-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Bacillus Calmette-Guerin Infection in NADPH Oxidase Deficiency: Defective Mycobacterial Sequestration and Granuloma Formation
The vaccine Mycobacterium bovis BCG is administrated to prevent early age tuberculosis in endemic areas. BCG is a live vaccine with a low incidence of complications. However, local or disseminated BCG infection may occur, in particular in immunodeficient individuals. Chronic granulomatous disease (CGD), a deficiency in the superoxide-producing phagocyte NADPH oxidase, is a primary immune deficiency and one of the most frequent congenital defects of phagocyte in humans. Here we analyze the role of the phagocyte NADPH oxidase NOX2 in the defense against BCG. An extensive literature review suggested that BCG infection is by far the most common mycobacterial disease in CGD patients (220 published cases). We therefore studied BCG infection in several CGD mouse models showing that these were highly susceptible to BCG infection with a mortality rate of ∼50%. As compared to the wild type, CGD mice showed a markedly increased release of cytokines, an altered granuloma structure, and were unable to restrain mycobacteria within granulomas. Rescue of the phagocyte NADPH oxidase in macrophages was sufficient to protect mice from BCG infection and to sequester the mycobacteria within granulomas. Thus, superoxide generation by macrophages plays an important role for the defense against BCG infection and prevents overshooting release of proinflammatory cytokines.
Published in the journal: Bacillus Calmette-Guerin Infection in NADPH Oxidase Deficiency: Defective Mycobacterial Sequestration and Granuloma Formation. PLoS Pathog 10(9): e32767. doi:10.1371/journal.ppat.1004325
Category: Research Article
doi: https://doi.org/10.1371/journal.ppat.1004325Summary
The vaccine Mycobacterium bovis BCG is administrated to prevent early age tuberculosis in endemic areas. BCG is a live vaccine with a low incidence of complications. However, local or disseminated BCG infection may occur, in particular in immunodeficient individuals. Chronic granulomatous disease (CGD), a deficiency in the superoxide-producing phagocyte NADPH oxidase, is a primary immune deficiency and one of the most frequent congenital defects of phagocyte in humans. Here we analyze the role of the phagocyte NADPH oxidase NOX2 in the defense against BCG. An extensive literature review suggested that BCG infection is by far the most common mycobacterial disease in CGD patients (220 published cases). We therefore studied BCG infection in several CGD mouse models showing that these were highly susceptible to BCG infection with a mortality rate of ∼50%. As compared to the wild type, CGD mice showed a markedly increased release of cytokines, an altered granuloma structure, and were unable to restrain mycobacteria within granulomas. Rescue of the phagocyte NADPH oxidase in macrophages was sufficient to protect mice from BCG infection and to sequester the mycobacteria within granulomas. Thus, superoxide generation by macrophages plays an important role for the defense against BCG infection and prevents overshooting release of proinflammatory cytokines.
Introduction
M. bovis BCG (Bacillus Calmette Guérin) is an attenuated strain of M. bovis, used as a vaccine against tuberculosis. BCG vaccination has a proven efficacy only early in life (<1 year of age), in particular against tuberculous meningitis and miliary tuberculosis. Thus, the WHO recommends vaccination of newborns in endemic areas [1]. However, BCG is a live vaccine, which may persist and become a pathogen. In some individuals, in particular those with immune defects, BCG vaccination may lead to severe local or to disseminated infection [2], [3]. BCG is also used as local treatment for bladder cancer [4], where in some cases it may lead to symptomatic infection, from cystitis to life threatening dissemination [5]. However, there is emerging evidence for increased risk of BCG infection in patients lacking the phagocyte NADPH oxidase (chronic granulomatous disease, CGD) [6]–[8]. Indeed studies looking at underlying risk factors in patients presenting BCG infection suggest that approximately 20% of such patients suffer from CGD [9] and in many instances, BCG infection is the first manifestation of CGD [10].
The phagocyte NADPH oxidase NOX2 is a superoxide producing enzyme, involved in the host defense against numerous bacteria and fungi. Genetic loss of function of NOX2 is a primary immunodeficiency referred as chronic granulomatous disease (CGD). CGD may be caused by mutations in the gp91phox/NOX2 protein which is coded by the Cybb gene or one of its subunits, in particular p47phox, which is coded by the Ncf1 gene [11]. CGD patients suffer from severe and recurrent bacterial and fungal infections as well as from hyperinflammatory and autoimmune diseases in particular discoid lupus [12]. Until about 10 years ago, it was thought that the phagocyte NADPH oxidase was not relevant for the defense against mycobacteria [13]. Whether mice carrying CGD mutations show an increased susceptibility to infection with Mycobacterium tuberculosis remains controversial [14], while their susceptibility to BCG infection has so far not been studied.
Host defense mechanisms against mycobacteria are typically initiated by phagocytosis through macrophages, inducing inflammation and subsequently cell-mediated immunity involving Th1-type immune responses. These coordinated mechanisms result in granuloma formation. Granulomas are highly organized structures generated by interactions between myeloid and lymphoid cells that characterize the adaptive immune response to mycobacteria. In general granulomas sequester mycobacteria and thereby limit their dissemination. Granulomas are formed through cellular recruitment and are associated with production of cytokines and chemokines [15]. Among these cytokines, TNF and IFN-γ are the main players contributing to activation of macrophage host defense mechanisms [16]. Neutrophils are able to kill mycobacteria in vitro, but the in vivo relevance of neutrophils in the mycobacterial host defense remains a matter of debate [17].
Here we have first analyzed the relevance of BCG infection in CGD patients and then investigated the role of NADPH oxidase-generated ROS in experimental BCG infection. Mice lacking a functional phagocyte NADPH oxidase showed a markedly enhanced severity to BCG infection. Rescue of phagocyte NADPH oxidase function in macrophages was sufficient to reverse the phenotype to the mild disease observed in wild-type mice. We identified increased cytokine generation and poorly organized granuloma formation as mechanisms involved in the exacerbated severity of BCG infection in NADPH oxidase-deficient mice.
Results
To understand the relevance of mycobacterial infections for CGD patients, we performed an extensive review of the existing studies and case reports on this topic. A previous literature-based study from 1971 to 2006 reported 72 cases [6]; here we report a total of 297 cases of mycobacterial infections in CGD patients [6], [8], [9], [18]–[23]. M. bovis BCG infection was by most frequently reported (74%; i.e. 220 cases); 20% of cases were caused by Mycobacterium tuberculosis infection, and the rest by different nontuberculous mycobacteria (Fig. 1A). Most of the BCG cases were local or regional infections (BCG-itis). Relatively little information was found on the treatment and the outcome of these local infections, however one article mentions the necessity for surgical excision [6]. However, systemic BCG infections (BCG-osis) in CGD patients were not uncommon (31 cases; Fig. 1B). In 6 of the 31 cases, the outcome has been documented: 3 of the patients died and 3 of the patients survived [6], [24]–[28].
Fig. 1. Analysis of published cases of mycobacterial infections in CGD patients. 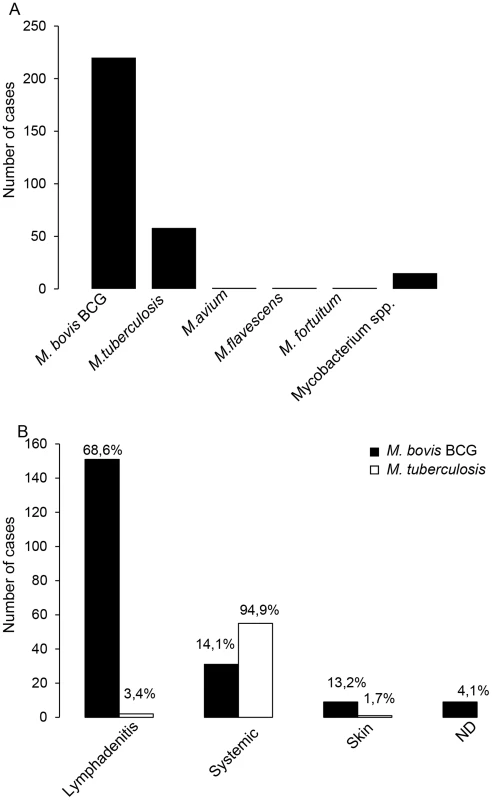
Our literature research identified a total of 297 published cases of mycobacterial disease in CGD patients. (A) Mycobacterial species recovered in mycobacterial disease in CGD patients. (B) Clinical presentations of Mycobacterium bovis BCG and Mycobacterium tuberculosis infections in CGD patients. The numbers indicated on top of each column represent the percentage with respect to the total number of BCG or M. tuberculosis cases, respectively. The terms “systemic” refers to disseminated or to lung infections. We therefore studied BCG infection in CGD mouse models. To exclude epistatic effects, we investigated different types of CGD mice (Ncf1 mutants, Cybb-knock-out mice), as well as different genetic backgrounds (C57Bl/10.Q, C57Bl/6). Taken together, the following mouse lines were used:
-
wild-type C57Bl/10.Q and C57Bl/6 mice.
