonies than Yptb* (Fig 1B), suggesting that pPla might slightly increase the diffusing potential of Y. pseudotuberculosis.
Fig. 1. Distribution and infiltration pattern of bacteria in dLNs infected with Y. pestis or Y. pseudotuberculosis strains containing or not the pPla plasmid. 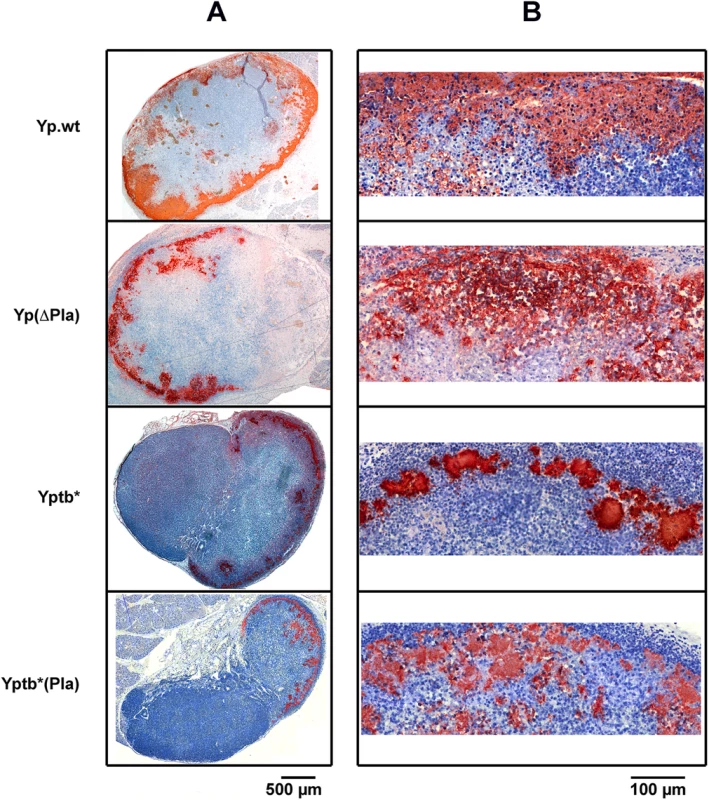
Mice were infected id in the ear with 5x103 cfu of each strain. At 48 h post infection mice were sacrificed and the ipsilateral superficial parotid LN was collected. LN sections were immunostained with an anti-Y. pestis (first two rows) or -Y. pseudotuberculosis (last two rows) antiserum. Bacteria have an orange-brown coloration, and the tissues are counterstained with hematoxylin (blue). (A) and (B) panels represent low- and high-magnification pictures, as indicated by the corresponding scale bars. Strains are denoted as in Table 1. The figure shows typical aspects observed in a panel of 68 examined LNs (20 infected with Yp.wt, 26 with Yp(ΔPla), 11 with Yptb* and 11 with Yptb*(Pla)). Therefore, although pPla may participate in the infiltrating pattern that typifies a bubo, its role appears to be minor. This plasmid is not responsible for the difference in bacterial containment observed between Y. pestis and Y. pseudotuberculosis, and is not a requisite for Y. pestis infiltration of the dLN.
Destructive lesions in the bubo are not caused by pPla
We previously showed that on day 2 pi, the dLNs of mice infected id with Y. pestis exhibited destructive lesions leading to alterations of the tissue density and a breakdown of the functional organization of the organ, while dLNs of mice infected with Y. pseudotuberculosis displayed peripheral abscesses but kept an otherwise normal architecture [16]. To estimate the contribution of pPla to the destruction of the LN architecture, mice were infected with Yp.wt, Yp(ΔPla), Yptb* and Yptb*(Pla) and LN histopathology was examined at 48h pi. Hematoxylin-eosin (HE) staining of the dLNs infected with either Yp.wt or Yp(ΔPla) revealed comparable heterogeneous tissue structures with zones of tissue depletion and necrosis (Fig 2, HE). Disruption of the LN follicular organization by both pPla-positive and -negative Y. pestis was also seen on sections immunostained to reveal B lymphocytes: these cells no longer occupied the outermost regions of the organ, as in normal LNs. They composed instead fragmented islets that were not restricted to the periphery (Fig 2, BL). LNs infected with Yptb* or Yptb*(Pla) (Fig 2) displayed in both cases preserved tissue density (Fig 2, HE) and the follicular architecture was also conserved, as B cells were located at the organ periphery or homogeneously forced inward by an organized and contained inflammation (Fig 2, BL). A grouping analysis of the histology lesions confirmed that the lesional profiles clustered according to the infecting species, and not to the presence of Pla (S1 Fig).
Fig. 2. Histology of dLNs infected with Y. pestis or Y. pseudotuberculosis strains containing or not the pPla plasmid. 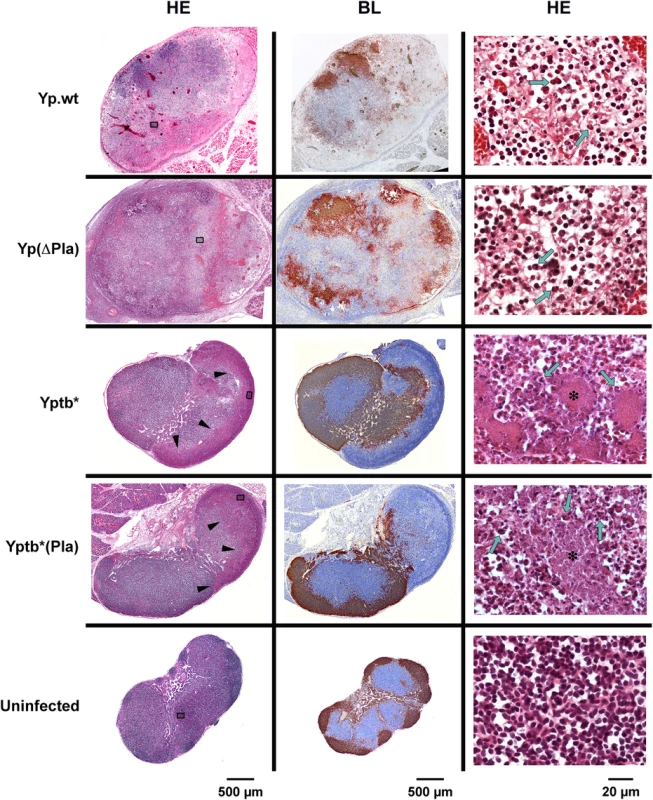
Mice were infected id in the ear with 5x103 cfu of each strain and dLNs were collected 48h later. An uninfected LN is shown for comparison. HE: hematoxylin-eosin staining; BL: immunostaining of B lymphocytes (brown), and counterstaining with hematoxylin (blue). In Yp.wt- and Yp(ΔPla)-infected nodes (first two rows): areas of lymphoid tissue depletion and necrosis appear on low-magnification HE pictures (left column) as zones of lower staining intensity or as irregular pink areas; at higher magnification (right column), dissociation of the lymphoid tissue, deposition of eosinophilic fibrillar material, and the presence of necrotic cells and cell debris characterize the necrotic process; typical PMNs harboring horseshoe-shape nuclei are visible (green arrows). In Yptb* and Yptb*(Pla)-infected nodes (third and fourth rows): on low-magnification HE pictures, arrowheads indicate the limits of the inflammatory infiltration clearly delineated from the rest of the organ; higher magnifications show that the inflammatory infiltration is essentially made of PMNs (green arrows), which come in close contact with the bacterial foci (stars). In uninfected LNs (last row), the lymphoid tissue density and follicular organization (B cells at the periphery) are normal. Strains are denoted as in Table 1. Sections of infected dLNs shown here are from the same dLNs as in Fig 1. The position of the fields shown in the right column is marked by grey rectangles in the corresponding low-magnification HE sections. These findings thus show that histological features characteristic of the plague bubo, i.e. disappearance of the organ functional architecture, destructive alterations of the tissue, and lack of an organized innate cell response [10,11,16], are specific for the plague bacillus, but independent of pPla. Therefore, pPla is neither required nor sufficient for the destruction of the LN structure that characterizes a Y. pestis infection.