-
Ncf1 mutant mice with a loss of function mutation in the p47phox subunit of the phagocyte NADPH oxidase (genetic background: C57Bl/10.Q; [29], [30]). The intronic point mutation in the Ncf1 gene generates spliced variants. Only a truncated protein, which fails to activate NOX2 is expressed [30].
-
Ncf1 mutant mice with a transgenic rescue of the Ncf1 gene under the control of a CD68 promoter. These mice express a wild-type Ncf1/p47phox protein in macrophages and dendritic cells, but not in neutrophils and are referred to as Ncf1 rescue mice (genetic background: C57Bl/10.Q) [31], [32].
-
Ncf1 mutant mice with C57Bl/6 background.
-
Cybb-deficient mice with C57Bl/6 background [33].
ROS production in mononuclear phagocytes limits severity of BCG infection
Mice were injected intravenously with BCG (107 CFU). Wild-type mice resisted the infection during the 4 week observation. In contrast, Ncf1 mutant mice showed early mortality: 50% of mice died after 10 days and only 33% of the mice survived after 4 weeks (Figure 2A). The high mortality of Ncf1 mutant mice was associated with a rapid weight loss, which was absent in wild-type controls (Figure 2B). To investigate whether the genetic background or the type of CGD mutation was responsible for the high susceptibility, we investigate other types of CGD mice. BCG-infected Ncf1 mutant mice in a C57Bl/6 background showed also a higher mortality as compared with their wild-type controls (Figure 2C). Similarly to Ncf1 mutant mice in C57Bl/10.Q background, Ncf1 mutant mice in a C57Bl/6 background showed a rapid weight loss (Figure 2D). However the median survival time was around 20 days in the C57Bl/6 background, as opposed to ∼8 days in the C57Bl/10.Q background which suggest a contribution of the mouse genetic background to BCG susceptibility. Given that the survival trends in the different genetic backgrounds appeared to be similar, suggesting a minor role for epistasis and a major role of the NOX2 subunit mutation, BCG infection was studied in Ncf1 rescue mice that we have previously characterized [31], [32]. Ncf1 rescue as wild-type mice resisted the infection during the 4 weeks observation and no mortality or no important weight loss was observed (Figure 2A and B). Finally, BCG infection in Cybb-deficient mice also led to a high mortality and weight loss as compared to wild type controls (Figure 2E and F). These observations strongly suggest that in absence of ROS production by NADPH oxidase (see below), mice are more susceptible to mycobacterial infection. Furthermore, the normal survival of Ncf1 rescue mice implies that ROS production in mononuclear phagocytes is crucial.
Fig. 2. Impact of CGD mutation on mortality and weight loss in response to BCG infection. 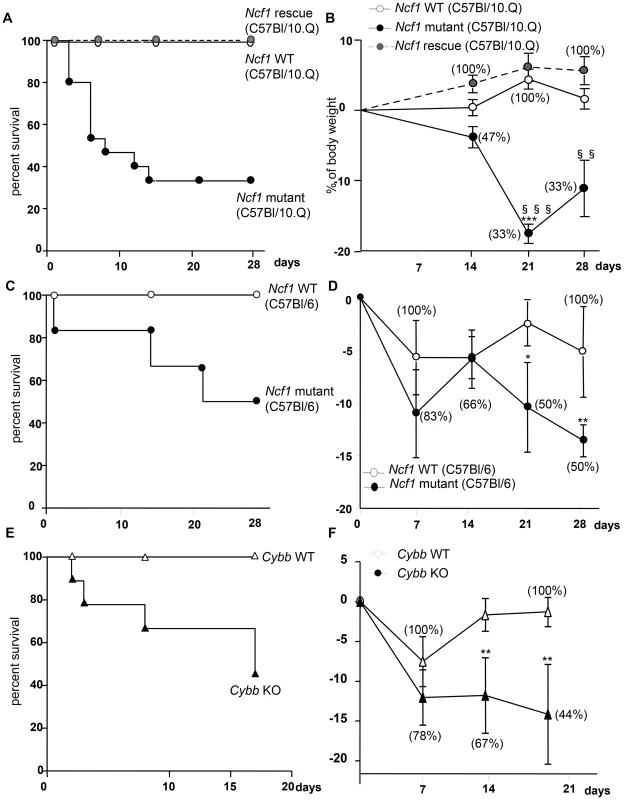
Ncf1 mutant (loss of function mutation in p47phox), Ncf1 rescue (expression of wild-type p47phox in mononuclear phagocytes) with C57Bl/10.Q background, Ncf1 mutant (loss of function mutation in p47phox) with C57Bl/6 background, Cybb-deficient and their respective wild-type controls were injected intravenously with BCG (107 CFU). Survival was monitored over the 4 weeks period following BCG inoculation in (A) C57Bl/10.Q wild-type (n = 15), Ncf1 mutant (n = 15) and Ncf1 rescue (n = 11), in (C) C57Bl/6 wild-type (n = 7), Ncf1 mutant (n = 6) and (E) C57Bl/6 wild-type (n = 7), Cybb-deficient (n = 9) mice. (B, D and F) Body weight changes as a function of time after BCG inoculation. Survival (percent of initial number of mice) is shown in brackets. Statistics shown in the figures are the comparison between respective wild-type and Ncf1 mutant or Cybb-deficient (***: p<0.001, **: p<0.05, *: p<0.01) and the comparison between Ncf1 mutant and rescue (§§§: p<0.001 and §§: p<0.01). Note that no significant differences were observed between wild-type and Ncf1 rescue mice. Severe pulmonary lesions after BCG inoculation in the phagocyte NADPH oxidase-deficient mice
To further understand the causes of the early mortality of Ncf1 mutant mice, mice were sacrificed at day 3 post-infection for lung histopathological examination. In the absence of BCG infection, no histological differences were observed between wild-type, Ncf1 mutant and rescue mice (Figure S1). However, upon BCG infection, Ncf1 mutant mice presented severe inflammatory lesions in the lungs with extended hemorrhagic lesions, intravascular thrombosis, decrease of the alveolar spaces (Figure 3A.b) and hypertrophy of pleural cells (Figure 3B.b). Ncf1 mutant mice also showed accumulation of inflammatory cells composed essentially by neutrophils concentrated as microabscesses (Figure 3A.e). In contrast, wild-type and Ncf1 rescue did not show massive hemorrhagic lesions and only moderate inflammation with mixed inflammatory cells observed in lungs (Figures 3A.a, c, d and f).
Fig. 3. Ncf1 mutation leads to severe lung damage in response to BCG infection. 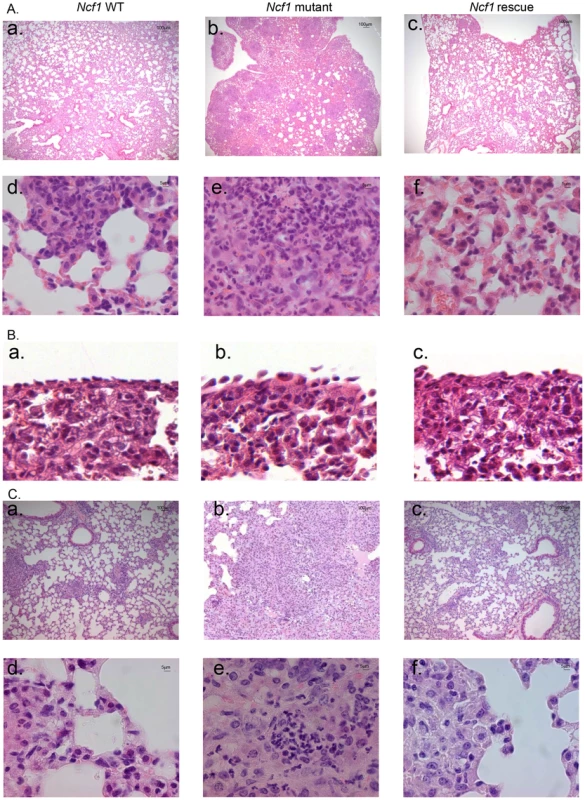
Hematoxylin and eosin-stained lung sections taken from mice sacrificed after 3 days (A, B) or 4 weeks (C) of BCG infection. (A, C) representative sections from wild-type (a and d), Ncf1 mutant (b and e) and Ncf1 rescue (c and f) mice. (B) Pleural histology from wild-type (a), Ncf1 mutant (b) and Ncf1 rescue (c) mice sacrificed 3 days after BCG infection. Magnifications were ×200 (panels A a–c and C a–c) and ×1000 (panels A d–f and C d–f) and ×600 (panel B). The surviving Ncf1 mutant mice (5 out of 15) were also analyzed at 4 weeks post-infection. Histopathological examination of Ncf1 mutant lungs revealed extensive inflammatory lesions reducing notably the alveolar space (Figure 3C.b) and microabscesses composed of neutrophils. Only one third of the Ncf1 mutant mice survived up to 4 weeks and the latter results might represent a survivor effect, and not necessarily be representative for all Ncf1 mutant mice. In contrast, wild-type and Ncf1 rescue did not show massive infiltrate of inflammatory cells (Figures 3C.a–c and d–f).