dLN bacterial titers are determined by Pla catalytic activity
Overwhelming bacterial loads in mature buboes represent another distinctive feature of Y. pestis infections [11,12,16]. This characteristic has been linked to the presence of pPla by histological observations [15,24], but no quantification of the effect of pPla on bubo bacterial loads has ever been performed. To quantitatively assess the impact of pPla on the bacterial ability to multiply in the dLN, 5,000 cfu of Yp.wt, Yp(∆Pla), Yptb* and Yptb*(Pla) were inoculated id and cfu enumerations in the dLN were carried out on day 2 pi. As shown in Fig 3, loss of pPla by Y. pestis resulted in a reduced proportion of infected dLNs (87.5% for Yp.wt versus 65% for Yp(∆Pla)), and in dLNs that were infected the amount of pPla-cured bacteria was on average ~1,000 fold lower than that of the wild type, confirming that pPla is required for achievement of high Y. pestis loads in the bubo. Furthermore, in the presence of pPla mean Y. pseudotuberculosis bacterial titers increased significantly to reach levels similar to those of Yp.wt (Fig 3). Thus pPla, whether in Y. pestis or a Y. pseudotuberculosis, enhances bacterial expansion in the dLN.
Fig. 3. dLN colonization by Yersinia strains differentially expressing the proteolytic activity of Pla. 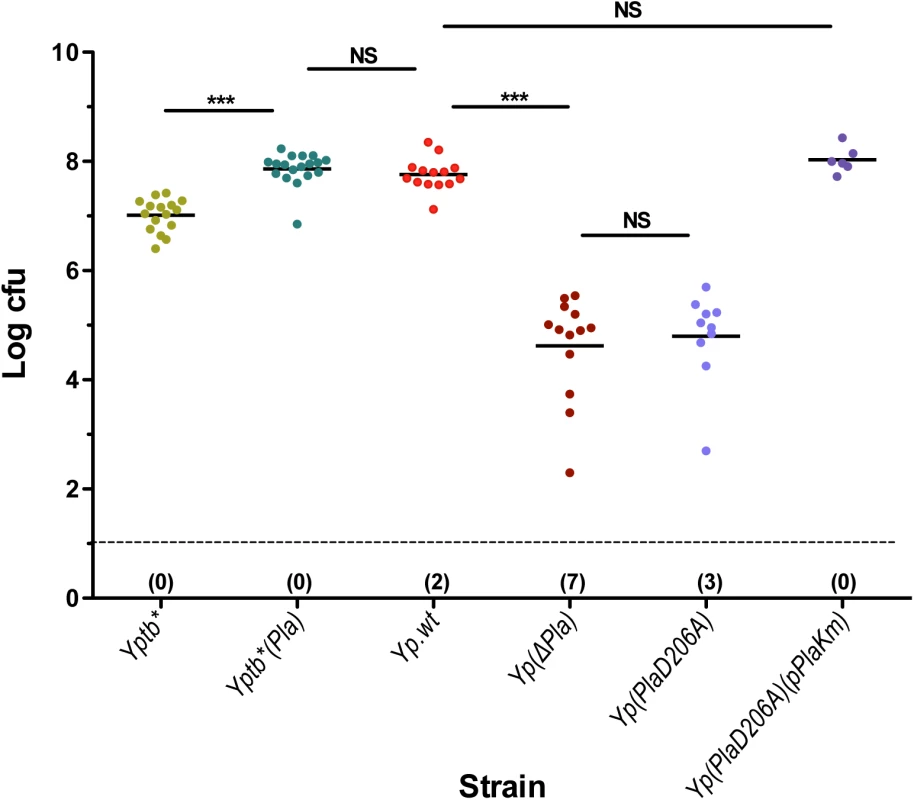
Mice were infected id in the ear with 5x103 cfu of each strain. At 48 h pi mice were sacrificed and colonization of the ipsilateral superficial parotid LN was determined. Each dot represents an individual animal. Black bars correspond to the mean number of cfu in colonized LNs. The dashed line indicates the limit of detection. In parenthesis below the dashed line is indicated for each group the number of LNs with no detectable live bacteria. Mean numbers of cfu in colonized LNs were compared using t-test, as data were normally distributed in all groups. NS: P > 0.05; ***: P ≤ 0.0001. Strains are denoted as in Table 1. Since Pla is a multifunctional protein, we wanted to determine whether its capacity to promote bacterial multiplication in the dLN was due to its proteolytic activity. We constructed strain Yp(PlaD206A) (Table 1), which differs from Yp.wt by a single point mutation that was previously shown to abolish the proteolytic action of Pla [44]. In an E. coli expression system [44] as well as in Y. pestis [25], the D206A Pla mutation rendered the bacteria unable to activate plasminogen in vitro. We confirmed here that the D206A mutation in Pla abolishes its plasminogen activator activity (S2 Fig). Upon id injection of Yp(PlaD206A), the dLN bacterial burden of the mutant strain was strongly decreased, to a level similar to that of the pPla-cured derivative (Fig 3). To ensure that this impaired growth in the dLN was caused by the mutation, a Km-labeled pPla plasmid carrying the wild type pla allele was introduced into strain Yp(PlaD206A). The bacterial load of the complemented strain Yp(PlaD206A)(pPlaKm) reached levels comparable to those of the wild type Y. pestis strain (Fig 3). Therefore, the D206A mutation alone had the same impact on the capacity of the bacteria to survive and multiply in the draining lymph node as that of loss of the whole plasmid, highlighting the prominent role of the Pla catalytic activity for bacterial expansion in the dLN during bubonic plague.
Mouse mortality correlates with dLN bacterial loads, but not with bacterial distribution and tissue damage
Pla is a major virulence factor of various Y. pestis strains upon id or sc infections [14,15,23,24,51]. However, some strains, such as Pestoides F and strain 358, do not require pPla for full virulence [15,52]. In this study we used Y. pestis strain 6/69 because a pPla-cured derivative was available in our strain collection. To evaluate the contribution of pPla to the pathogenic potential of strain 6/69, mice were infected id with 5,000 cfu of Yp.wt or Yp(∆Pla) and monitored for 21 days after injection. The survival curves showed that the high virulence of the parental strain, which killed 83% of mice within 4 days, was strongly attenuated in the absence of pPla, with most of the animals being still alive (Fig 4A) and apparently in good health at the end of the observation period. This confirms that Pla is a major virulence factor also of Y. pestis 6/69. When the D206A mutation was introduced into pla, the Yp(PlaD206A) resulting strain was as attenuated as the Yp(∆Pla) derivative following injection in the ear pinna (Fig 4A). Reintroduction of a pPla plasmid carrying a functional pla gene restored the pathogenicity of the mutant strain (Fig 4A). Thus, in a bubonic plague model, host mortality strongly depends on the proteolytic activity of Pla. Furthermore, since we showed in this study that Pla is not required for Y. pestis 6/69 to produce large-scale tissue damage and bacterial infiltrating pattern, our data demonstrate that histopathological lesions and outcome are dissociated during bubonic plague.