In the absence of BCG infection, the organ weight indexes for lung, liver and spleen were comparable in all mouse strains (Figure 4A and Figure S1). After BCG infection, lung weight, as a surrogate measure of lung inflammation and edema, increased only moderately in wild-type and Ncf1 rescue mice, but massively in Ncf1 mutant mice (Figure 4A). At 4 weeks of BCG infection, the severity of lung pathology was also assessed by analysis of free alveolar space vs. occupied space. The occupied space was significantly increased in Ncf1 mutant as compared to wild-type and Ncf1 rescue lungs (Figure 4B). This quantification corroborates with the massive obstruction of alveolar space in Ncf1 mutant mice seen in histology. Similar as seen for Ncf1 mutant mice, BCG-infected Cybb-deficient mice showed severe inflammatory lesions with extended hemorrhagic lesions and decreased alveolar space (Figure S2.A and B.b). Microabscesses of neutrophils were also present in Cybb-deficient and Ncf1 mutant in C57Bl/6 background in the lung of both sacrificed and deceased mouse while mixed inflammatory cells were observed in Ncf1 rescue and wild-type lungs (Figure S2.B.d and C). The lung weight was also increased in Cybb-deficient and Ncf1 mutant in C57Bl/6 background mice compared to wild-type, 4 weeks after BCG infection (Figure S4.A). In summary, these data support that impaired ROS production by mononuclear phagocytes is associated with increased inflammatory response involving neutrophilic microabscess formation following BCG infection.
Fig. 4. Lung parameters in response to BCG infection. 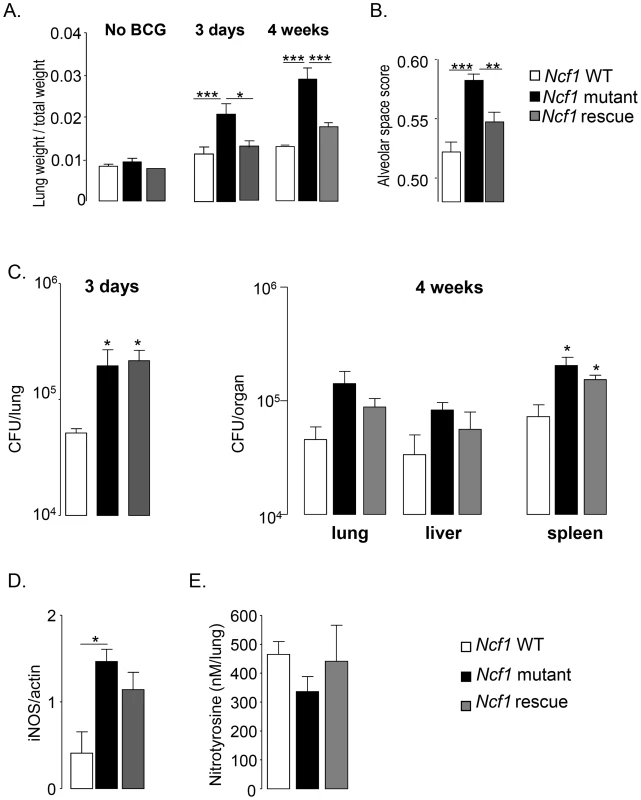
(A) Lung/weight ratio of wild-type (n = 9), Ncf1 mutant (n = 5) and Ncf1 rescue (n = 8) mice without BCG infection and at 3 days and 4 weeks post infection. (B) Determination of alveolar space score (occupied lung tissue vs. free space) in lung sections at 4 weeks post infection. Data are represented as the mean of alveolar space score ± SD in 4 mice per group with at least 3 lobes analyzed per mouse. (C) Number of viable bacteria was determined at 3 days and 4 weeks following BCG infection. Data are shown as mean log of CFU per organ (±SEM; 3–5 mice per group). (D) iNOS protein expression in lung was detected by western blot 4 weeks after BCG infection. Results are expressed as mean ± SEM of relative units of iNOS/actin (n = 4, per group) after quantification by Image Quant software. (E) Nitrotyrosine quantification by ELISA was done in lungs, 4 weeks after BCG infection. Results are expressed as mean ± SEM of nM per lung (n = 4–5, per group). (***: p<0.001, **: p<0.05, *: p<0.01). Bacterial counts and iNOS activation upon BCG infection
To evaluate mechanisms how ROS production protect from death by BCG infection, we assessed bacterial burden by colony forming unit quantification in different organs. Bacterial load in the lung of both the Ncf1 mutant and Ncf1 rescue mice were similar but higher than those in wild-type mice 3 days after infection (Figure 4C). Four weeks post-infection, no significant differences in bacterial load were observed in lung and liver. However, bacterial counts in the spleen of Ncf1mutant and Ncf1rescue mice were significantly increased compared to wild-type (Figure 4C). We further evaluated inducible nitric oxide synthase iNOS by western blot, which is crucial for clearance of BCG and mouse survival [34]. Expression of iNOS protein in the lung at 4 weeks post-infection was significantly increased in Ncf1 mutant as compared to wild-type mice (Figure 4D). NO and superoxide form peroxynitrite, a highly reactive molecule, are implicated in mycobacteria killing. Upon interaction with proteins, peroxynitrite produces nitrotyrosine, which are stable biological peroxynitrite markers [35]. Interestingly, despite the increase of iNOS protein, nitrotyrosine levels measured by ELISA in lungs of Ncf1 mutant were not different from wild-type (Figure 4D), presumably because Ncf1 mutant mice lack the second substrate required for peroxynitrite generation, namely superoxide. Thus, most likely CGD mice produce increased amounts of NO in response to mycobacteria, but given the lack of NOX2-generated superoxide, this is not accompanied by an increase in peroxynitrite. These results are compatible with the concept that peroxynitrite, rather than NO or ROS, is crucial for optimal mycobacterial killing.
Cytokine and chemokine levels activated by BCG infection
We next measured levels of selected cytokines by ELISA in lung homogenates from BCG infected mice (Figures 5). Three days post infection, the increase of TNF levels in Ncf1 mutant lung was massive (3.6-fold compared to wild-type) and also observed at four weeks post-infection (Figure 5A). TNF levels in Ncf1 rescue lung were comparable to those observed in wild-type lung. Three days, but not 4 weeks, post infection, IL-17 lung levels were increased in Ncf1 mutant mice (Figure 5B). The same pattern was observed for IL-12p40 (Figure 5C). The pattern was slightly different for IFN-γ: there were increased in Ncf1 mutant mice at 3 days and 4 weeks post-infection, however Ncf1 rescue mice showed even higher IFN-γ levels 4 weeks post-infection (Figure 4D). We also assessed the levels of the chemokines CXCL1 (KC, the murine IL-8 homolog), and CCL5 (RANTES). We selected CXCL1 because it is a powerful neutrophil chemoattractant [36] and might explain the high number of neutrophils in the lung lesion in mutant mice and CCL5 because it is a leukocyte chemoattractant with a role in mycobacterial protection [37]. Ncf1 mutant mice showed a higher CXCL1 levels 3 days after BCG infection (Figure 5E). CCL5 levels were increased in Ncf1 mutant mice three days and 4 weeks after infection (Figure 5F). The general pattern was an increase in pulmonary cytokine and chemokine responses in Ncf1 mutant mice due to the infection which was controlled by Ncf1 rescue mice. Moreover, we also evaluated if Cybb-deficient mice would also respond with an exacerbated cytokine response using ex-vivo recall of spleen cells from BCG infected mice. Both re-infection of splenocytes or addition of BCG antigens resulted in enhanced TNF and nitrite, as an indicator of NO production, evaluated respectively by ELISA and Griess reagent, confirming that NOX2 deficiency leads to an increase response in TNF and immune mediators (Figure S3). Thus, at early time points a massive increase of pro-inflammatory cytokines was observed in BCG-infected CGD mice. At later time points, only TNF and CCL5 levels remained elevated, this had a probable importance for altered granuloma formation (see below).
Fig. 5. Cytokine and chemokine responses to BCG infection. 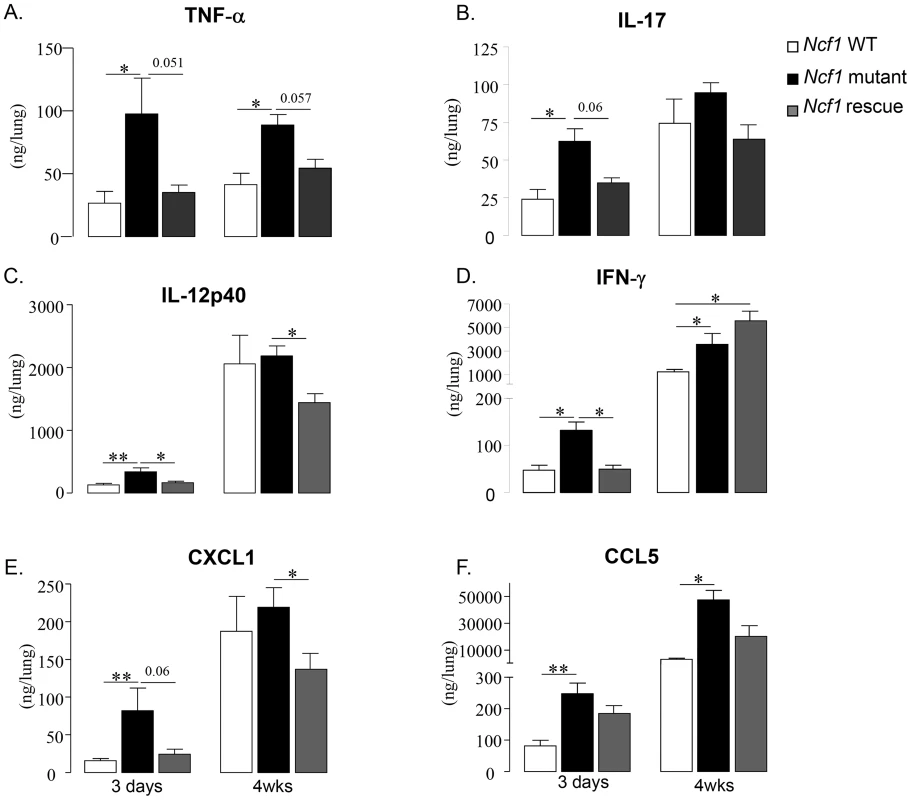
TNF-α (A), IL-17 (B), IL-12p40 (C), IFN-γ (D), CXCL1 (E) and CCL5 (F) were assessed in lung homogenates obtained 3 days and 4 weeks after BCG infection. Results are presented as the mean ± SEM (n = 4–7 mice per group). (**: p<0.05, *: p<0.01). ROS generation in mononuclear cells and in granulomas from Ncf1 rescue mice
We have previously demonstrated that ROS production in response to phorbol myristate acetate (PMA) or β-glucan was abolished in neutrophils, bone-marrow derived macrophages (BMDM) and dendritic cells (BMDC) in Ncf1 mutant mice [29]. We therefore investigated ROS production measured by amplex red in BMDM and BMDC exposed to BCG. Wild-type and Ncf1 rescue cells produced ROS in response to BCG, but not Ncf1 mutant cells (Figures 6A, B). Diphenylene iodonium (DPI), a non-specific NOX inhibitor, abolished the mycobacteria-induced ROS production in wild-type and Ncf1 rescue cells. The kinetic of ROS production was comparable in BMDM and BMDC from wild-type and Ncf1 rescue mice (Figures 6A and B).
Fig. 6. ROS generation in response to BCG in vitro and in vivo. 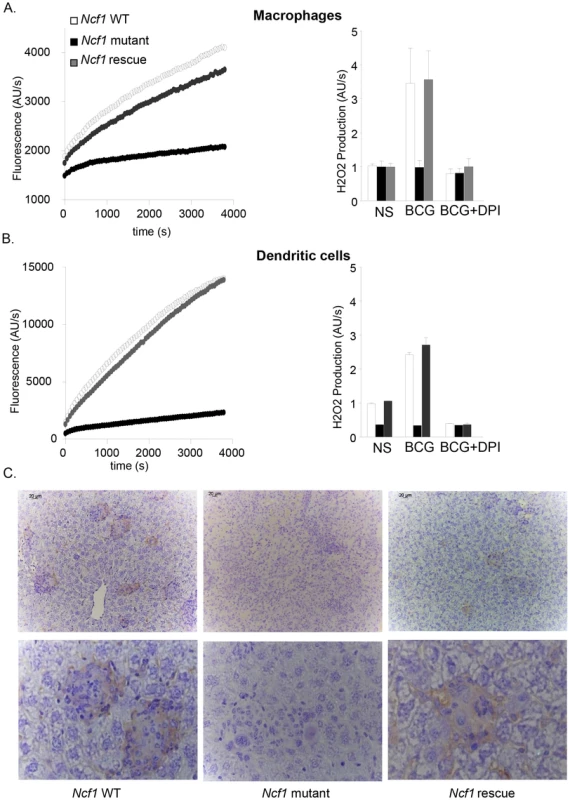
(A) Bone marrow-derived macrophages and (B) dendritic cells were obtained from wild-type, Ncf1 mutant and Ncf1 rescue mice. H2O2 release was measured by Amplex red. Left panels: Cells were stimulated with BCG. Representative kinetic graphs of ROS production as measured by fluorescence emission. Right panels: Cells were exposed to PBS (NS) or BCG; where indicated, the inhibitor DPI was added. Histograms representing ROS production of three independent experiments performed in duplicate (mean ± SEM). (C) Representative images of immunohistochemistry for 8-hydroxy-2′-deoxyguanosine (8-OHdG) in liver sections from wild-type, Ncf1 mutant and rescue mice obtained 4 weeks post infection. Magnifications were ×200 (upper panel C) and ×1000 (lower panel). We next investigated whether there are signs of ROS production in granulomas in vivo. For this purpose, liver sections from 4 weeks BCG-infected mice were stained with an antibody against 8-OHdG (8-hydroxydeoxyguanosine), a well-studied marker of DNA oxidation [38]. In wild-type and Ncf1 rescue liver, an important 8-OHdG staining was observed within granulomas (Figure 6C). Note that, to the best of our knowledge, this is the first demonstration of ROS generation during granuloma formation. Importantly, no 8-OHdG staining was observed in granulomas of Ncf1 mutant mice, demonstrating that the phagocyte NADPH oxidase is the major source of ROS during BCG infection.
Phagocyte NADPH oxidase in mononuclear phagocytes contributes to granuloma formation and sequestration of mycobacteria
Granuloma formation is a crucial mechanism to control mycobacterial infection. To determine the relationship between ROS production and granuloma formation, we next analyzed lung histology 3 days and 4 weeks after BCG infection using the following stainings: H/E (general morphology), Ziehl-Neelsen (mycobacteria), acidic phosphatase activity (activated macrophages). Three days post BCG infection, lung sections from wild-type and Ncf1 rescue mice showed clusters of macrophages (Figure 7A). In Ncf1 mutant mice, BCG infection induced abundant neutrophil abscesses, with a lack of macrophage clustering within restricted areas (Figure 7B). Mycobacteria appeared less abundant in lung section from wild-type as compared to Ncf1 mutant mice (Figure 7C). Interestingly, the Ziehl-Neelsen stain suggests a relatively high bacterial load in rescue mice, corroborating the quantitative bacterial load analysis (Figure 4C).