Fig. 4. Mortality rates and kinetics in mice infected with A) Y. pestis or B) Y. pseudotuberculosis strains. 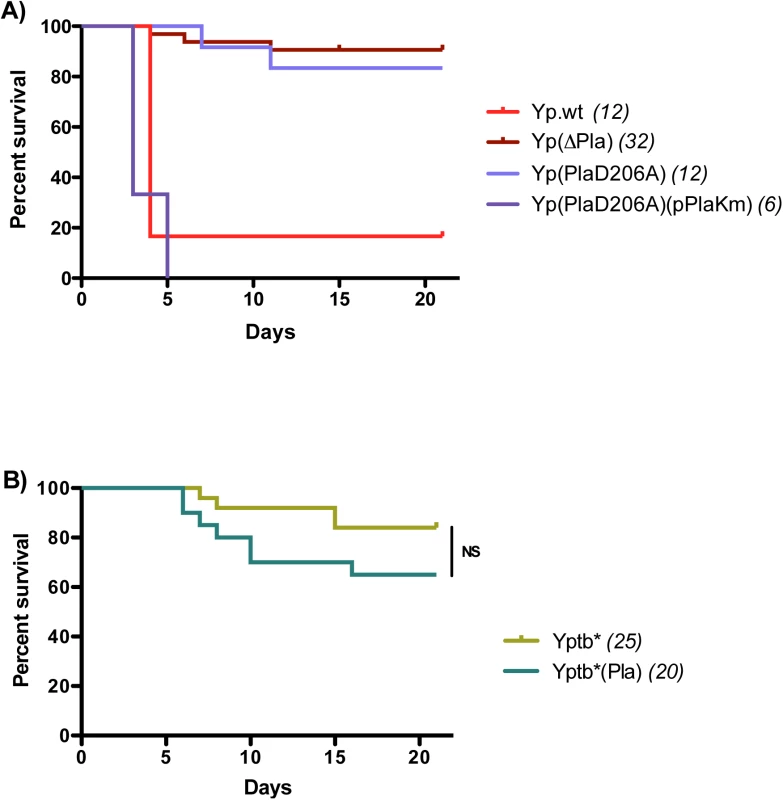
Mice were infected id in the ear with 5x103 cfu and followed up for survival studies. In parenthesis are indicated the numbers of animals analyzed for each strain. NS: P > 0.05. In contrast, production of heavy bacterial loads in the dLN correlates to the death of the animals, consistent with the possibility that reaching a sufficient level of bacterial infection in the proximal LN is a decisive step for plague pathogenicity. To further explore the pathophysiological repercussions of high bacterial titers in the dLN, we took advantage of the fact that pPla was able to boost Yptb* expansion in the dLN to levels as high as those achieved by Yp.wt, and we asked whether these increased bacterial titers would result in an enhanced virulence of the complemented strain. Accordingly, mice were infected id with Yptb*(Pla) and followed up for survival. The pPla-complemented strain killed more mice and more rapidly than did the parent strain, but the difference failed to reach statistical significance (Fig 4B). The fact that Yptb*(Pla) was not as virulent as Yp.wt although the two strains reached similar bacterial loads in the dLN prompted us to explore the ability of the two strains to disseminate beyond the dLN. Spleen cfu titers at 48h did not significantly differ between Yp.wt and Yptb*(Pla) (log10 medians = 6.1 and 5.3, respectively, p = 0.0952). Therefore, neither high bacterial loads in the dLN nor the ability to disseminate to the bloodstream are sufficient to cause a fatal outcome. Other Y. pestis-specific pathophysiological mechanisms must play a role during bubonic plague to promote efficient host killing.
Pla proteolytic activity protects Y. pestis from massive destruction in the dLN
Pla-mediated bacterial expansion in the LN at 48h may result from: (i) a higher capacity to reach the dLN, (ii) an increased multiplication rate and/or iii) a lower death rate of the bacteria in the organ. Cfu enumerations of Pla-negative and wild type Y. pestis bacteria at an early time point (24h) pi showed that they were present in similar amounts in the dLN (S3 Fig), indicating that pPla is not required for the initial colonization of the dLN and that the difference in bacterial loads observed at 48h pi results from mechanisms that take place after translocation to and multiplication in the LN. High magnification images of 48h dLN preparations immunostained to highlight bacteria revealed differences between wild type and Pla-deficient Y. pestis infections that were not visible at lower scale. In dLNs infected with Yp.wt, large clusters of bacteria with an intact shape were visible (Fig 5). In contrast, sections of dLN infected with Yp(∆Pla) displayed a fragmented staining pattern, made of irregular dots suggestive of bacterial debris (Fig 5). Similar observations were made on Yp(PlaD206A)-infected dLN sections (S4 Fig). A consistently low number of intact bacteria per section (0 to 12) could be seen across all (N = 26) Yp(∆Pla) - or Yp(PlaD206A)-infected dLN preparations examined. The massive difference in bacterial integrity between wild-type and Pla-deficient Y. pestis was highly consistent. No exceptions were found among all infected LN preparations examined. These results thus indicate that a major role of Pla in the dLN is to prevent bacterial destruction, presumably by counteracting the host immune system and/or overcoming nutritional limitations.