Fig. 7. Role of the phagocyte NADPH oxidase in granuloma formation and BCG sequestration. 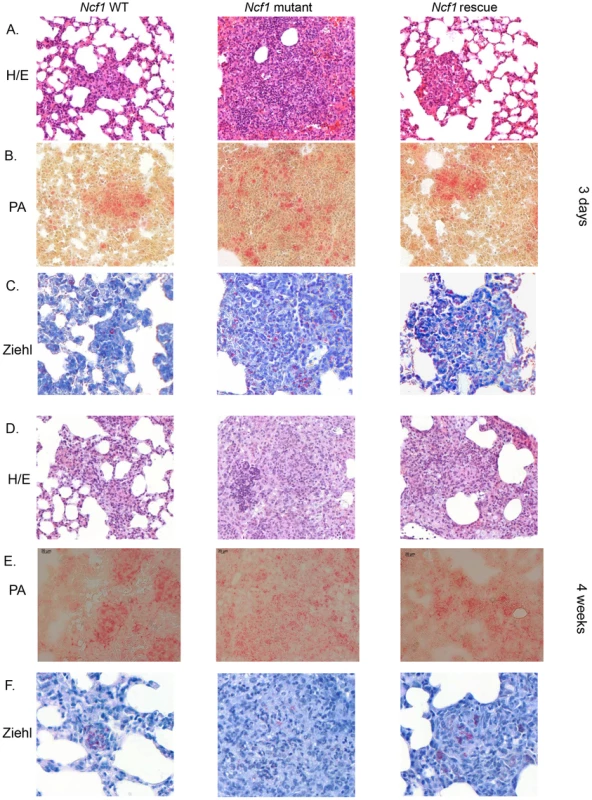
Three days and 4 weeks after BCG infection, wild-type, Ncf1mutant and rescue mice were sacrificed and lungs were fixed and sectioned. Representative hematoxylin and eosin (H&E) stained lung histology focused on (A) focal clusters at 3 days and (D) granuloma formation at 4 weeks. Representative acid phosphatase activity in lung lesions showing activated macrophages at 3 days (B) and 4 weeks (E). Ziehl-Neelsen staining of lung lesions showing distribution of acid fast bacilli at 3 days (C) and 4 weeks (F). Magnifications were ×200. Granuloma formation is a crucial step in the mycobacterial containment and clearance. After 4 weeks of BCG infection, both wild-type and Ncf1 rescue mice had well differentiated granulomas containing multinucleated giant cells (Figures 7D–E). In these mice, granulomas enclosed the mycobacteria and virtually no mycobacteria were observed outside of granulomas (Figure 7F). In contrast, Ncf1 mutant mice presented large pyogranulomatous lesions with abundant neutrophil abscesses (Figure 7D) and diffusely distributed acid phosphatase-positive macrophages (Figure 7E). Importantly, no sequestration of mycobacteria was observed in Ncf1 mutant mice (Figure 7F). As seen for Ncf1 mutant mice, Cybb-deficient mice as well as Ncf1 mutant mice in a C57Bl/6 background showed larger granulomas without concise delimitations (Figure S4B). Disorganized granulomas with an abnormal presence of neutrophils were mainly in lung but there are also observed in the liver and spleen of Ncf1 mutant mice (data not shown). Thus, the presence of NADPH oxidase in mononuclear phagocytes is required for the formation of compact granulomas with concise delimitations and for sequestration of mycobacteria within granulomas.
Discussion
In this study, we have analyzed BCG infection in several mouse model of phagocyte NADPH oxidase deficiency. CGD mice were highly susceptible to BCG infection. Our results suggest that the phagocyte NADPH oxidase limits the severity of mycobacterial infection by at least two mechanisms: i) block of overshooting cytokine release; and ii) contribution to mycobacterial sequestration in granulomas. For these two mechanisms, NADPH oxidase function in macrophages was essential. We also observed a modest increase in bacterial load in mice lacking NOX2 function.
Role of macrophage NOX2 in mycobacterial infection
Particularly interesting in this respect is the recent discovery of a family with a peculiar variant of CGD [32]. These patients lack ROS production in macrophages, but not in neutrophils and showed a high sensitivity to mycobacterial infection, in particular to BCG. The Ncf1 mutant mice used in this study, including a selective rescue in mononuclear phagocytes, provide a mirror image of the patient study [31]: selective rescue of NOX2 in macrophages protected CGD mice against BCG infection. Indeed, most of the enhanced mycobacterial pathology associated with NOX2-deficiency (morbidity, mortality, enhanced cytokine production, abnormal granuloma formation) could be attributed to macrophages. There is one exception to this: the moderately increased mycobacterial load, which is not reversed by Ncf1 rescue in macrophages and hence was not correlated to the outcome of infection. Thus, while our results in mice show that selective rescue of NOX2 in macrophages restores resistance BCG infection; in the above mentioned CGD patients a selective loss of NOX2 in macrophages establishes high susceptibility.
Role CGD mutation and genetic background for the increased severity of BCG infection in the absence of the phagocyte NADPH oxidase
Hitherto, BCG infection has never been investigated in mouse models of CGD. However, infection of CGD mice with other types of mycobacteria led to discordant results: in some cases aggravation was observed, while in other studies no effect was observed. We wanted to assure that our results are not due to a specific choice of the CGD mutation or to the genetic background. We therefore tested two different CGD mutations (Ncf1, Cybb) as well as two different genetic backgrounds (C57/B10.Q, C57Bl/6). All results concur: CGD mice are highly susceptible to BCG infection.
Enhanced neutrophil infiltration in the absence of the phagocyte NADPH oxidase
Reconstitution of the phagocyte NADPH oxidase in mononuclear phagocytes completely reversed the neutrophil influx phenotype. Thus, it is not the lack of activity of NOX2 in neutrophils which leads to the increased number of neutrophils in inflammation. Most likely, NOX2 in mononuclear phagocytes regulates the number of invading neutrophils by controlling the release of neutrophil chemoattractants. These chemoattractants might be directly released from macrophages or possibly from other cells that depend on a macrophage signal. An alternative theory is the decreased uptake of apoptotic neutrophils by NADPH oxidase-deficient macrophages [39]. Enhanced neutrophil infiltration in CGD mice might be involved in the enhanced TNF production, thereby possibly contributing to the enhanced mortality in CGD mice.
Mycobacterial load in CGD mice
Despite enhanced levels of iNOS, our results show a small, increase of mycobacterial load in Ncf1 mutants. This suggests that the well-documented bactericidal activity of iNOS-dependent NO production is several impaired in the absence of NOX2, compatible with the suggested role of peroxynitrite (i.e. the reaction product of NO and superoxide) in mycobacterial killing. Note however that NADPH-oxidase involvement in killing of mycobacteria does not necessarily signify a direct antibacterial action. For example, mycobacteria have been suggested to be sensitive to neutrophil extracellular trap (NET) [40] and NADPH oxidase-dependent NET formation [41] could also be a relevant mechanism limiting the multiplication of mycobacteria.
Cytokine production in response to BCG infection
It has been suggested that the increased sensitivity of CGD patients to mycobacterial infection might be linked to a ROS activation of cytokine production, in particular IL-12 (which is secreted by macrophages to stimulate IFN-γ release by T lymphocytes [3]). In CGD patients, an hyperresponsiveness of neutrophils to different stimuli was usually observed [42]. In our study, we observed the opposite: CGD mice infected with BCG generated increased levels of cytokines. Interestingly, several of the cytokines increased in Ncf1 mutant mice (in particular TNFα, IL-12, IFN-γ, IL-17) are involved in the antimycobacterial defense. This might be a defense mechanism compensating for the lack of ROS generated by the NADPH oxidase. However, the high level of certain cytokines, in particular TNF, in CGD mice might also account for the high early mortality and absence of resolution of inflammation to mycobacterial infections.
Macrophage NOX2 and granuloma formation
Our results shed new light on granuloma formation in mycobacterial infection and the role of NOX2 in this process:
-
Within mycobacteria-induced granulomas there is an oxidative environment, which is completely abolished in Ncf1 mutant mice demonstrating that NOX2 is the source of oxidative stress. Rescue of functional NOX2 in mononuclear cells was sufficient to restore the oxidative environment within the granulomas.
-
The absence of macrophage NOX2 leads to morphologically altered granulomas. BCG-induced granulomas in Ncf1 mutant mice were larger, but of atypical appearance: acidophilic centers were not detectable; numerous neutrophils were infiltrated; and the delimitation of granuloma boarders was barely perceivable. At early time points, macrophage clusters, presumably the earliest signs of granuloma formation, were detected in wild-type and rescue, but not in Ncf1 mutant mice.
-
Ncf1 mutant granulomas are not able to maintain BCG. Indeed, while large, concentrated clusters of mycobacteria were readily detected in wild-type and in rescue mice, the bacteria were widely distributed throughout the tissue in Ncf1 mutant mice. Thus, while -at least at later time points - the allover mycobacterial load was not different between Ncf1 mutant and rescue mice, their tissue distribution was fundamentally altered.
-
The dysregulated CCL5 and TNF levels might contribute to the disturbed granuloma formation. The increased TNF levels might possibly even be a consequence of the neutrophil microabscesses within CGD granulomas.
Taken together, our results provide strong evidence for a role of NADPH oxidase-dependent ROS generation in the fine tuning of granuloma formation. Thus, redox-sensitive signaling steps are involved in the coordinated genesis of granulomas, and the overshooting cytokine and chemokine productions observed in CGD mice probably destabilizes granulomas.
To which extend do results obtained in our study apply to CGD patients? Clearly, our analysis of the published literature demonstrates that, human CGD patients are sensitive to infection with the vaccinal BCG strain [6], [8]. Approximately 15% of CGD patient with BCG disease will develop a disseminated form, also referred to as BCGosis. At this point, it is not clear which are the factors precipitating such disseminated disease. Genetic modifiers, type of BCG strain, inoculum size of viable mycobacteria are among the possible culprits. Similar as observed in our mouse model of disseminated BCG infection, there was a substantial mortality associated with BCGosis in CGD patients.
Taken together, the results presented here not only shed new light on BCG infection in CGD, but also provide first evidence for a role of the macrophage NADPH oxidase in the coordination of granuloma formation. The vaccinal BCG strain is an important tool for the control of childhood tuberculosis in countries with a high incidence of the disease. In general, children are vaccinated at birth, because the major effect of BCG vaccination is prevention from tuberculous meningitis early in life. Thus, the vaccination occurs prior to first manifestations of immune deficiency. New algorithms need to be defined to assure vaccine protection of immunocompetent neonates, without putting immunodeficient neonates at risk.
Materials and Methods
Ethics statement
Animal experiments complied with ethical standards of the University of Geneva and the Cantonal Veterinary Office (Authorization No. 1005/3715/2). Handling and manipulation of the animals complied with European Community guidelines.
Mice
Wild-type B10.Q, Ncf1 mutant and rescue mice, backcrossed into identical background were used (for details of backcross see [31], [43]). Ncf1 rescue mice are Ncf1 mutant animals which contain a transgenic wild-type Ncf1 gene under the control of a human CD68 promoter fragment. Ncf1 mutant with the same mutation on a C57Bl/6N background and its respective wild-type controls were used. Cybb-deficient mice and respective controls were backcrossed on C57Bl/6 background (Jackson Laboratories). For all experiments, mice aged 8–12 weeks were kept in a quiet room at 25°C with a 12 h light/dark cycle and food and water were supplied ad libitum.
Experimental infection
Mice were infected intravenously with 107 living CFU of M. bovis BCG Connaught [44], [45]. Mortality and body weights were monitored during infection. Three days and 4 weeks post-infection, mice were sacrificed and lung, liver and spleen were weighted, fixed and frozen for subsequent analyses.
Determination of colony forming units (CFU) from infected organs
The number of viable bacteria recovered from frozen organs was evaluated as previously described [46], [47].
Isolation and culture of primary macrophages and dendritic cells
Bone marrow primary cells were obtained from mice by flushing both the femur and the tibia as previously described [29], [48]
ROS evaluation
BMDMs and BMDCs were stimulated with BCG (MOI 10). The production of ROS by NOX2 was measured using Amplex red (Invitrogen) fluorescence, as described previously [49].
iNOS and nitrotyrosine quantifications
Lung homogenates were prepared and western blot performed as previously described [50]. Nitrotyrosine, a stable end product of peroxynitrite oxidation, was assessed in serum by enzyme-linked immunosorbent assay (ELISA; Hycult biotechnology, Netherlands).
Histological analyses and acid phosphatase activity
Histologic analyses of lung lesions were performed at 3 days and 4 weeks after infection. Lungs embedded in paraffin for hematoxylin/eosin (HE) and Ziehl-Neelsen stainings. For acid phosphatase staining, cryostat tissue sections from lung frozen in liquid nitrogen were used as previously described [51]. Signs of ROS production were evaluated by 8-hydroxy-2′-deoxyguanosine (8-OHdG) staining (1∶50, JaICA, Shizuoka, Japan) as previously described [52].
Evaluation of free alveolar space versus occupied space
Evaluation of the histopathology was performed on three lung lobe sections per animal (n = 4/group). Lung sections were captured on Zeiss Mirax Scan microscope system. Virtual sections were subdivided and images covering lobe sections corresponding to a surface of 21.50±8.05 mm2 per mouse, were proceeded for quantification of free space and occupied lung tissue using a specific program designed in the Metamorph software identifying cellularity, hematoxilin-eosin stain and air spaces [53].
Ex-vivo recall responses of spleen cells and release of nitric oxide
Mice were infected with BCG, sacrificed at day 17 and spleen cells were prepared as previously described [45]. Cells were stimulated with either medium alone, living BCG (103 CFU/well), or BCG culture protein extracts (17 µg/ml). After one, three and six days of treatment, medium was harvested for nitrite and TNF determination. Nitrite accumulation, as an indicator of NO production, was evaluated by Griess reagent (1% sulfanilamide and 0.1% naphtylethylenediamide in 2.5% phosphoric acid). TNF was determined in cell supernatants as described below.
Evaluation of cytokines in lung homogenates
Lungs were collected at different time points after BCG injection and tissue homogenate was prepared [54]. Cytokines and chemokines were measured by ELISA (Ready&D System).
Literature research
Literature research on CGD and mycobacterial infections was done from PubMed and Google Scholar with no limitations in time.
Statistics
Parametric (t -tests) and non-parametric (One-way analysis and Kruskal–Wallis) tests were used. In the case of multiple comparisons, a two-way ANOVA test with Bonferroni correction was used.
Supporting Information
Zdroje
1. AndersenP, DohertyTM (2005) The success and failure of BCG - implications for a novel tuberculosis vaccine. Nat Rev Microbiol 3 : 656–662.
2. KeijsersRR, BovenschenHJ, SeygerMM (2011) Cutaneous complication after BCG vaccination: case report and review of the literature. J Dermatolog Treat 22 : 315–318.
3. BustamanteJ, PicardC, Boisson-DupuisS, AbelL, CasanovaJL (2011) Genetic lessons learned from X-linked Mendelian susceptibility to mycobacterial diseases. Ann N Y Acad Sci 1246 : 92–101.
4. van der MeijdenAP, SteerenbergPA, de JongWH, DebruyneFM (1991) Intravesical Bacillus Calmette-Guerin treatment for superficial bladder cancer: results after 15 years of experience. Anticancer research 11 : 1253–1258.
5. StegA, LeleuC, DebreB, Boccon-GibodL, SicardD (1989) Systemic bacillus Calmette-Guerin infection, ‘BCGitis’, in patients treated by intravesical bacillus Calmette-Guerin therapy for bladder cancer. Eur Urol 16 : 161–164.
6. BustamanteJ, AksuG, VogtG, de BeaucoudreyL, GenelF, et al. (2007) BCG-osis and tuberculosis in a child with chronic granulomatous disease. J Allergy Clin Immunol 120 : 32–38.
7. LiHM, ZhaoSY, HeJX, JiangZF (2010) [Clinical analysis of 18 children with disseminated Bacille Calmette-Guerin infection]. Zhonghua Er Ke Za Zhi 48 : 65–68.
8. YingWJ, WangXC, SunJQ, LiuDR, YuYH, et al. (2012) [Clinical features of chronic granulomatous disease]. Zhonghua Er Ke Za Zhi 50 : 380–385.
9. NorouziS, AghamohammadiA, MamishiS, RosenzweigSD, RezaeiN (2012) Bacillus Calmette-Guerin (BCG) complications associated with primary immunodeficiency diseases. J Infect 64 : 543–554.
10. FattahiF, BadalzadehM, SedighipourL, MovahediM, FazlollahiMR, et al. (2011) Inheritance pattern and clinical aspects of 93 Iranian patients with chronic granulomatous disease. J Clin Immunol 31 : 792–801.
11. BedardK, KrauseKH (2007) The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev 87 : 245–313.
12. SchappiM, DeffertC, FietteL, GavazziG, HerrmannF, et al. (2008) Branched fungal beta-glucan causes hyperinflammation and necrosis in phagocyte NADPH oxidase-deficient mice. J Pathol 214 : 434–444.
13. NathanC, ShilohMU (2000) Reactive oxygen and nitrogen intermediates in the relationship between mammalian hosts and microbial pathogens. Proc Natl Acad Sci U S A 97 : 8841–8848.
14. DeffertC, CachatJ, KrauseKH (2014) Phagocyte NADPH oxidase, chronic granulomatous disease and mycobacterial infections. Cell Microbiol 16 : 1168–1178.
15. Garcia I, Olleros ML (2009) The roles of tumor necrosis factor and other macrophage-derived cytokines in host defense mechanisms during the course of Mycobacterium tuberculosis infection. In: Current Topics on the Profiles of Host Immunological Response to Mycobacterial Infections pp. 1–46.
16. GarciaI, OllerosML, QuesniauxVF, JacobsM, AllieN, et al. (2011) Roles of soluble and membrane TNF and related ligands in mycobacterial infections: effects of selective and non-selective TNF inhibitors during infection. Adv Exp Med Biol 691 : 187–201.