Fig. 5. Impact of pPla on bacterial morphology in the dLN. 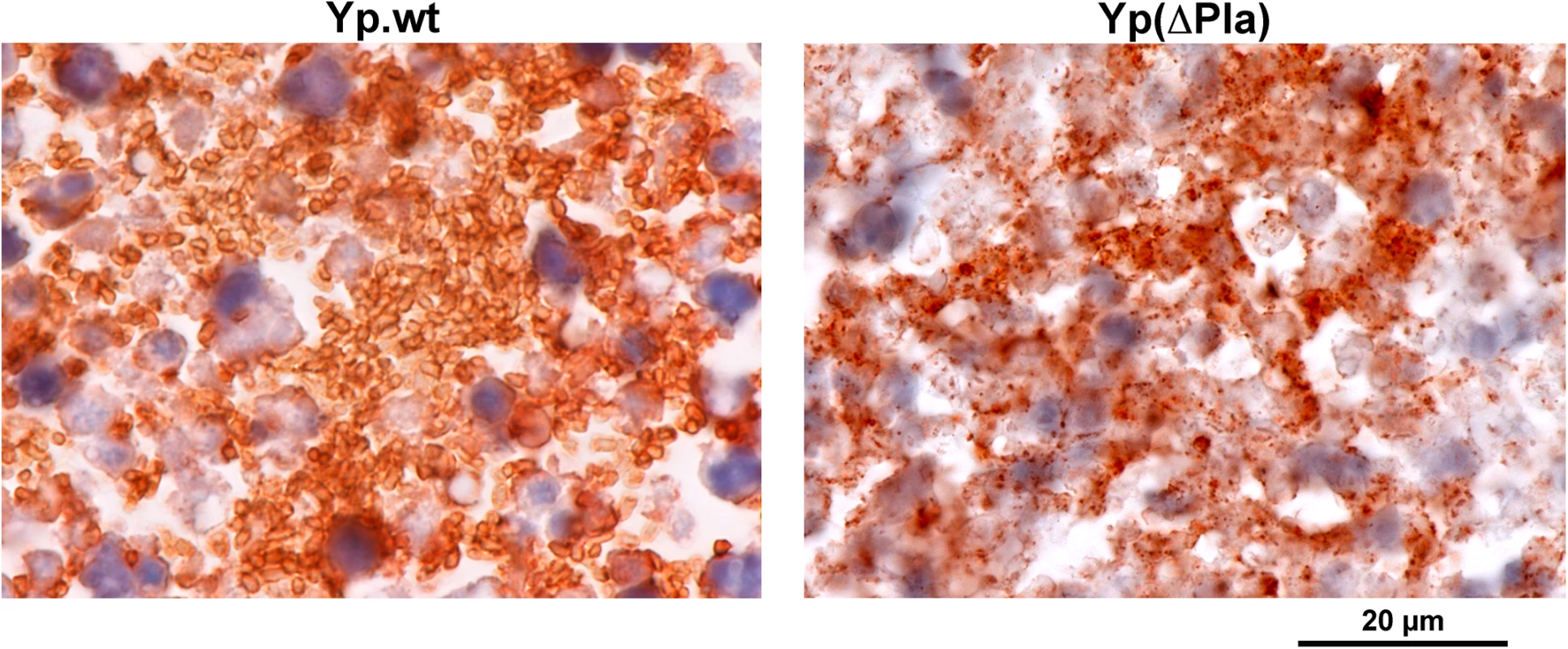
LNs were collected 48h after id inoculation of 5x103 cfu of the indicated strain and sections were immunolabeled with an anti-Y. pestis antiserum. In the left panel, the orange-brown staining delineates abundant and apparently intact bacteria typical of wild-type Y. pestis (Yp.wt) infections, contrasting with the punctate staining pattern observed after infection with the Y. pestis variant devoid of pPla (Yp(∆Pla), right panel). Discussion
During the evolutionary process of its emergence from Y. pseudotuberculosis, Y. pestis acquired the multifunctional protein Pla, which is a powerful determinant of virulence and dissemination [23,25]. The best-characterized function of Pla in vitro is the up regulation of the host fibrinolytic system by both proteolytic transformation of the precursor plasminogen to active plasmin and inactivation of plasmin inhibitors [28,53]. Plasmin, a broad-spectrum serine protease, is the main fibrin-clot degrading enzyme and is thus central to the coagulation/fibrinolysis balance. Because its targets include procollagenases and structural proteins of interstitial matrices and basement membranes, it is also important in connective tissue homeostasis [54]. Direct or indirect activation of the host plasminogen is a common invasive strategy among pathogenic bacteria belonging to diverse genera, such as Streptococcus, Staphylococcus, Borrelia, Helicobacter, Bacillus, Salmonella and Leptospira [26,55–57]. This strategy was also found in parasites and fungi [58–60]. It has been suggested that a function of bacterial plasminogen activating systems is to destabilize host barriers created by fibrin and extracellular protein networks to enable bacterial expansion [53,55,61,62], in a way reminiscent of the use of plasmin by metastatic cancer cells [63]. Although there is little in vivo evidence to support this “bacterial metastasis” hypothesis, there have been several reports of bacterial plasminogen activators promoting the crossing of reconstituted extracellular matrices (ECM) and basal membranes in vitro [55,61,64]. The dramatic LN disruption observed in bubonic plague, associated with exceedingly high amounts of bacteria infiltrating the organ, led us to speculate that, within the frame of the bacterial metastasis model, these two features were pathogenetically linked.
However, using Y. pestis mutants lacking Pla or its proteolytic activity in a mouse bubonic plague model, we found that extensive tissue damage and uncontrolled bacterial burdens are uncoupled. The destructive alterations of the bubo characteristic of Y. pestis infections do not require the Pla-encoding plasmid pPla, which is nonetheless key to bacterial outgrowth in the organ. Likewise, introduction of pPla in Y. pseudotuberculosis increased the bacterial load up to wild type Y. pestis levels, but did not result in severe histological alterations of the dLN. Hence, the mode of action of Pla underlying its virulence potential is not primarily to extensively disorganize the dLN matrix protein network to clear the way for bacterial spread. Conversely, in the absence of pPla the tissue breakdown of the Y. pestis-infected dLN is not sufficient to promote bacterial accumulation.
Since Pla proteolysis is not involved, the mechanisms leading to dLN damage remain to be determined. Inflammatory responses to infections are normally accompanied by tissue destruction in and around infectious foci, chiefly owing to the release of various polymorphonuclear neutrophil (PMN) toxins, among which matrix metalloproteases and the serprocidin family of antibiotics proteins degrade most of the ECM components [65–67]. Therefore the PMN response visible in Y. pestis-infected LNs, although disorganized, could at least in part account for the observed tissue alterations. However, Y. pseudotuberculosis-infected dLNs are abundantly infiltrated by PMNs [16] without exhibiting Y. pestis-like destructive lesions. Apoptosis of immune cells, a hallmark of severe sepsis [68,69], may be another cause of the profound cell depletion of wild type Y. pestis-infected buboes, but is unlikely to play an important role during the less severe infection caused by the Pla-deficient strains.
While pPla is not the determinant of LN destructions, our observations confirm quantitatively its critical importance in the formation of bacteria-ridden buboes. We previously observed [16] and we confirm here that Y. pseudotuberculosis is significantly less abundant than Y. pestis in the infected dLNs at 48h pi. This difference in bacterial load between Y. pestis and Y. pseudotuberculosis is completely abolished when pPla is introduced into Y. pseudotuberculosis. pPla is thus a key genetic element to endow the bacteria with the capacity to survive and multiply in the dLN, and we further show that this capacity is due to the proteolytic activity of Pla. This protein could act on the bacterial load either by protecting the bacteria from the bactericidal action of innate immune defenses, or by providing them with an environment favorable for their growth. Our observation that the LNs of mice infected with Y. pestis strains lacking Pla catalytic activity contained many bacterial debris with few intact Y. pestis cells, reveals that Pla protects bacteria from undergoing lysis in the host. It is likely that most of the bacterial destruction takes place in the dLN, instead of the bacterial debris being drained from the dermis, because on day 1 pi, live Yp(∆Pla) cells are present in quantities comparable to those of wild type Y. pestis, their titers subsequently declining between 24h and 48h. Among the innate bacteriolytic factors that have been tested, Yp(∆Pla) is resistant to complement [23] but sensitive to the cationic antimicrobial peptides (CAMPs) human LL-37 and murine CRAMP [29]. CAMPs are small amphipathic molecules that bind to lipid components (hydrophobic region) and phospholipid groups (hydrophilic region) of the bacterial cell membranes, thereby causing disintegration of the lipid bilayer structure [70]. It has been reported that some CAMPs are targets of Pla and other bacterial omptins in vitro, and the proteolytic function of Pla prevents bacteriolysis by LL-37 and CRAMP [29,71–73]. This protection, however, was only effective in the absence of the F1 capsule, which is normally expressed in the bubo. This implies that degradation of the above CAMPs is not likely to account for the dramatically different survival rates in the bubo between wild-type and Pla-defective Y. pestis strains. Other possible mechanisms of Pla-mediated protection against in vivo bacteriolysis include targeting of other factors of the immune system or providing essential nutrients requiring a proteolytic degradation to become available to bacteria in the LN environment.