17. LoweDM, RedfordPS, WilkinsonRJ, O'GarraA, MartineauAR (2012) Neutrophils in tuberculosis: friend or foe? Trends Immunol 33 : 14–25.
18. BustamanteJ, AriasAA, VogtG, PicardC, GaliciaLB, et al. (2011) Germline CYBB mutations that selectively affect macrophages in kindreds with X-linked predisposition to tuberculous mycobacterial disease. Nat Immunol 12 : 213–221.
19. KokerMY, CamciogluY, van LeeuwenK, KilicSS, BarlanI, et al. (2013) Clinical, functional, and genetic characterization of chronic granulomatous disease in 89 Turkish patients. J Allergy Clin Immunol 132 : 1156–1163 e1155.
20. LeeWI, HuangJL, YehKW, JaingTH, LinTY, et al. (2011) Immune defects in active mycobacterial diseases in patients with primary immunodeficiency diseases (PIDs). J Formos Med Assoc 110 : 750–758.
21. LinCJ, WangSC, KuCL, KaoJK, ChenM, et al. (2013) Successful Unrelated Cord Blood Stem Cell Transplantation in an X-linked Chronic Granulomatous Disease Patient with Disseminated BCG-induced Infection. Pediatr Neonatol DOI: 10.1016/j.pedneo.2013.04.001
22. KhotaeiG, Hirbod-MobarakehA, AmirkashaniD, ManafiF, RezaeiN (2012) Mycobacterium tuberculosis meningitis as the first presentation of chronic granulomatous disease. Braz J Infect Dis 16 : 491–492.
23. NaidooR, JordaanN, ChanKW, Le RouxDM, PienaarS, et al. (2011) A novel CYBB mutation with the first genetically confirmed case of chronic granulomatous disease in South Africa. S Afr Med J 101 : 768–769.
24. Afshar PaimanS, SiadatiA, MamishiS, TabatabaieP, KhotaeeG (2006) Disseminated Mycobacterium bovis infection after BCG vaccination. Iran J Allergy Asthma Immunol 5 : 133–137.
25. LeePP, ChanKW, JiangL, ChenT, LiC, et al. (2008) Susceptibility to mycobacterial infections in children with X-linked chronic granulomatous disease: a review of 17 patients living in a region endemic for tuberculosis. Pediatr Infect Dis J 27 : 224–230.
26. Sadeghi-ShanbestariM, AnsarinK, MaljaeiSH, RafeeyM, PezeshkiZ, et al. (2009) Immunologic aspects of patients with disseminated bacille Calmette-Guerin disease in north-west of Iran. Ital J Pediatr 35 : 42.
27. KusuharaK, OhgaS, HoshinaT, SaitoM, SasakiY, et al. (2009) Disseminated Bacillus Calmette-Guerin lymphadenitis in a patient with gp91phox - chronic granulomatous disease 25 years after vaccination. Eur J Pediatr 168 : 745–747.
28. MovahediZ, NorouziS, MamishiS, RezaeiN (2011) BCGiosis as a presenting feature of a child with chronic granulomatous disease. Braz J Infect Dis 15 : 83–86.
29. DeffertC, CarnesecchiS, YuanH, RougemontAL, KelkkaT, et al. (2012) Hyperinflammation of chronic granulomatous disease is abolished by NOX2 reconstitution in macrophages and dendritic cells. J Pathol 228 : 341–350.
30. SareilaO, JaakkolaN, OlofssonP, KelkkaT, HolmdahlR (2013) Identification of a region in p47phox/NCF1 crucial for phagocytic NADPH oxidase (NOX2) activation. J Leukoc Biol 93 : 427–435.
31. GeldermanKA, HultqvistM, PizzollaA, ZhaoM, NandakumarKS, et al. (2007) Macrophages suppress T cell responses and arthritis development in mice by producing reactive oxygen species. J Clin Invest 117 : 3020–3028.
32. PizzollaA, HultqvistM, NilsonB, GrimmMJ, EneljungT, et al. (2012) Reactive oxygen species produced by the NADPH oxidase 2 complex in monocytes protect mice from bacterial infections. J Immunol 188 : 5003–5011.
33. MorgensternDE, GiffordMA, LiLL, DoerschukCM, DinauerMC (1997) Absence of respiratory burst in X-linked chronic granulomatous disease mice leads to abnormalities in both host defense and inflammatory response to Aspergillus fumigatus. J Exp Med 185 : 207–218.
34. GarciaI, GulerR, VesinD, OllerosML, VassalliP, et al. (2000) Lethal Mycobacterium bovis Bacillus Calmette Guerin infection in nitric oxide synthase 2-deficient mice: cell-mediated immunity requires nitric oxide synthase 2. Lab Invest 80 : 1385–1397.
35. PacherP, BeckmanJS, LiaudetL (2007) Nitric oxide and peroxynitrite in health and disease. Physiol Rev 87 : 315–424.
36. ChtanovaT, SchaefferM, HanSJ, van DoorenGG, NollmannM, et al. (2008) Dynamics of neutrophil migration in lymph nodes during infection. Immunity 29 : 487–496.
37. VesoskyB, RottinghausEK, StrombergP, TurnerJ, BeamerG (2010) CCL5 participates in early protection against Mycobacterium tuberculosis. J Leukoc Biol 87 : 1153–1165.
38. BreenAP, MurphyJA (1995) Reactions of oxyl radicals with DNA. Free Radic Biol Med 18 : 1033–1077.
39. SanmunD, WitaspE, JitkaewS, TyurinaYY, KaganVE, et al. (2009) Involvement of a functional NADPH oxidase in neutrophils and macrophages during programmed cell clearance: implications for chronic granulomatous disease. Am J Physiol Cell Physiol 297: C621–631.
40. von Kockritz-BlickwedeM, NizetV (2009) Innate immunity turned inside-out: antimicrobial defense by phagocyte extracellular traps. J Mol Med (Berl) 87 : 775–783.
41. BianchiM, NiemiecMJ, SilerU, UrbanCF, ReichenbachJ (2011) Restoration of anti-Aspergillus defense by neutrophil extracellular traps in human chronic granulomatous disease after gene therapy is calprotectin-dependent. J Allergy Clin Immunol 127 : 1243–1252 e1247.
42. HatanakaE, CarvalhoBT, Condino-NetoA, CampaA (2004) Hyperresponsiveness of neutrophils from gp 91phox deficient patients to lipopolysaccharide and serum amyloid A. Immunol Lett 94 : 43–46.
43. HultqvistM, OlofssonP, HolmbergJ, BackstromBT, TordssonJ, et al. (2004) Enhanced autoimmunity, arthritis, and encephalomyelitis in mice with a reduced oxidative burst due to a mutation in the Ncf1 gene. Proc Natl Acad Sci U S A 101 : 12646–12651.
44. HanusM, MatouskovaM, VernerP, HyrslL (1994) Immunotherapy of superficial bladder tumors: preliminary results with ImmuCyst–BCG Connaught, Toronto. Neoplasma 41 : 25–27.
45. OllerosML, VesinD, BisigR, Santiago-RaberML, Schuepbach-MallepellS, et al. (2012) Membrane-bound TNF induces protective immune responses to M. bovis BCG infection: regulation of memTNF and TNF receptors comparing two memTNF molecules. PLoS One 7: e31469.
46. OllerosML, GulerR, CorazzaN, VesinD, EugsterHP, et al. (2002) Transmembrane TNF induces an efficient cell-mediated immunity and resistance to Mycobacterium bovis bacillus Calmette-Guerin infection in the absence of secreted TNF and lymphotoxin-alpha. J Immunol 168 : 3394–3401.
47. OllerosML, GulerR, VesinD, ParapanovR, MarchalG, et al. (2005) Contribution of transmembrane tumor necrosis factor to host defense against Mycobacterium bovis bacillus Calmette-guerin and Mycobacterium tuberculosis infections. Am J Pathol 166 : 1109–1120.
48. FotioAL, OllerosML, VesinD, TauzinS, BisigR, et al. (2010) In vitro inhibition of lipopolysaccharide and mycobacterium bovis bacillus Calmette Guerin-induced inflammatory cytokines and in vivo protection from D-galactosamine/LPS -mediated liver injury by the medicinal plant Sclerocarya birrea. Int J Immunopathol Pharmacol 23 : 61–72.
49. BedardK, AttarH, BonnefontJ, JaquetV, BorelC, et al. (2009) Three common polymorphisms in the CYBA gene form a haplotype associated with decreased ROS generation. Hum Mutat 30 : 1123–1133.
50. GulerR, OllerosML, VesinD, ParapanovR, VesinC, et al. (2004) Inhibition of inducible nitric oxide synthase protects against liver injury induced by mycobacterial infection and endotoxins. J Hepatol 41 : 773–781.