It is also worth noting that removal of pPla from Y. pestis or inactivation of the proteolytic activity of Pla impaired the bacterial load in the dLN to an extent higher than that of the naturally pPla-negative Y. pseudotuberculosis strain. Y. pseudotuberculosis, the ancestor of Y. pestis, is an enteropathogen that has a tropism for lymphatic tissues and in particular for the mesenteric lymph nodes during its transit through the intestinal tract. Numerous genes were either lost or inactivated in Y. pestis after it evolved from Y. pseudotuberculosis [22,74]. It is thus possible that during its evolution, Y. pestis lost some of the Y. pseudotuberculosis ancestral functions involved in bacterial survival in LNs, while acquiring pPla, which conferred a higher capacity to survive and multiply in these lymphoid organs. Interestingly, the same phenomenon was recently reported in a study involving Y. pestis Pestoides F, a pPla-negative intermediate between Y. pseudotuberculosis and modern Y. pestis. In a murine model of pneumonic plague, Pestoides F was more fit than ∆Pla-Y. pestis to colonize the lung, suggesting that Pestoides F was still harboring the Y. pseudotuberculosis ancestral functions subsequently lost during the evolution of Y. pestis [75]. Another consequence of this evolution may be the bottleneck effect that restricts access to the dLN from the dermis [76]. It is interesting that in our work and in other studies [76–78] a consistent 10% fraction of animals showed no bacteria in the dLN following id challenge with Y. pestis, while we detected bacteria in the dLN of all mice that had received Y. pseudotuberculosis cells in the ear pinna. This suggests that the bottleneck effect is linked to the loss of one or several Y. pseudotuberculosis function(s) involved in the access to lymphoid tissues, and that the acquisition of pPla did not fully restore the ability to overcome this effect.
In conclusion, this study unraveled pathophysiological relationships between components of the host response to Y. pestis infection and the role of pPla in this process. While high bacterial titers, tissue destructions and virulence were expected to be tightly linked, we show here that the extensive histological lesions observed in the bubo do not require Pla and are not associated with mortality. In contrast, bacterial loads in the dLN correlate with mortality and are Pla-dependent. However, achieving a high bacterial burden in the dLN is not sufficient for full pathogenicity. It has been proposed that Pla contribution to virulence was to catalytically break down protein barriers that would confine the bacteria and restrain their spread. However, since Pla is involved neither in the initial colonization of the organ nor in dLN destruction, this mechanism is unlikely to be essential for the development of the bubo. Our results show that achieving high bacterial burdens in the LN might be a critical step in plague pathogenesis and that one major role of Pla is to protect Y. pestis cells from the bactericidal action of the dLN environment.
Supporting Information
Zdroje
1. (2006) International meeting on preventing and controlling plague: the old calamity still has a future. Wkly Epidemiol Rec 81 : 278–284. 16841399
2. Stenseth NC, Atshabar BB, Begon M, Belmain SR, Bertherat E, et al. (2008) Plague: past, present, and future. PLoS Med 5: e3. doi: 10.1371/journal.pmed.0050003 18198939
3. Schrag SJ, Wiener P (1995) Emerging infectious diseases: what are the relative roles of ecology and evolution? Trends Evol Ecol 10 : 319–324.
4. Morens DM, Folkers GK, Fauci AS (2004) The challenge of emerging and re-emerging infectious diseases. Nature 430 : 242–249. 15241422
5. Pollitzer R (1954) Plague. WHO Monograph Series 22 World Health Organization, Geneva, Switzerland.
6. Perry RD, Fetherston JD (1997) Yersinia pestis—etiologic agent of plague. Clin Microbiol Rev 10 : 35–66. 8993858
7. Flexner S (1901) The pathology of bubonic plague. Am J Med Sci 122 : 396–416.
8. Crowell BC (1915) Pathologic anatomy of bubonic plague. The Philippine Journal of Science 10 B: 249–307.
9. Smith JH, Reisner BS (1997) Plague. In: Connor DH, editor. Pathology of infectious diseases. Stamford, CT: Prentice-Hall. pp. 729–738.
10. Dennis DT, Meier FA (1997) Plague. In: Horsburgh RC Jr, editor. Pathology of Emerging Infections. Washington, DC: American Society for Microbiology. pp. 21–47.
11. Sebbane F, Gardner D, Long D, Gowen BB, Hinnebusch BJ (2005) Kinetics of disease progression and host response in a rat model of bubonic plague. Am J Pathol 166 : 1427–1439. 15855643
12. Herzog M (1904) The Plague, Bacteriology, Morbid Anatomy, and Histopathology. Including a consideration of insects as plague carriers; Laboratories BoG, editor. Manila: Bureau of public printing. 1–149 p.
13. Prentice MB, Rahalison L (2007) Plague. Lancet 369 : 1196–1207. 17416264
14. Brubaker RR, Beesley ED, Surgalla MJ (1965) Pasteurella pestis: Role of Pesticin I and Iron in Experimental Plague. Science 149 : 422–424. 17809405
15. Welkos SL, Friedlander AM, Davis KJ (1997) Studies on the role of plasminogen activator in systemic infection by virulent Yersinia pestis strain C092. Microb Pathog 23 : 211–223. 9344782
16. Guinet F, Ave P, Jones L, Huerre M, Carniel E (2008) Defective Innate Cell Response and Lymph Node Infiltration Specify Yersinia pestis Infection. Plos One 3(2): e1688. doi: 10.1371/journal.pone.0001688 18301765
17. Achtman M, Zurth K, Morelli C, Torrea G, Guiyoule A, et al. (1999) Yersinia pestis, the cause of plague, is a recently emerged clone of Yersinia pseudotuberculosis. Proc Natl Acad Sci USA 96 : 14043–14048. 10570195
18. Smego RA, Frean J, Koornhof HJ (1999) Yersiniosis I: Microbiological and clinicoepidemiological aspects of plague and non-plague Yersinia infections [Review]. Eur J Clin Microbiol Infect Dis 18 : 1–15. 10192708
19. Carniel E, Autenrieth I, Cornelis G, Fukushima H, Guinet F, et al. (2006) Y. enterocolitica and Y. pseudotuberculosis; Dworkin MM, Falkow S, Rosenberg E, Schleifer K-H, Stackebrandt E, editors.