51. GulerR, OllerosML, VesinD, ParapanovR, GarciaI (2005) Differential effects of total and partial neutralization of tumor necrosis factor on cell-mediated immunity to Mycobacterium bovis BCG infection. Infect Immun 73 : 3668–3676.
52. SchiavoneS, SorceS, Dubois-DauphinM, JaquetV, ColaiannaM, et al. (2009) Involvement of NOX2 in the development of behavioral and pathologic alterations in isolated rats. Biol Psychiatry 66 : 384–392.
53. VigneS, PalmerG, MartinP, LamacchiaC, StrebelD, et al. (2012) IL-36 signaling amplifies Th1 responses by enhancing proliferation and Th1 polarization of naive CD4+ T cells. Blood 120 : 3478–3487.
54. DeffertC, OllerosML, HuipingY, HerrmannFR, ZekryD, et al. (2011) TNF-alpha blockade in chronic granulomatous disease-induced hyperinflammation: patient analysis and murine model. J Allergy Clin Immunol 128 : 675–677.
Štítky
Hygiena a epidemiológia Infekčné lekárstvo Laboratórium
Článek Out-of-Sequence Signal 3 as a Mechanism for Virus-Induced Immune Suppression of CD8 T Cell ResponsesČlánek RNF26 Temporally Regulates Virus-Triggered Type I Interferon Induction by Two Distinct MechanismsČlánek Mouse, but Not Human, ApoB-100 Lipoprotein Cholesterol Is a Potent Innate Inhibitor of Pneumolysin
Článok vyšiel v časopisePLOS Pathogens
Najčítanejšie tento týždeň
2014 Číslo 9- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Očkování proti virové hemoragické horečce Ebola experimentální vakcínou rVSVDG-ZEBOV-GP
- Koronavirus hýbe světem: Víte jak se chránit a jak postupovat v případě podezření?
-
Všetky články tohto čísla
- Virus Control Goes Epigenetic
- The Role of Iron in Prion Disease and Other Neurodegenerative Diseases
- The Ins and Outs of Rust Haustoria
- Prion Strains and Amyloid Polymorphism Influence Phenotypic Variation
- Teaching Fido New ModiFICation Tricks
- Can Enhance Infection in Mosquitoes: Implications for Malaria Control?
- MIF Contributes to Associated Immunopathogenicity Development
- Persistence of Virus Reservoirs in ART-Treated SHIV-Infected Rhesus Macaques after Autologous Hematopoietic Stem Cell Transplant
- Bacillus Calmette-Guerin Infection in NADPH Oxidase Deficiency: Defective Mycobacterial Sequestration and Granuloma Formation
- EhCoactosin Stabilizes Actin Filaments in the Protist Parasite
- Molecular Insights Into the Evolutionary Pathway of O1 Atypical El Tor Variants
- LprG-Mediated Surface Expression of Lipoarabinomannan Is Essential for Virulence of
- Structural Correlates of Rotavirus Cell Entry
- Multivalent Adhesion Molecule 7 Clusters Act as Signaling Platform for Host Cellular GTPase Activation and Facilitate Epithelial Barrier Dysfunction
- The Effects of Vaccination and Immunity on Bacterial Infection Dynamics
- Myeloid Derived Hypoxia Inducible Factor 1-alpha Is Required for Protection against Pulmonary Infection
- Functional Characterisation of Germinant Receptors in and Presents Novel Insights into Spore Germination Systems
- Global Analysis of Neutrophil Responses to Reveals a Self-Propagating Inflammatory Program
- Host Cell Invasion by Apicomplexan Parasites: The Junction Conundrum
- Comparative Phenotypic Analysis of the Major Fungal Pathogens and
- Unravelling the Multiple Functions of the Architecturally Intricate β-galactosidase, BgaA
- Sialylation of Prion Protein Controls the Rate of Prion Amplification, the Cross-Species Barrier, the Ratio of PrP Glycoform and Prion Infectivity
- Symbionts Commonly Provide Broad Spectrum Resistance to Viruses in Insects: A Comparative Analysis of Strains
- Ontogeny of Recognition Specificity and Functionality for the Broadly Neutralizing Anti-HIV Antibody 4E10
- Identification and Characterisation of a Hyper-Variable Apoplastic Effector Gene Family of the Potato Cyst Nematodes
- Crimean-Congo Hemorrhagic Fever Virus Entry into Host Cells Occurs through the Multivesicular Body and Requires ESCRT Regulators
- Age-Dependent Enterocyte Invasion and Microcolony Formation by
- CD160-Associated CD8 T-Cell Functional Impairment Is Independent of PD-1 Expression
- Functional Fluorescent Protein Insertions in Herpes Simplex Virus gB Report on gB Conformation before and after Execution of Membrane Fusion
- The Tudor Domain Protein Spindlin1 Is Involved in Intrinsic Antiviral Defense against Incoming Hepatitis B Virus and Herpes Simplex Virus Type 1
- Transgenic Analysis of the MAP Kinase MPK10 Reveals an Auto-inhibitory Mechanism Crucial for Stage-Regulated Activity and Parasite Viability
- Evidence for a Transketolase-Mediated Metabolic Checkpoint Governing Biotrophic Growth in Rice Cells by the Blast Fungus
- Incomplete Deletion of IL-4Rα by LysM Reveals Distinct Subsets of M2 Macrophages Controlling Inflammation and Fibrosis in Chronic Schistosomiasis
- Identification and Functional Expression of a Glutamate- and Avermectin-Gated Chloride Channel from , a Southern Hemisphere Sea Louse Affecting Farmed Fish
- Out-of-Sequence Signal 3 as a Mechanism for Virus-Induced Immune Suppression of CD8 T Cell Responses
- Strong Epistatic Selection on the RNA Secondary Structure of HIV
- Hematopoietic but Not Endothelial Cell MyD88 Contributes to Host Defense during Gram-negative Pneumonia Derived Sepsis
- Delineation of Interfaces on Human Alpha-Defensins Critical for Human Adenovirus and Human Papillomavirus Inhibition
- Exploitation of Reporter Strains to Probe the Impact of Vaccination at Sites of Infection
- RNF26 Temporally Regulates Virus-Triggered Type I Interferon Induction by Two Distinct Mechanisms
- Helminth Infections Coincident with Active Pulmonary Tuberculosis Inhibit Mono- and Multifunctional CD4 and CD8 T Cell Responses in a Process Dependent on IL-10
- MHC Class II Restricted Innate-Like Double Negative T Cells Contribute to Optimal Primary and Secondary Immunity to
- Reactive Oxygen Species Regulate Caspase-11 Expression and Activation of the Non-canonical NLRP3 Inflammasome during Enteric Pathogen Infection
- Evolution of Plastic Transmission Strategies in Avian Malaria
- A New Human 3D-Liver Model Unravels the Role of Galectins in Liver Infection by the Parasite
- Translocates into the Myocardium and Forms Unique Microlesions That Disrupt Cardiac Function
- Mouse, but Not Human, ApoB-100 Lipoprotein Cholesterol Is a Potent Innate Inhibitor of Pneumolysin
- The Cofilin Phosphatase Slingshot Homolog 1 (SSH1) Links NOD1 Signaling to Actin Remodeling
- Kaposi's Sarcoma Herpesvirus MicroRNAs Induce Metabolic Transformation of Infected Cells
- Reorganization of the Endosomal System in -Infected Cells: The Ultrastructure of -Induced Tubular Compartments
- Distinct Dictation of Japanese Encephalitis Virus-Induced Neuroinflammation and Lethality via Triggering TLR3 and TLR4 Signal Pathways
- Exploitation of the Complement System by Oncogenic Kaposi's Sarcoma-Associated Herpesvirus for Cell Survival and Persistent Infection
- The Secreted Peptide PIP1 Amplifies Immunity through Receptor-Like Kinase 7
- Structural Insight into Host Recognition by Aggregative Adherence Fimbriae of Enteroaggregative
- The CD14CD16 Inflammatory Monocyte Subset Displays Increased Mitochondrial Activity and Effector Function During Acute Malaria
- Infection Induces Expression of a Mosquito Salivary Protein (Agaphelin) That Targets Neutrophil Function and Inhibits Thrombosis without Impairing Hemostasis
- PLOS Pathogens
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- The Secreted Peptide PIP1 Amplifies Immunity through Receptor-Like Kinase 7
- Symbionts Commonly Provide Broad Spectrum Resistance to Viruses in Insects: A Comparative Analysis of Strains
- MIF Contributes to Associated Immunopathogenicity Development
- The Ins and Outs of Rust Haustoria
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