20. Une T, Brubaker RR (1984) In vivo comparison of avirulent Vwa - and Pgm - or Pstr phenotypes of yersiniae. Infect Immun 43 : 895–900. 6365786
21. Pouillot F, Derbise A, Kukkonen M, Foulon J, Korhonen TK, et al. (2005) Evaluation of O-antigen inactivation on Pla activity and virulence of Yersinia pseudotuberculosis harbouring the pPla plasmid. Microbiology 151 : 3759–3768. 16272397
22. Chain PS, Carniel E, Larimer FW, Lamerdin J, Stoutland PO, et al. (2004) Insights into the evolution of Yersinia pestis through whole-genome comparison with Yersinia pseudotuberculosis. Proc Natl Acad Sci USA 101 : 13826–13831. 15358858
23. Sodeinde OA, Subrahmanyam YVBK, Stark K, Quan T, Bao YD, et al. (1992) A surface protease and the invasive character of plague. Science 258 : 1004–1007. 1439793
24. Sebbane F, Jarrett CO, Gardner D, Long D, Hinnebusch BJ (2006) Role of the Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proc Natl Acad Sci USA 103 : 5526–5530. 16567636
25. Lathem WW, Price PA, Miller VL, Goldman WE (2007) A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science 315 : 509–513. 17255510
26. Lahteenmaki K, Kuusela P, Korhonen TK (2001) Bacterial plasminogen activators and receptors [Review]. FEMS Microbiol Rev 25 : 531–552. 11742690
27. Kukkonen M, Korhonen TK (2004) The omptin family of enterobacterial surface proteases/adhesins: from housekeeping in Escherichia coli to systemic spread of Yersinia pestis. Int J Med Microbiol 294 : 7–14. 15293449
28. Korhonen TK, Haiko J, Laakkonen L, Jarvinen HM, Westerlund-Wikstrom B (2013) Fibrinolytic and coagulative activities of Yersinia pestis. Front Cell Infect Microbiol 3 : 35. doi: 10.3389/fcimb.2013.00035 23898467
29. Galvan EM, Lasaro MAS, Schifferli DM (2008) Capsular antigen fraction 1 and pla modulate the susceptibility of Yersinia pestis to pulmonary antimicrobial peptides such as cathelicidin. Infect Immun 76 : 1456–1464. doi: 10.1128/IAI.01197-07 18227173
30. Caulfield AJ, Walker ME, Gielda LM, Lathem WW (2014) The Pla protease of Yersinia pestis degrades fas ligand to manipulate host cell death and inflammation. Cell Host Microbe 15 : 424–434. doi: 10.1016/j.chom.2014.03.005 24721571
31. Kienle Z, Emody L, Svanborg C, O'Toole PW (1992) Adhesive properties conferred by the plasminogen activator of Yersinia pestis. J Gen Microbiol 138 : 1679–1687. 1527508
32. Lahteenmaki K, Virkola R, Saren A, Emody L, Korhonen TK (1998) Expression of plasminogen activator Pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect Immun 66 : 5755–5762. 9826351
33. Cowan C, Jones HA, Kaya YH, Perry RD, Straley SC (2000) Invasion of epithelial cells by Yersinia pestis: evidence for a Y. pestis-specific invasin. Infect Immun 68 : 4523–4530. 10899851
34. Lahteenmaki K, Kukkonen M, Korhonen TK (2001) The Pla surface protease/adhesin of Yersinia pestis mediates bacterial invasion into human endothelial cells. FEBS Lett 504 : 69–72. 11522299
35. Zhang SS, Park CG, Zhang P, Bartra SS, Plano GV, et al. (2008) Plasminogen Activator Pla of Yersinia pestis Utilizes Murine DEC-205 (CD205) as a Receptor to Promote Dissemination. J Biol Chem 283 : 31511–31521. doi: 10.1074/jbc.M804646200 18650418
36. Felek S, Tsang TM, Krukonis ES (2010) Three Yersinia pestis Adhesins Facilitate Yop Delivery to Eukaryotic Cells and Contribute to Plague Virulence. Infect Immun 78 : 4134–4150. doi: 10.1128/IAI.00167-10 20679446
37. Lawrenz MB, Pennington J, Miller VL (2013) Acquisition of omptin reveals cryptic virulence function of autotransporter YapE in Yersinia pestis. Mol Microbiol 89 : 276–287. doi: 10.1111/mmi.12273 23701256
38. Sebbane F, Lemaitre N, Sturdevant DE, Rebeil R, Virtaneva K, et al. (2006) Adaptive response of Yersinia pestis to extracellular effectors of innate immunity during bubonic plague. Proc Natl Acad Sci U S A 103 : 11766–11771. 16864791
39. Kukkonen M, Suomalainen M, Kyllonen P, Lahteenmaki K, Lang H, et al. (2004) Lack of O-antigen is essential for plasminogen activation by Yersinia pestis and Salmonella enterica. Mol Microbiol 51 : 215–225. 14651623
40. Skurnik M, Peippo A, Ervela E (2000) Characterization of the O-antigen gene clusters of Yersinia pseudotuberculosis and the cryptic O-antigen gene cluster of Yersinia pestis shows that the plague bacillus is most closely related to and has evolved from Y. pseudotuberculosis serotype O:1b. Mol Microbiol 37 : 316–330. 10931327
41. Zheng L, Baumann U, Reymond JL (2004) An efficient one-step site-directed and site-saturation mutagenesis protocol. Nucleic Acids Res 32: e115. 15304544
42. Derbise A, Lesic B, Dacheux D, Ghigo JM, Carniel E (2003) A rapid and simple method for inactivating chromosomal genes in Yersinia. FEMS Immunol Med Microbiol 38 : 113–116. 13129645
43. Derbise A, Chenal-Francisque V, Pouillot F, Fayolle C, Prevost M - C, et al. (2007) A horizontally acquired filamentous phage contributes to the pathogenicity of the plague bacillus. Molecular microbiology 63 : 1145–1157. 17238929
44. Kukkonen M, Lahteenmaki K, Suomalainen M, Kalkkinen N, Emody L, et al. (2001) Protein regions important for plasminogen activation and inactivation of alpha(2)-antiplasmin in the surface protease Pla of Yersinia pestis. Mol Microbiol 40 : 1097–1111. 11401715
45. Guinet F, Carniel E (2003) A technique of intradermal injection of Yersinia to study Y. pestis physiopathology. Adv Exp Med Biol 529 : 73–78. 12756731
46. Van den Broeck W, Derore A, Simoens P (2006) Anatomy and nomenclature of murine lymph nodes: Descriptive study and nomenclatory standardization in BALB/cAnNCrl mice. J Immunol Methods 312 : 12–19. 16624319
47. Ferrero RL, Ave P, Radcliff FJ, Labigne A, Huerre MR (2000) Outbred mice with long-term helicobacter felis infection develop both gastric lymphoid tissue and glandular hyperplastic lesions [In Process Citation]. J Pathol 191 : 333–340. 10878557
48. Lang T, Ave P, Huerre M, Milon G, Antoine J (2000) Macrophage subsets harbouring Leishmania donovani in spleens of infected BALB/c mice: localization and characterization. Cellular Microbiology 2 : 415–430. 11207597
49. Armed Forced Institute of Pathology (1992) Laboratory Methods in Histotechnology.; Prophet EB, Mills B, Arrington JB, Sobin LH, editors. Washington, DC.
50. Buchrieser C, Prentice M, Carniel E (1998) The 102-kilobase unstable region of Yersinia pestis comprises a high-pathogenicity island linked to a pigmentation segment which undergoes internal rearrangement. J Bacteriol 180 : 2321–2329. 9573181
51. Degen JL, Bugge TH, Goguen JD (2007) Fibrin and fibrinolysis in infection and host defense. J Thromb Haemost 5 : 24–31. 17635705
52. Samoilova SV, Samoilova LV, Yezhov IN, Drozdov IG, Anisimov AP (1996) Virulence of pPst+ and pPst - strains of Yersinia pestis for guinea-pigs. J Med Microbiol 45 : 440–444. 8958247
53. Caulfield AJ, Lathem WW (2012) Substrates of the plasminogen activator protease of Yersinia pestis. Adv Exp Med Biol 954 : 253–260. doi: 10.1007/978-1-4614-3561-7_32 22782771
54. Swedberg JE, Harris JM (2012) Natural and engineered plasmin inhibitors: applications and design strategies. Chembiochem 13 : 336–348. doi: 10.1002/cbic.201100673 22238174
55. Bhattacharya S, Ploplis VA, Castellino FJ (2012) Bacterial plasminogen receptors utilize host plasminogen system for effective invasion and dissemination. J Biomed Biotechnol 2012 : 482096. doi: 10.1155/2012/482096 23118509
56. Fulde M, Steinert M, Bergmann S (2013) Interaction of streptococcal plasminogen binding proteins with the host fibrinolytic system. Front Cell Infect Microbiol 3 : 85. doi: 10.3389/fcimb.2013.00085 24319673
57. Vieira ML, Alvarez-Flores MP, Kirchgatter K, Romero EC, Alves IJ, et al. (2013) Interaction of Leptospira interrogans with human proteolytic systems enhances dissemination through endothelial cells and protease levels. Infect Immun 81 : 1764–1774. doi: 10.1128/IAI.00020-13 23478319
58. Mitra MM, Alizadeh H, Gerard RD, Niederkorn JY (1995) Characterization of a plasminogen activator produced by Acanthamoeba castellanii. Mol Biochem Parasitol 73 : 157–164. 8577323
59. Almeida L, Vanegas G, Calcagno M, Concepcion JL, Avilan L (2004) Plasminogen interaction with Trypanosoma cruzi. Mem Inst Oswaldo Cruz 99 : 63–67. 15057349
60. Stie J, Fox D (2012) Blood-brain barrier invasion by Cryptococcus neoformans is enhanced by functional interactions with plasmin. Microbiology 158 : 240–258. doi: 10.1099/mic.0.051524-0 21998162
61. Lahteenmaki K, Kuusela P, Korhonen TK (2000) Plasminogen activation in degradation and penetration of extracellular matrices and basement membranes by invasive bacteria. Methods 21 : 125–132. 10816373
62. Lahteenmaki K, Edelman S, Korhonen TK (2005) Bacterial metastasis: the host plasminogen system in bacterial invasion. Trends Microbiol 13 : 79–85. 15680767
63. Andreasen PA, Egelund R, Petersen HH (2000) The plasminogen activation system in tumor growth, invasion, and metastasis. Cell Mol Life Sci 57 : 25–40. 10949579
64. Lahteenmaki K, Virkola R, Pouttu R, Kuusela P, Kukkonen M, et al. (1995) Bacterial plasminogen receptors: in vitro evidence for a role in degradation of the mammalian extracellular matrix. Infect Immun 63 : 3659–3664. 7642304
65. Weiss SJ (1989) Tissue destruction by neutrophils. The New England journal of medicine 320 : 365–376. 2536474
66. Nathan C (2006) Neutrophils and immunity: challenges and opportunities. Nature Reviews Immunology 6 : 173–182. 16498448
67. Kolaczkowska E, Kubes P (2013) Neutrophil recruitment and function in health and inflammation. Nature Reviews Immunology 13 : 159–175. doi: 10.1038/nri3399 23435331
68. Hotchkiss RS, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, et al. (1999) Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Crit Care Med 27 : 1230–1251. 10446814
69. Lang JD, Matute-Bello G (2009) Lymphocytes, apoptosis and sepsis: making the jump from mice to humans. Crit Care 13 : 109. doi: 10.1186/cc7144 19216722
70. Giuliani A, Pirri G, Nicoletto SF (2007) Antimicrobial peptides: an overview of a promising class of therapeutics. Central European Journal of Biology 2 : 1–33.
71. Haiko J, Suomalainen M, Ojala T, Lahteenmaki K, Korhonen TK (2009) Breaking barriers—attack on innate immune defences by omptin surface proteases of enterobacterial pathogens. Innate Immun 15 : 67–80.
72. Thomassin JL, Brannon JR, Gibbs BF, Gruenheid S, Le Moual H (2012) OmpT outer membrane proteases of enterohemorrhagic and enteropathogenic Escherichia coli contribute differently to the degradation of human LL-37. Infect Immun 80 : 483–492. doi: 10.1128/IAI.05674-11 22144482
73. Le Sage V, Zhu L, Lepage C, Portt A, Viau C, et al. (2009) An outer membrane protease of the omptin family prevents activation of the Citrobacter rodentium PhoPQ two-component system by antimicrobial peptides. Mol Microbiol 74 : 98–111. doi: 10.1111/j.1365-2958.2009.06854.x 19708916
74. Derbise A, Chenal-Francisque V, Huon C, Fayolle C, Demeure CE, et al. (2010) Delineation and analysis of chromosomal regions specifying Yersinia pestis. Infect Immun 78 : 3930–3941. doi: 10.1128/IAI.00281-10 20605981
75. Zimbler DL, Schroeder JA, Eddy JL, Lathem WW (2015) Early emergence of Yersinia pestis as a severe respiratory pathogen. Nat Commun 6 : 7487. doi: 10.1038/ncomms8487 26123398
76. Gonzalez RJ, Lane MC, Wagner NJ, Weening EH, Miller VL (2015) Dissemination of a highly virulent pathogen: tracking the early events that define infection. PLoS Pathog 11: e1004587. doi: 10.1371/journal.ppat.1004587 25611317
77. Bosio CF, Jarrett CO, Gardner D, Hinnebusch BJ (2012) Kinetics of innate immune response to Yersinia pestis after intradermal infection in a mouse model. Infect Immun 80 : 4034–4045. doi: 10.1128/IAI.00606-12 22966041
78. Shannon JG, Hasenkrug AM, Dorward DW, Nair V, Carmody AB, et al. (2013) Yersinia pestis subverts the dermal neutrophil response in a mouse model of bubonic plague. MBio 4: e00170-00113.
Štítky
Hygiena a epidemiológia Infekčné lekárstvo Laboratórium
Článek TRIM21 Promotes cGAS and RIG-I Sensing of Viral Genomes during Infection by Antibody-Opsonized VirusČlánek Effector OspB Activates mTORC1 in a Manner That Depends on IQGAP1 and Promotes Cell ProliferationČlánek Fundamental Roles of the Golgi-Associated Aspartyl Protease, ASP5, at the Host-Parasite InterfaceČlánek Modulation of the Surface Proteome through Multiple Ubiquitylation Pathways in African Trypanosomes
Článok vyšiel v časopisePLOS Pathogens
Najčítanejšie tento týždeň
2015 Číslo 10- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Očkování proti virové hemoragické horečce Ebola experimentální vakcínou rVSVDG-ZEBOV-GP
- Koronavirus hýbe světem: Víte jak se chránit a jak postupovat v případě podezření?
-
Všetky články tohto čísla
- Expression of Concern: Misregulation of Underlies the Developmental Abnormalities Caused by Three Distinct Viral Silencing Suppressors in Arabidopsis
- Preparing for the Next Epidemic with Basic Virology
- Effectively Communicating the Uncertainties Surrounding Ebola Virus Transmission
- Translating Basic Research into Clinical Applications: Malaria Research at an NIH Lab
- A Gut Odyssey: The Impact of the Microbiota on Spore Formation and Germination
- Papillomavirus E6 Oncoproteins Take Common Structural Approaches to Solve Different Biological Problems
- Chronobiomics: The Biological Clock as a New Principle in Host–Microbial Interactions
- Dimensions of Horizontal Gene Transfer in Eukaryotic Microbial Pathogens
- Addressing the Complications of Ebola and Other Viral Hemorrhagic Fever Infections: Using Insights from Bacterial and Fungal Sepsis
- Time for Chocolate: Current Understanding and New Perspectives on Cacao Witches’ Broom Disease Research
- Ganglioside and Non-ganglioside Mediated Host Responses to the Mouse Polyomavirus
- Crosslinking of a Peritrophic Matrix Protein Protects Gut Epithelia from Bacterial Exotoxins
- Structure Elucidation of Coxsackievirus A16 in Complex with GPP3 Informs a Systematic Review of Highly Potent Capsid Binders to Enteroviruses
- CD39 Expression Identifies Terminally Exhausted CD8 T Cells
- Abiotic Stresses Antagonize the Rice Defence Pathway through the Tyrosine-Dephosphorylation of OsMPK6
- Dissociation of Tissue Destruction and Bacterial Expansion during Bubonic Plague
- Interferon-γ: The Jekyll and Hyde of Malaria
- CCR2 Inflammatory Dendritic Cells and Translocation of Antigen by Type III Secretion Are Required for the Exceptionally Large CD8 T Cell Response to the Protective YopE Epitope during Infection
- A New Glycan-Dependent CD4-Binding Site Neutralizing Antibody Exerts Pressure on HIV-1
- The Suramin Derivative NF449 Interacts with the 5-fold Vertex of the Enterovirus A71 Capsid to Prevent Virus Attachment to PSGL-1 and Heparan Sulfate
- Trans-generational Immune Priming Protects the Eggs Only against Gram-Positive Bacteria in the Mealworm Beetle
- Peripheral Vγ9Vδ2 T Cells Are a Novel Reservoir of Latent HIV Infection
- Respiratory Syncytial Virus Disease Is Mediated by Age-Variable IL-33
- TRIM21 Promotes cGAS and RIG-I Sensing of Viral Genomes during Infection by Antibody-Opsonized Virus
- Modeling the Effects of Vorinostat Reveals both Transient and Delayed HIV Transcriptional Activation and Minimal Killing of Latently Infected Cells
- Identification of a Novel Lipoprotein Regulator of Spore Germination
- Calcium Regulation of Hemorrhagic Fever Virus Budding: Mechanistic Implications for Host-Oriented Therapeutic Intervention
- Antigen-Specific Th17 Cells Are Primed by Distinct and Complementary Dendritic Cell Subsets in Oropharyngeal Candidiasis
- Comparative Life Cycle Transcriptomics Revises Genome Annotation and Links a Chromosome Duplication with Parasitism of Vertebrates
- The Autophagy Receptor TAX1BP1 and the Molecular Motor Myosin VI Are Required for Clearance of Salmonella Typhimurium by Autophagy
- Carcinogenic Parasite Secretes Growth Factor That Accelerates Wound Healing and Potentially Promotes Neoplasia
- Effector OspB Activates mTORC1 in a Manner That Depends on IQGAP1 and Promotes Cell Proliferation
- Dengue Virus Infection of Requires a Putative Cysteine Rich Venom Protein
- Distinct Viral and Mutational Spectrum of Endemic Burkitt Lymphoma
- Fundamental Roles of the Golgi-Associated Aspartyl Protease, ASP5, at the Host-Parasite Interface
- Phenotypic and Functional Alterations in Circulating Memory CD8 T Cells with Time after Primary Infection
- Systematic Identification of Cyclic-di-GMP Binding Proteins in Reveals a Novel Class of Cyclic-di-GMP-Binding ATPases Associated with Type II Secretion Systems
- Influenza Transmission in the Mother-Infant Dyad Leads to Severe Disease, Mammary Gland Infection, and Pathogenesis by Regulating Host Responses
- Myeloid Cell Arg1 Inhibits Control of Arthritogenic Alphavirus Infection by Suppressing Antiviral T Cells
- The White-Nose Syndrome Transcriptome: Activation of Anti-fungal Host Responses in Wing Tissue of Hibernating Little Brown Myotis
- Influenza Virus Reassortment Is Enhanced by Semi-infectious Particles but Can Be Suppressed by Defective Interfering Particles
- Identification of the Mechanisms Causing Reversion to Virulence in an Attenuated SARS-CoV for the Design of a Genetically Stable Vaccine
- Differentiation-Dependent KLF4 Expression Promotes Lytic Epstein-Barr Virus Infection in Epithelial Cells
- The Histone Acetyltransferase Hat1 Regulates Stress Resistance and Virulence via Distinct Chromatin Assembly Pathways
- C-di-GMP Regulates Motile to Sessile Transition by Modulating MshA Pili Biogenesis and Near-Surface Motility Behavior in
- Modulation of the Surface Proteome through Multiple Ubiquitylation Pathways in African Trypanosomes
- Crystal Structure of the Human Cytomegalovirus Glycoprotein B
- Depletion of . GlmU from Infected Murine Lungs Effects the Clearance of the Pathogen
- Immunologic Control of Papillomavirus Type 1
- Requires Host Rab1b for Survival in Macrophages
- Structure Analysis Uncovers a Highly Diverse but Structurally Conserved Effector Family in Phytopathogenic Fungi
- PD-L1 Expression on Retrovirus-Infected Cells Mediates Immune Escape from CD8 T Cell Killing
- Phospho-dependent Regulation of SAMHD1 Oligomerisation Couples Catalysis and Restriction
- IL-4 Induced Innate CD8 T Cells Control Persistent Viral Infection
- Crystal Structures of a Piscine Betanodavirus: Mechanisms of Capsid Assembly and Viral Infection
- BCG Skin Infection Triggers IL-1R-MyD88-Dependent Migration of EpCAM CD11b Skin Dendritic cells to Draining Lymph Node During CD4+ T-Cell Priming
- Antigenic Characterization of the HCMV gH/gL/gO and Pentamer Cell Entry Complexes Reveals Binding Sites for Potently Neutralizing Human Antibodies
- Rescue of a Plant Negative-Strand RNA Virus from Cloned cDNA: Insights into Enveloped Plant Virus Movement and Morphogenesis
- Geminivirus Activates to Accelerate Cytoplasmic DCP2-Mediated mRNA Turnover and Weakens RNA Silencing in
- Disruption of Sphingolipid Biosynthesis Blocks Phagocytosis of
- The Fungal Exopolysaccharide Galactosaminogalactan Mediates Virulence by Enhancing Resistance to Neutrophil Extracellular Traps
- The Timing of Stimulation and IL-2 Signaling Regulate Secondary CD8 T Cell Responses
- Structural and Functional Analysis of Murine Polyomavirus Capsid Proteins Establish the Determinants of Ligand Recognition and Pathogenicity
- The Dual Role of an ESCRT-0 Component HGS in HBV Transcription and Naked Capsid Secretion
- PLOS Pathogens
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Chronobiomics: The Biological Clock as a New Principle in Host–Microbial Interactions
- Interferon-γ: The Jekyll and Hyde of Malaria
- Crosslinking of a Peritrophic Matrix Protein Protects Gut Epithelia from Bacterial Exotoxins
- Antigen-Specific Th17 Cells Are Primed by Distinct and Complementary Dendritic Cell Subsets in Oropharyngeal Candidiasis
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



